Chapter 22
advertisement

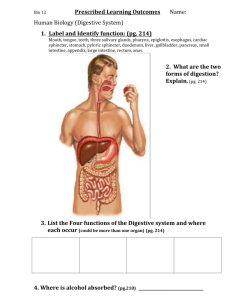
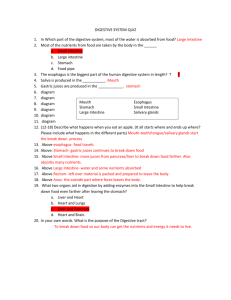
Chapter 24 The Digestive System The Alimentary Canal Accessory Digestive Organs Functions of Digestive System Ingestion - selective intake of food. Digestion – mechanical and chemical breakdown of food into a form the body can use. Absorption – uptake of nutrients into blood and lymph. Compaction – absorption of water and consolidation of wastes into fecal mass. Defecation – the elimination of the fecal mass. Alimentary canal [Gastrointestinal (GI) tract] Consists of: Mouth→ Pharynx→ Esophagus → Stomach→ Duodenum→ Jejunum → Ileum→ Caecum→ Colon (ascending, transverse, descending, sigmoid) → Rectum → Anus . GI tract is a tube that is actually outside of the body. Accessory Digestive Organs Teeth, salivary glands, pancreas, liver, gall bladder. The digestive system Histology of the Alimentary Canal Defined: Beginning at the esophagus and continuing through the alimentary canal to the anus, there are four basic layers or tunics.. Listed: from the inner-most to the outer-most layer. 1. mucosa – moist epithelial membrane; functions in secretion, absorption and protection against infection. This layer is more complex than the other tunics of the GI tract in that it has three sublayers. Three layers or linings of the mucosa: epithelial lining – simple columnar with goblet cells lamina propria – areolar CT (some reticular CT) muscularis mucosae – a thin layer of smooth muscle that helps move the mucosa. Secretes mucous, digestive enzymes & hormones and absorbs end products of digestion. Histology of the Alimentary Canal 2. submucosa – loose CT containing blood vessels, nerves (submucosal nerve plexus), lymph vessels. 3. muscularis externa – consists of an inner circular layer and an outer longitudinal layer of smooth muscle. These muscles are responsible for the peristalsis and segmentation of the GI tract and are controlled by the myenteric plexus (a group of nerves between the layers). Thickenings of this layer create the sphincters or valves that separate sections of the tract. 4. serosa – the same layer as the visceral peritoneum. Consists of areolar CT covered by a single layer of epithelial cells. Should be noted that the esophagus is somewhat different in that it is not covered by the visceral peritoneum. GI tract innervation Tongue, pharynx, and esophagus are innervated by CN V, VII, IX-XII regulate swallowing and mastication . Superior sympath. cervical gang. and CN VII and IX regulate salivary secretions. Both sympathetic and parasympathetic nerves regulate GI tract. Sympathetic stimulation causes ↓ in motility, ↓ in secretions and keep sphincters contracted. Parasympathetic ↑ motility, secretions and relaxes sphincters and promotes digestion. Enteric nervous system regulate GI function irrespective of PSym. or Sym. Input. It is located in the submucosa (Meissners plexus) and between 2 layers muscularis mucosa as myenteric (Auerbach’s plexus) Enteric nervous system - Auerbachs nerve plexus Monitor stretch Chem cond. Meissners plexus Vascular supply to GI Tract Above the diaphragm there are numerous branches off of the aorta and carotid arteries to the esophagus, pharynx, mouth etc. Below the diaphragm the celiac trunk supplies the stomach (gastric), spleen (splenic) and liver (hepatic) as well as superior and inferior mesenteric arteries. Vascular supply to GI Tract Vascular supply to GI Tract Hepatic portal veins Peritoneum and mesentery Peritoneum- serous membrane lining the abdominal cavity and most of the visceral organs Parietal peritoneum Visceral peritoneum Mesentery- is a double layer of peritoneum that extends from the abdominal wall to the digestive organs. It keeps the organs in place and allows for their active contractions to occur without the guts becoming twisted and entangled. Greater and lesser omentum; falciform ligament Serous membranes Lesser omentum Greater omentum Mesenteries The Mouth Initial point of entry of food into GI tract Is the first site for beginning the breakdown of food into its constituent molecules (lipids → fatty acids, carbohydrates → simple sugars & protieins → amino acids) for absorption into the body. Consists of: lips, cheeks, tongue, teeth, salivary glands, palate. Lined with a thick stratified squamous epithelium The mouth Tongue Muscular organ for manipulating and moving food in mouth and aid in swallowing of foods. Contains taste buds chemoreceptors The Palate Separates the mouth from the nasal cavity. Allows you to chew food while breathing Anterior portion is hard palate formed palatine process of mandible and palatine bones. Posterior portion is composed of mainly sk. m. Uvula hangs down from soft palate Teeth Adults: 32 total ( 8) incisors- blade shaped for clipping and cutting food (4) canines- conical with sharp ridgeline and pointed tip for tearing food ( 20) molars/premolars- flattened crowns for crushing and grinding food Each tooth is embedded in a socket = alveolus Teeth Adults=32 Children =20 Salivary glands Parotid-serous/watery Sublingual-serous and mucous Submandibular- serous and mucous The Pharynx Three regions defined by location and function: Nasopharynx- air passage way only: composed of pseudostratified ciliated columnar epithelium Oropharynx- back of oral cavity down to epiglottis: -composed of stratified squamous epithelium. Laryngopharynx- air passageway, food is deflected into esophagus and does not enter this region -composed of stratified squamous epithelium - Esophagus Defined/Location: straight muscular tube ~ 10” long extends from laryngopharynx to stomach. Histology: mucosa – nonkeratinized stratified squamous epithelium with mucous glands muscularis externa – consists of circular and longitudinal layers of skeletal muscle and smooth muscle: (upper 1/3 is sk.m.; mid 1/3 is sk/sm. m; and lower 1/3 is all sm.m.) fibrous adventitia that blends with surrounding tissues Esophagus Lower esophageal sphincter is a physiologic control valve that opens to release food into stomach, but constricts to prevent gastric regurgitation into esophagus. Movement of food is by segmentation = peristalsis Courses through the thorax posterior to trachea and penetrates diaphragm at esophageal hiatus. Peristaltic movement Food moves as a bolus in segmented manner with alternate segments of esophagus contracting then relaxing to move food downward. Esophagus X-section The Stomach Defined: Temporary storage tank where chemical breakdown of proteins begins and a creamy paste “chyme” is formed. pH~ 1-2. Location-Lies in upper left quadrant of abdominal cavity, inferior to diaphragm and partially covered by the liver. Histology: Lined with simple columnar epithelium and numerous gastric glands Four regions: Cardia Fundus Body Pyloric Stomach Size: Varies from 15 to 25 cm. (6-10”) in length. empty has a volume of ~ 50 ml; full capacity ~ 4 l. empty it collapses onto itself and throws its mucosa and submucosa into longitudinal folds called “rugae” Three layers of smooth muscle: Longitudinal Circular Oblique Pyloric region joins the duodenum at pyloric sphincter. Cross section of rugae and stomach wall Small Intestine Three sections: Duodenum, Jejunum, and Ileum Duodenum: shortest (~ 10”) and widest; buffers low pH of chyme. First 2” is intraperitoneal, remainder is retroperitoneal. Contains Plicae circularis = circular folds → spiraling of chyme Jejunum : ~8’ long; bulk of digestion and absorption occurs here. Ileum : ~ 12’ long; controls movement of mass into caecum of large intestine Peyer’s Patches- aggregated lymphoid follicles near ileum; increase in abundance as you get nearer large intestine Joins large intestine at ileocecal junction (ileocecal valve) Histology of Small Intestine mucosa –simple columnar epithelium with absorptive cells bound by tight junctions and numerous mucussecreting goblet cells. microvilli –tiny projections of plasma membrane (brushed border) contain enzymes that complete final stages of CHO and protein digestion 3-D view of small intestinal Microvilli - note the lacteal within the core of the microvilli Route of absorbed nutrients Plicae circularis in Jejunum plicae circularis – deep permanent folds of mucosa and submucosa of duodenum and jejunum; force chyme to spiral through the intestinal lumen; slows movement and increases absorptive surface area Large Intestine divisions of: Begins at caecum, a blind pouch with appendix attached and ends at anal canal. Ascending colon: proceeds upward on right side after anastomosing with ileum at ileocecal junction. (Retroperitoneal) Transverse colon: curves medially at right colic flexure and crosses over superior part of abdominal cavity. Descending colon: begins at left colic flexure off of transverse colon and descends the left side of abdomen until it reaches the iliac fossa to join sigmoid. (retroperitoneal) Large intestine diameter is greater than small intestine length is only 1.5 m (5.5 ft) vs 6 m for small intestine Large Intestine divisions in pelvic cavity Sigmoid colon: S-shaped segment starts at iliac fossa and travels behind bladder to empty into the rectum (retroperitoneal). Rectum: ~ 15” long expandable end portion of L.I. at level of S3 and is for temporary storage of fecal material . Rectal mocosa is smoother than colon; Has three rectal folds (rectal valves) that enable it to pass gas (flatulence) without releasing fecal matter. Upon fecal matter entering rectum it triggers the defecation reflex to expel fecal matter from rectum. Large Intestine divisions in pelvic cavity Anal canal: Final portion of L.I. before excreting fecal matter out of anal opening. Mucosa of anal canal contains longitudinal columns called anal columns with depressions called anal sinuses between the columns. As feces passes through anal canal they press against the sinuses causing them to release more mucous to lubricate the canal during defecation. Anal sphincters internal and external Internal sphincter is smooth muscle of muscularis externa External sphincter is skeletal muscle Anal Canal Large intestine Large intestine absorbs mostly water from fecal mass. Lacks villi and has relatively thin wall. Interior wall is relatively smooth mucosa – contains numerous goblet cells which produce copious amounts of mucus to lubricate the fecal mass. lymphoid nodules (Peyers’ patches) extend in submucosa. Large intestine Muscularis externa layer is reduced in thickness Wall contains: - - Tenia coli- small bands of longitudinal muscle occurring just beneath submucosa. Tenia coli contract and pull Large Intestine longitudinally to form bulges called haustra. - Haustra- pocket like sacs along L.I.; result in segmentation of L.I. Churning action occurs here which turns fecal material into a sludgy paste. Large intestine histology Liver Largest gland in the body. Redish brown and located in upper right quadrant of abdomen. Multiple functions only 1 of which has to do with digestion, manufactures bile for breakdown of fats which are then acted upon by pancreatic lipases. Consists of 4 lobes: right, left, caudate and quadrate. Contains gall bladder = storage bag for bile. Liver Falciform ligament separates right lobe from left lobe anchors liver to anterior wall of abdomen. Caudate and quadrate lobes are visible from posterior only. Gall bladder is lateral to quadrate lobe Porta hepatis is where vessels and nerves enter liver. Liver anterior view Liver posterior view Liver histology The liver is composed of millions of hexagonal lobules about the size of a sesame seed and made up of hepatocytes. Lobule has a central vein in middle and at each corner a portal triad (arteriole, venule and bile duct) Gall Bladder Storage bag (~ 10 cm long) for bile produced by liver Bile enters gall bladder via left and right hepatic ducts which empty into common hepatic duct → cystic duct → gall bladder for storage. Bile leaves gall bladder via cystic duct and joins pancreatic duct to form hepatopancreatic ampulla before it empties into duodenum. Release is controlled by hepatopancreatic sphincter of “Oddi” Bile salts act as detergents in breaking down fats in small intestine. Pancreas Tucked under stomach and liver in a bend of the duodenum has a lobulated appearance. Consists of a head, body, and a tail. Combination endocrine and exocrine gland. Functions as an endocrine and digestive organ Endocrine pancreatic islets → insulin and glucagon → regulation of blood glucose Exocrine → pancreatic enzymes and zymogens that aid in digestion. Pancreatic juices are very alkaline and neutralize acidic chyme coming from stomach when released into duodenum. Pancreas