checkpt 6 study guide
advertisement
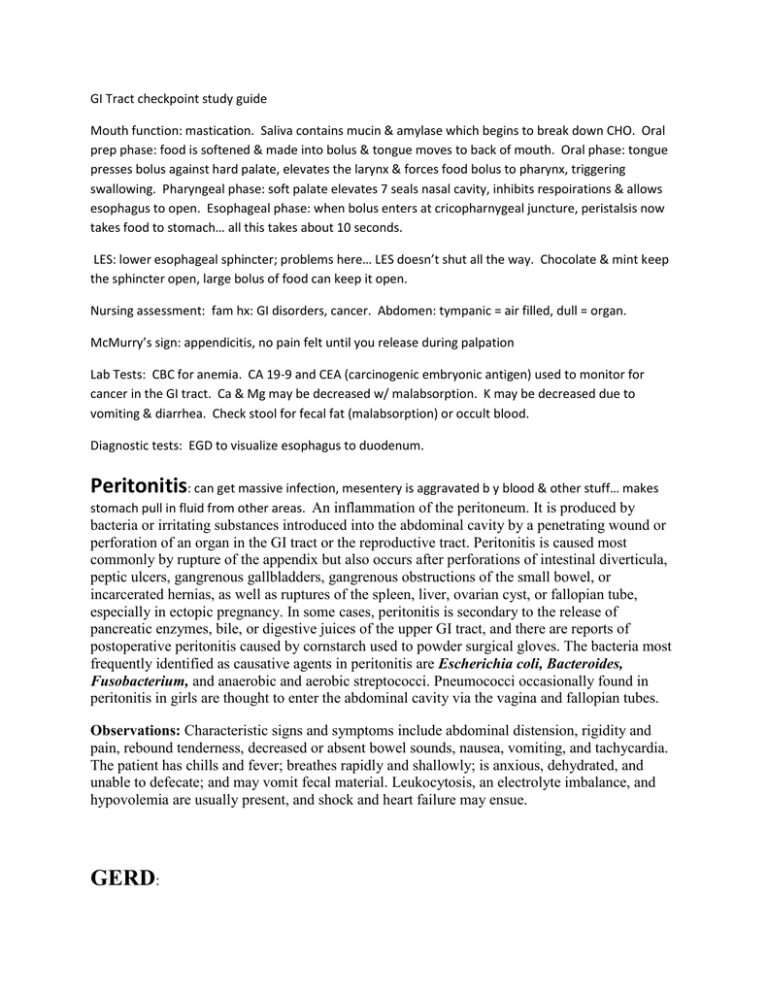
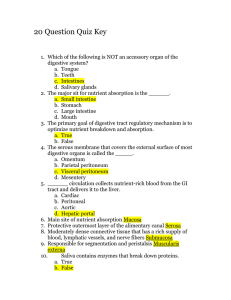
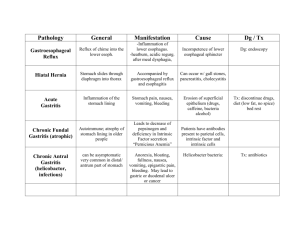
GI Tract checkpoint study guide Mouth function: mastication. Saliva contains mucin & amylase which begins to break down CHO. Oral prep phase: food is softened & made into bolus & tongue moves to back of mouth. Oral phase: tongue presses bolus against hard palate, elevates the larynx & forces food bolus to pharynx, triggering swallowing. Pharyngeal phase: soft palate elevates 7 seals nasal cavity, inhibits respoirations & allows esophagus to open. Esophageal phase: when bolus enters at cricopharnygeal juncture, peristalsis now takes food to stomach… all this takes about 10 seconds. LES: lower esophageal sphincter; problems here… LES doesn’t shut all the way. Chocolate & mint keep the sphincter open, large bolus of food can keep it open. Nursing assessment: fam hx: GI disorders, cancer. Abdomen: tympanic = air filled, dull = organ. McMurry’s sign: appendicitis, no pain felt until you release during palpation Lab Tests: CBC for anemia. CA 19-9 and CEA (carcinogenic embryonic antigen) used to monitor for cancer in the GI tract. Ca & Mg may be decreased w/ malabsorption. K may be decreased due to vomiting & diarrhea. Check stool for fecal fat (malabsorption) or occult blood. Diagnostic tests: EGD to visualize esophagus to duodenum. Peritonitis: can get massive infection, mesentery is aggravated b y blood & other stuff… makes stomach pull in fluid from other areas. An inflammation of the peritoneum. It is produced by bacteria or irritating substances introduced into the abdominal cavity by a penetrating wound or perforation of an organ in the GI tract or the reproductive tract. Peritonitis is caused most commonly by rupture of the appendix but also occurs after perforations of intestinal diverticula, peptic ulcers, gangrenous gallbladders, gangrenous obstructions of the small bowel, or incarcerated hernias, as well as ruptures of the spleen, liver, ovarian cyst, or fallopian tube, especially in ectopic pregnancy. In some cases, peritonitis is secondary to the release of pancreatic enzymes, bile, or digestive juices of the upper GI tract, and there are reports of postoperative peritonitis caused by cornstarch used to powder surgical gloves. The bacteria most frequently identified as causative agents in peritonitis are Escherichia coli, Bacteroides, Fusobacterium, and anaerobic and aerobic streptococci. Pneumococci occasionally found in peritonitis in girls are thought to enter the abdominal cavity via the vagina and fallopian tubes. Observations: Characteristic signs and symptoms include abdominal distension, rigidity and pain, rebound tenderness, decreased or absent bowel sounds, nausea, vomiting, and tachycardia. The patient has chills and fever; breathes rapidly and shallowly; is anxious, dehydrated, and unable to defecate; and may vomit fecal material. Leukocytosis, an electrolyte imbalance, and hypovolemia are usually present, and shock and heart failure may ensue. GERD: Meds: Protonix, prilosec & nexium: proton pump inhibitors: an agent that inhibits gastric acid secretion by blocking the action of hydrogen ions, potassium ions, and adenosine triphosphatase at the secretory surface of gastric parietal cells. (generics end in “zole” ) H2 (histamine) blockers: zantac, axid & pepsid: an agent that blocks the action of histamine by competitive binding to the H2 receptor. It is used to inhibit gastric secretion in the treatment of peptic ulcer. (names of generic end in “dine” ) Antacid: (malox, gaviscon) a drug or dietary substance that buffers, neutralizes, or absorbs hydrochloric acid in the stomach. Nonsystemic antacids containing aluminum and calcium are constipating; those containing magnesium have a laxative effect. Systemic antacids such as sodium bicarbonate are rarely used. (prong pH level up) Reglan: if rapid emptying of the stomach is needed, metoclopramide (Reglan) may be prescribed. Metoclopramide (Reglan) is the oldest and most commonly used prokinetic drug. It is available only by prescription because it can cause some severe adverse effects if not used correctly. Metoclopramide is used for the treatment of delayed gastric emptying and gastroesophageal reflux and also as an antiemetic. Its use is contraindicated in patients with seizure disorder, pheochromocytoma, breast cancer, or GI obstruction and also in patients with a hypersensitivity to it or to procaine or procainamide. Metoclopramide is available in both oral and parenteral formulations. GERD: Causes: inappropriate relaxation of the LES (stomach contents w/ pH of 2 coming into esophagus where pH is normally 7 or 8). Irritation from refluxed material. Delayed gastric empyting, gastric volume or intra abdominal pressure is increased. Abnormal esophageal clearance. Gastric acid & pepsin cause the tissue injury. Barrett’s epithelium: a disorder of the lower esophagus marked by a benign ulcerlike lesion in columnar epithelium, resulting most often from chronic irritation of the esophagus by gastric reflux of acidic digestive juices. Major symptoms include dysphagia, decreased lower esophageal (LES) pressure, and heartburn. Symptoms may be relieved by eating frequent small meals, avoiding foods that produce gas, taking antacid medication, and elevating the head of the bed to prevent passive reflux when lying down. Treatment consists of proton pump inhibitors and H2 blockers. The lesion is considered premalignant, and surveillance endoscopy is performed to screen for esophageal cancer. Physical manifestations of GERD: dyspepsia after meals & lasts 1 to 2 hours; regurgitation (aspiration is biggest GI complication); hypersalivation (water brash): heartburn with regurgitation into the mouth of fluid that may be sour or almost tasteless; dysphagia & odynophagia (a severe sensation of burning, squeezing pain while swallowing caused by irritation of the mucosa or a muscular disorder of the esophagus, such as gastroesophageal reflux; bacterial or fungal infection; tumor; achalasia; or chemical irritation.); chronic cough, atypical chest pain, belching, flatulence or bloating. Diagnosis of GERD: 24 hour ambulatory pH monitoring Meds that make GERD worse: oral contraceptives, anticholinergenics, sedatives, tranquilizers, B adrenergic agonists, nitrates & Ca Channel Blockers (they all slow gut movement & then reflux occurs as food stays longer in stomach) Anticholingenic: an anti-cholinergic agent that functions by competing with the neurotransmitter acetylcholine for its receptor sites at synaptic junctions. Anticholinergics are used to treat spastic disorders of the GI tract, to reduce salivary and bronchial secretions before surgery, or to dilate the pupil. Some anticholinergics reduce parkinsonian symptoms but are never considered primary agents for therapy. Atropine in large doses stimulates the central nervous system and in small doses acts as a depressant. Among numerous cholinergic blocking agents are atropine, belladonna, glycopyrrolate, hyoscyamine, methixene hydrochloride, trihexyphenidyl hydrochloride, and scopolamine. Surgical therapy for GERD: Laparoscopic Nissen fundoplication (LNF) is the minimally invasive surgery commonly used for hiatal hernia repair. Complications after LNF occur less frequently compared with those seen in patients having the more traditional open surgical approach. Hiatal Hernia: Protrusion of stomach through the esophagus. MUST have bowel sounds before you can eat after hernia surgery. Surgery is LNF (same as GERD). Reinforces the LES, wraps a portion of the stomach around the distal esophagus to anchor it. Risk for bleeding is biggest risk, also chance of infection & respiratory complication (people who have had this surgery don’t want to take deep breaths b/c it hurts. Can begin PO once bowel sounds return. Have to watch for gas-bloat syndrome & air swallowing. Peptic Ulcer Disease: A peptic ulcer is a mucosal lesion of the stomach or duodenum. Peptic ulcer disease (PUD) results when mucosal defenses become impaired and no longer protect the epithelium from the effects of acid and pepsin. Three main types: gastric, duodenal & stress. Gastric ulcer: (aspirin & NSAIDS inhibit prostaglandins which irritates the GI). Prostaglandins increase the barrier’s resistance to ulceration by producing mucous. Acid, pepsin, and H. pylori infection play an important role in the development of gastric ulcers. The gastric mucosal barrier overlies the epithelium. The secretion of mucus and bicarbonate provides a first line of defense in maintaining a near-normal pH on the gastric epithelium and protects the mucosal barrier against acid. Gastromucosal prostaglandins increase the barrier's resistance to ulceration. The integrity of the barrier is enhanced by the rich blood supply of the mucosa of the stomach and duodenum. When a break in the mucosal barrier occurs, hydrochloric acid injures the epithelium. Gastric ulcers may then result from back-diffusion of acid or dysfunction of the pyloric sphincter (Fig. 58-1). Without normal functioning of the pyloric sphincter, bile refluxes (backs up) into the stomach. This reflux of bile acids may break the integrity of the mucosal barrier and produce hydrogen ion back-diffusion, which leads to mucosal inflammation. Toxic agents and bile then destroy the membrane of the gastric mucosa. (pyloric sphincter: a sphincter at the opening from the stomach into the duodenum. It is usually closed, opening only for a moment when a peristaltic wave passes over it.) High fat & protein meals stay in stomach much longer & aggravate… BRAT (bananas, applesause, rice & tea) diet helps to settle. Duodenal Ulcers: Most duodenal ulcers occur in the upper portion of the duodenum. They are deep, sharply demarcated lesions that penetrate through the mucosa and submucosa into the muscularis propria (muscle layer). The floor of the ulcer consists of a necrotic area residing on granulation tissue and surrounded by areas of fibrosis. The main feature of a duodenal ulcer is high gastric acid secretion, although a wide range of secretory levels is found. In patients with duodenal ulcers, pH levels are low (excess acid) in the duodenum for long periods. Protein-rich meals, calcium, and vagus nerve excitation stimulate acid secretion. Combined with hypersecretion, a rapid emptying of food from the stomach reduces the buffering effect of food and delivers a large acid bolus to the duodenum (see Fig. 581). Inhibitory secretory mechanisms and pancreatic secretion may be insufficient to control the acid load. Many patients with duodenal ulcer disease have confirmed H. pylori infection. These bacteria produce substances that damage the mucosa. Urease produced by H. pylori breaks down urea into ammonia. Hydrogen ions are then released in response to the presence of ammonia and contribute further to mucosal damage. Billroth 1: the surgical removal of the pylorus in the treatment of gastric cancer or peptic ulcer disease. The proximal end of the duodenum is anastomosed to the stomach. Billroth 2: the surgical removal of the pylorus and the first part of the duodenum. The cut end of the stomach is anastomosed to the jejunum, which is pulled through the transverse mesocolon from the lower abdomen. The remaining duodenum carrying biliary and pancreatic secretions drains into the ileum through a new anastamosis in the lower abdomen. Also called gastrojejunostomy. Dumping Syndrome: the combination of profuse sweating, nausea, dizziness, and weakness experienced by patients who have had a subtotal gastrectomy. Symptoms are felt soon after eating, when the contents of the stomach empty too rapidly into the duodenum. The entrance of this hypertonic material into the small intestine causes fluid to shift into the intestine via osmosis. This increased volume causes peristalsis and diarrhea. The loss of fluid from capillaries causes hypotension with resulting weakness and dizziness. A high-protein, high-calorie diet, with small, dry meals taken frequently, should prevent discomfort and ensure adequate nutrition. See also gastrectomy. Post op GI surgery: deficiencies of vitamin B12, folic acid & iron. Impaired Ca metabolism & reduced absorption of Ca & vitamin D. Shortage of intrinsic factor r/t the resection & rapid emptying of the food, pernicious anemia-weak, anemic, atrophic glossitis-beefy shiny tongue. Irritable Bowel Syndrome: abnormally increased motility of the small and large intestines, of unknown origins. Most of those affected are young adults who complain of diarrhea and, occasionally, pain in the lower abdomen. The pain is usually relieved by passing flatus or stool. In diagnosing irritable bowel syndrome, other more serious conditions, such as dysentery, lactose intolerance, and the inflammatory bowel diseases, must be ruled out. Because there is no organic disease present in irritable bowel syndrome, no specific treatment is necessary. Many persons benefit from the use of bulk-producing agents in the diet because bulk tends to stabilize the water content of the stool. Antidiarrheal drugs are helpful in decreasing the frequency of stool. Although this is a functional disorder, patients experience pain and discomfort and need emotional support. Mild tranquilizers or antidepressants are sometimes given to relieve anxiety or depression. Also called functional bowel syndrome, mucous colitis, spastic colon. Manning criteria: abdominal pain relieved by defecation, abdominal distention, sensation of incomplete evacuation of stool, presence mucus w/ the stool… Pain in LLQ & cramps, may be tenderness & air in bowels Dx: flexible sigmoidoscopy or colonoscopy if greater than 40 yoa or barium enema. Interventions: diet: limit caffeine, alcohol, sorbitol (artificial sweetner), take in fiber & bulk. Meds: bulk forming laxatives, antidiarrheals (loperamide, immodium), anticholinergics (bentyl to decrease GI spasms), antidepressants (elavil), 5-HT4 agonists (Zelnorm: stops GI tract pain & cramping) for prokinetic activity (allow to pass smoother), imitates serotonin to stimulate peristalsis Stress Mgmt: relaxation techniques. Colorectal Cancer: 95% are adenocarcinomas, most come from adenomatous polyps. a malignant neoplastic disease of the large intestine, characterized by a change in bowel habits; the passing of blood (melena), which may be occult initially; and anemias. Malignant tumors of the large bowel usually occur after 50 years of age, are slightly more frequent in women than in men, and are common in the Western world. They are rare in children; clustering in families is common. The risk of large bowel cancer is increased in patients with chronic ulcerative colitis, villous adenomas, and especially familial adenomatous polyposis of the colon. 75% of all colorectal cancers have no known predisposing factors, but people who have a high-fat diet and low activity levels may be more likely than others to have this cancer. In the vermiform appendix, carcinoid is the most common tumor. Most lesions of the large bowel are adenocarcinomas. These tumors have a long preinvasive stage, and, when they invade, they tend to grow slowly. Rectal tumors may cause pain, bleeding, and a feeling of incomplete evacuation. They may metastasize slowly through lymphatic channels and veins and occasionally prolapse through the anus. Typical napkin ring tumors in the sigmoid and descending colon grow circumferentially and constrict the intestinal lumen, causing partial obstruction and production of flat or pencil-shaped stools. Manifestations include progressive abdominal distension, pain, vomiting, constipation, cramps, and bright red blood on the stool's surface. Malignant lesions in the ascending colon are usually large growths that may be palpable on physical examination; they generally cause severe anemia and nausea. There may be dark red or mahogany-colored blood mixed with the stool. The diagnosis of colorectal cancer is based on digital rectal examination, testing for blood in the stool, proctosigmoidoscopic examination of the sigmoid, and x-ray studies of the GI tract. Colonoscopy is the definitive test for colorectal cancer. Suspicious polyps may be removed for histologic study, often through a sigmoidoscope or colonoscope or by laparotomy. Surgical treatment of colorectal cancer may involve a wide resection of the lesion, the surrounding colon, and the attached tissues. Tumors of the rectum may require removal of the entire rectum by abdominoperineal resection and the creation of a permanent colostomy. Chemotherapy and irradiation may be administered as palliative therapy or adjuvant treatment. Nursing care of the patient after a diagnosis of colorectal cancer focuses on coping with a possible loss of or alteration in body function. Familial Adenomatous polyposis 1% of cases but 100% malignant, usually start at age 20 Hereritary nonpolyposis colorectal cancer: 10% of cancers, also hereditary, develop by age 45. Colon cancer treated w/ chemo. Major complication is diarrhea & bleeding, colon cancer 3rd cause of death, spreads easily to liver & lungs. Manifestations: rectal bleeding, anemia & change in stool, gas pains, cramping or incomplete evacuation, hematochezia (bright red blood when in rectum). Tumors can grow large when in upper abdomen, mostly liquid stool, more pain when in lower abdomen. Tests: stool for occult blood, CEA, barium enema & CT of abdomen, colonscopy or sigmoidoscopy. Post op care after colostomy: change bag every 7 days, no beer, broccoli, gas forming foods, psych adj to the colostomy. Intestinal obstruction Mechanical obstruction: bowel is physically obstructed by adhesions or tumors. Nonmechanical obstruction: paralytic or adynamic ileus: paralytic ileus: a decrease in or absence of intestinal peristalsis. It may occur after abdominal surgery or peritoneal injury or be associated with severe pyelonephritis; ureteral stone; fractured ribs; myocardial infarction; extensive intestinal ulceration; heavy metal poisoning; porphyria; retroperitoneal hematomas, especially those associated with fractured vertebrae; or any severe metabolic disease. The most common overall cause of intestinal obstruction, paralytic ileus is mediated by a hormonal component of the sympathoadrenal system. Also called adynamic ileus. observations Paralytic ileus is characterized by abdominal tenderness and distension, absence of bowel sounds, lack of flatus, and nausea and vomiting. There may be fever, decreased urinary output, electrolyte imbalance, dehydration, and respiratory distress. Loss of fluids and electrolytes may be extreme, and, unless they are replaced, the condition may lead to hemoconcentration, hypovolemia, renal insufficiency, shock, and death. interventions Typically, computed tomography of the abdomen and pelvis is performed with PO and IV contrast to rule out anatomic obstruction. The patient is kept in bed in a low Fowler's position, and nothing is given by mouth. A nasogastric tube may be inserted into the stomach and connected to intermittent suction and the patient is positioned to facilitate the advancement of the tube, which is checked at intervals, usually every 30 to 60 minutes. The character of GI drainage is monitored at intervals, usually every 2 to 4 hours, and any increase or decrease in the amount or changes in the color or consistency is reported. Bowel sounds, blood pressure, pulse, and respirations are checked every 2 to 4 hours, or as indicated in a particular circumstance, and rectal temperature usually every 4 hours. Abdominal girth is measured at least every 2 hours, and any increase is reported. Parenteral fluids with electrolytes and medication to promote peristalsis are administered as ordered; intake and output are measured, and, if less than about 30 mL of urine is excreted per hour, the physician is informed. The patient is helped to turn and deep breathe every 2 to 4 hours and is given oral hygiene every 1 to 2 hours. Active or passive rangeof-motion exercises are performed every 4 hours. Walking is helpful as gravity is a useful force. When intestinal output increases and bowel sounds return, the intestinal tube may be clamped and small amounts of warm tea may be given. If pain, distension, or cramps do not recur, the intestinal tube may be removed, but a rectal tube or an enema may be ordered to relieve distension. nursing considerations The concerns of the health care providers include monitoring and reporting the signs of paralytic ileus and its potential complications, ensuring that the patient is as comfortable as possible, explaining the purpose of the intestinal tube, and walking with the patient, encouraging ambulation. The patient is instructed to try to avoid mouth breathing because swallowed air can increase distension. Before surgery, patients need reassurance that the sutures are strong and the distended abdomen will not burst. Intestional obstruction: fluid leaks into the peritoneal cavity. Trapped fluid decreases the absorption of fluid and electrolytes into the vascular space. This leads to reduced blood volume & electrolyte imbalance which can = hypovolemic shock. Specific fluid and electrolyte problems result, depending on the part of the intestine that is blocked. An obstruction high in the small intestine causes a loss of gastric hydrochloride, which can lead to metabolic alkalosis. Obstruction below the duodenum but above the large bowel results in loss of both acids and bases, so that acid-base imbalance is usually not compromised. Obstruction at the end of the small intestine and lower in the intestinal tract causes loss of alkaline fluids, which can lead to metabolic acidosis. Chronic inflammatory BowelDisease: Ulcerative colitis: a chronic, episodic, inflammatory disease of the large intestine and rectum. It is characterized by profuse watery diarrhea containing varying amounts of blood, mucus, and pus. Some of the many systemic complications of ulcerative colitis include peripheral arthritis, ankylosing spondylitis, kidney and liver disease, and inflammation of the eyes, skin, and mouth. People with severe disease may develop toxic megacolon, a dangerous complication that may lead to perforation of the bowel, septicemia, and death. Observations: The attacks of diarrhea are accompanied by tenesmus, severe abdominal pain, fever, chills, anemia, and weight loss. Children with the disease may suffer retarded physical growth. The debilitating symptoms often prevent people with ulcerative colitis from carrying on the normal activities of daily living. Diagnosis of the disease is based on clinical signs, the results of barium x-ray films of the colon, and colonoscopy with biopsy. It is often difficult to differentiate between ulcerative colitis and Crohn's disease. Interventions: Medical treatment with corticosteroids or other antiinflammatory agents may help control the symptoms in some people. Those with severe disease or life-threatening complications may require surgery. Total proctocolectomy with ileostomy is a permanent cure. Ulcerative colitis carries an increased risk of cancer of the colon, and periodic colonoscopy is performed to rule out this complication. A person with ulcerative colitis is suffering from a chronic, life-threatening illness and requires frequent evidence of support and understanding during prolonged hospitalization. Chron’s Disease: a chronic inflammatory bowel disease of unknown origin, usually affecting the ileum, the colon, or another part of the GI tract. Diseased segments may be separated by normal bowel segments, which give it the characteristic “skip lesions.”