Amino group needs to be excreted

Chapter 10: The Water-
Soluble Vitamins
Overview of Water-Soluble
Vitamins
Dissolve in water
Easily destroyed or washed out during food storage and preparation.
Are easily absorbed and excreted
Not stored in the body tissues and must be replaced each day.
Seldom reach toxic levels
Overview of Water-Soluble Vitamins
Many B-complex vitamins needed for energy metabolism and form an integral part of coenzymes
Help the body metabolize CHO, lipids and amino acids
Thiamin pyrophosphate – TPP ( thiamin )
Flavin Adenine Dinucleotide (FAD), Flavin Mononucleotide
(FMN)( riboflavin )
Nicotinamide Adenine Dinucleotide (NAD), Nicotinamide adenine dinucleotide phosphate (NADP)( niacin )
Coenzyme A ( pantothenic acid )
Pyridoxal phosphate (PLP) ( Vitamin B-6 )
Tetrahydrofolic acid ( folate )
Cofactor ( biotin )
Enrichment Act of 1941 and 1998
Many nutrients lost through milling process of grains
Grain/cereal products are enriched with
Thiamin, riboflavin, niacin, folate, iron
Enriched grains still deficient in B-6, magnesium and zinc
Whole grains contain original nutrients
Distinction between water-soluble and fat-soluble vitamins
Fat-soluble vitamins Water-soluble vitamins
Absorption
Transport
Lymph first, then the blood Direct absorption into the blood
Protein carriers used by many Freely transported
Requireme nts
Periodic doses required
Storage
Excretion
Toxicity
Stored in cells associated with fat
Less readily excreted, tend to remain in fat-storage sites
Toxic levels likely when consuming supplements
Frequent doses required
Circulate in waterfilled parts of the body
Excreted in urine by kidneys
Toxic levels possible when consuming supplements
Thiamin
Functions as a coenzyme: Thiamin pyrophosphate
(TPP)
In metabolism of CHO; & amino acids
Decarboxylation of alpha keto acids (page 227)
Enzyme is Transketolase: coverts glucose to a 5carbon sugar
Food Sources of Thiamin
Wide variety of food
White bread, pork, hot dogs, luncheon meat, cold cereal
Enriched grains/ whole grains
RDA For Thiamin
1.1 mg/day for women
1.2 mg/day for men
Most exceed RDA in diet
Surplus is rapidly lost in urine; non toxic
Deficiency of Thiamin
Beriberi
first observed in the Far East where polished rice replaced rice where bran remained intact
.
characterized by
loss of sensation in the hands and feet, muscular weakness, advancing paralysis,and abnormal heart action.
Peripheral neuropathy
Dry beriberi
Weakness, nerve degeneration, irritability, poor arm/leg coordination, loss of nerve transmission
Wet beriberi
Edema, enlarge heart, heart failure
Wenicke-Koisakoff Syndrome
Mainly in alcoholics
Alcohol diminishes thiamin absorption
Alcohol increases thiamin excretion
Poor quality diet
Involuntary eye movement; double vision
Ataxia: staggering, poor muscle coordination
Mental confusion, “drunken stupor”
Riboflavin
Coenzymes:
Flavin mononucleotide ( FMN )
Flavin adenine dinucleotide ( FAD )
Oxidation-reduction reactions
Electron transport chain
Citric Acid Cycle
Catabolism of fatty acids: beta oxidation
FMN shuttles hydrogen ions and electrons to into the electron transport chain
Food Sources of Riboflavin
Milk/products
Enriched grains
Liver
Oyster
Brewer’s yeast
Sensitive to uv radiation (sunlight)
Stored in paper, opaque plastic containers
RDA for Riboflavin
1.1 mg/day for women
1.3 mg/day for men
Average intake is above RDA
Toxicity not documented
Deficiency of Riboflavin
Ariboflavinosis
Glossitis, cheilosis, seborrheic dermatitis, stomatitis, eye disorder, throat disorder, nervous system disorder
Niacin
Nicotinic acid (niacin) & nicotinamide
(niacinamide)
Coenzyme
Nicotinamide adenine dinucleotide ( NAD )
Nicotinamide adenine dinucleotide phosphate
( NADP )
Oxidation-reduction reaction
Food Sources of Niacin
Mushroom
Enriched grains
Beef, chicken, turkey, fish, eggs,milk
Amino acid tryptophan can be converted to niacin
Heat stable; little cooking loss
60mg tryptophan can be converted into 1 mg niacin
Estimate by dividing the total gram of protein by
6
Deficiency of Niacin
Pellagra
3 Ds: Dermatitis, dementia, diarrhea
appeared in Europe in early 1700s when corn became staple food
corn lacks niacin and tryptophan
Niacin as a Medicine
75-100 x RDA can lower LDL and increase HDL
Slow/ reverse progression of atherosclerosis with diet and exercise
Toxicity effects
Flushing of skin, itching, nausea, liver damage
Content Review
How are water-soluble vitamins different from fatsoluble vitamins?
Many of the B vitamins all function as a coenzyme, what is a coenzyme?
What disease is associated with a deficiency of niacin?
What disease is associated with a deficiency of thiamin?
What is the Enrichment Act? What nutrients are involved?
Pantothenic Acid
Part of Coenzyme-A
Essential for metabolism of CHO, fat, protein
Glucose
Fatty acids AcetylCoA
Alcohol
Amino Acids
Food Sources of Pantothenic
Acid
Meat
Milk
Mushroom
Liver
Peanut
Adequate Intake = 5 mg/day
Average intake meets AI
Biotin
Free and bound form
Biocytin (protein bound form)
Freed by Biotinidase in small intestine
Infant with genetic defect : low levels of biotinidase
Metabolism of CHO, fat, protein (C skeleton)
DNA synthesis
Functions of Biotin
Required to convert pyruvate to oxaloacetate
(TCA cycle) and thus ATP production.
Required for fatty acid synthesis
Breaks down leucine
Sources
Widely distributed in foods and is produced by intestinal bacteria
Liver, egg yolk , whole grains, cauliflower are good food sources
Avidin in raw egg whites bind biotin
Biotin Needs
Adequate Intake is 30 ug/day for adults
This may overestimate the amount needed for adults
No Upper Limit for biotin
Biotin Deficiency
Rare
High intake of raw egg white diet
Alcoholics
Biotinidase deficiency
Anticonvulsant drug use
Signs & symptoms: skin rash, hair loss, convulsion, neurological disorders, impaired growth in children
Vitamin B-6 family: Pyridoxal,
Pyridoxine, Pyridoxamine
Main coenzyme form: pyridoxal phosphate
( PLP )
Activate enzymes needed for metabolism of
CHO, fat , protein
Transamination
Synthesis of hemoglobin and oxygen binding and white blood cells
Synthesis of neurotransmitters
Functions of Vitamin B-6
Participates in 100+ enzymatic reactions
Decarboxylation of amino acid (decarboxylase)
Transamination reaction (transaminase)
Structural rearrangement of amino acids (racemase)
Heme synthesis
CHO metabolism
Lipid metabolism
Neurotransmitter Synthesis
Conversion of tryptophan to niacin
Other Role of Vitamin B-6
Homocysteine
From the metabolism of methionine
Produces toxic effect on arterial walls
(atherosclerosis)
Metabolized by vitamins B-6, B-12 and folate
Food Sources of Vitamin B-6
Meat, fish, poultry
Whole grains (not enriched back)
Banana
Spinach
Avocado
Potato
Heat and alkaline sensitive
RDA for Vitamin B-6
1.3 - 1.7 mg/day for adults
Daily Value set at 2 mg
Average intake is more than the RDA
Deficiency of Vitamin B-6
Microcytic hypochromic anemia
Seborrheic dermatitis
Convulsion, depression, confusion
Reduced immune response
Peripheral nerve damage
Factors That Affect B-6
Requirement
Alcohol reduces PLP formation
L -DOPA-medication used to treat
Parkinson’s disease and
Isoniazid-antituberculosis medication
Reduce blood concentration of PLP
Need extra vitamin B-6
B-6 As A Medicine?
PMS
B-6 to increase the level of serotonin
Improve depression
Not a reliable treatment
Toxicity potential
Can lead to irreversible nerve damage with > 200 mg/day
Upper level set at 100 mg/day
Folate (Folic acid, Folacin)
Consists of pteridine group, para-aminobenzoic acid (PABA), and glutamic acid
Coenzyme form: tetrahydorfolic acid ( THFA )
Produce many identical deficiency signs and symptoms as vitamin B-12
Vitamin B-12 is needed to recycle folate coenzyme
Absorption, Metabolism of Folate
Absorbed in the monoglutamate form with the help of folate conjugase
Actively absorbed during low to moderate intake
Passively absorbed during high intake
Delivered to the liver where it is changed back to the polyglutamate form
Mostly stored in the liver
Excreted in the urine and bile
(enterohepatic circulation)
Functions of Folate
DNA synthesis
Transfer of single carbon units
Synthesis of adenine and guanine
Anticancer drug methotrexate
Homocysteine metabolism
Neurotransmitter formation
Amino acid metabolism
Food Sources of Folate
Liver
Fortified breakfast cereals
Grains, legumes
Foliage vegetables
Susceptible to heat, oxidation, ultraviolet light
RDA for Folate
400 ug/day for adults
Daily Value is set at 400 ug
Dietary folate equivalents (DFE)
are units to express folate needs throughout life except during child bearing years
DFE = [(total synthetic folate) x 1.7] + total food folate intake
Deficiency of Folate
Similar signs and symptoms of vitamin B-
12 deficiency
Pregnant women
Alcoholics
Interferes with the enterohepatic circulation of bile/folate
Megaloblastic Anemia
Neural Tube Defects
Spina bifida
Anencephaly
Importance of folate before and during pregnancy
Toxicity of Folate
Epilepsy
Skin, respiratory disorder
FDA limits nonprescription supplements to
400 ug per tablet for non-pregnant adults
OTC Prenatal supplement contains 800 ug
Upper Level for synthetic folate is 1 mg
Excess can mask vitamin B-12 deficiency
Vitamin B-12
Cyanocobalamin, methlcobalamin,
5-deoxyadenosylcobalamin
Contains cobalt
Folate metabolism
Synthesized exclusively by bacteria, fungi, and algae
Maintenance of the myelin sheaths
Rearrange 3-carbon chain fatty acids so can enter the Citric Acid Cycle
Absorption of Vitamin B-12
Therapy for Ineffective Absorption
Many factors can disrupt this process
Monthly injections of vitamin B-12
Vitamin B-12 nasal gel
Megadoses of vitamin B-12 to allow for passive diffusion
Food Sources of Vitamin B-12
Synthesized by bacteria, fungi and algae
(Stored primarily in the liver)
Animal products
Organ meat
Seafood
Eggs
Hot dogs
Milk
RDA for Vitamin B-12
2.4 ug/ day for adults and elderly adults
Average intake exceeds RDA
B-12 stored in the liver; little is lost
Non-toxic
Functions of Vitamin B-12
Helps convert methylmalonyl CoA to succinyl CoA (citric acid cycle)
Recycles folate coenzymes
Nerve functions
Maintains myelin sheath
Megalobalstic anemia
Deficiency of Vitamin B-12
Pernicious anemia
Nerve degeneration, weakness
Tingling/numbness in the extremities
(parasthesia)
Paralysis and death
Looks like folate deficiency
Usually due to decreased absorption ability
Achlorhydria, especially in elderly
Homocysteine and the B Vitamins
Choline
Absorbed from the small intestine
All tissues contain choline
Excess choline is converted to betaine
Functions of Choline
Precursor for acetylecholine (neurotransmitter)
Precursor for phospholipids (such as lecithin)
Involved in the export of VLDL from the liver
Precursor for the methyl donor betaine
Assist in the conversion of homocysteine to methionine
Food Sources of Choline
Widely distributed
Milk
Liver
Eggs
Peanuts
Lecithins added to food
Deficiency rare
Needs for Choline
Adequate Intake is 550 mg/day for adult males
Adequate Intake is 425 mg/day for adult females
Normal consumption is ~700-1000 mg/day
High doses associated with fishy body odor, vomiting, salivation, sweating, hypotension,
GI effects
Upper Level is set at 3.5 g/day (3500 mg/day)
Deficiency of Choline
Decrease choline stores
Liver damage (fatty livers)
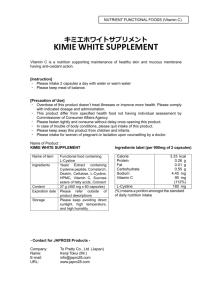
Vitamin C
Ascorbic acid (reduced form), dehydroascorbic acid (oxidized form)
Synthesized by most animals (not by human)
Absorbed by a specific energy dependant transport system
Passive transport if intake is high
Decrease absorption with high intakes
Excess excreted
Functions of Vitamin C
Reducing agent (antioxidant)
Iron absorption
Synthesis of carnitine, tryptophan to serotonin, thyroxine, cortiscosteroids, aldosterone, cholesterol to bile acids
Immune functions
Synthesis of other compounds
Questionable as to vitamin C’s role as an antioxidant in people
Collagen Synthesis
Food Sources of Vitamin C
Citrus fruits
Potatoes
Green peppers
Cauliflower
Broccoli
Strawberries
Romaine lettuce
Spinach
Easily lost through cooking
Sensitive to heat
Sensitive to iron, copper, oxygen
RDA for Vitamin C
90 mg/day for male adults
75 mg/day for female adults
+35 mg/day for smokers
Average intake ~72 mg/day
Fairly nontoxic (at <1 gm)
Upper level is 2 gm/day
Excess intake will not cure the common cold
Deficiency of Vitamin C
Scurvy
Deficient for 20-40 days
Fatigue, pinpoint hemorrhages
Bleeding gums and joints, hemorrhages
Associated with poverty
Vitamin-Like Compounds
Carnitine
Inositol
Taurine
Lipoic acid
Synthesized in the body at the expense of amino acids and other nutrients
Carnitine
Found in meat and dairy products
Synthesized in the liver from amino acids lysine and methionine
Transports fatty acids into the mitochondria
Aids in the removal of excess organic acids
Inositol
Myo-inositol
Found in animal products
Synthesized from glucose
Precursors to eicosanoids
Metabolizes calcium ions
Metabolism is altered in people with diabetics, multiple sclerosis, kidney failure, certain cancers
Taurine
Found only in animal products
Synthesized from methionine and cysteine
Associated with the photoreceptor in the eye
Antioxidant activity in the white blood cell and pulmonary tissue
CNS function, platelet aggregation, cardiac contraction, insulin action, cell differentiation and growth
Lipoic Acid
Found in meats, liver, and yeast
Redox agent
Needed in reactions in which CO
2 is lost from a substrate
Regenerates vitamin C and glutathione
Bogus “Vitamins”
Para-aminobenzoic acid (PABA)
Part of folate, but not able to make folate
A part of a B-complex family for bacteria
Laetrile
“Vitamin B-17”
Contains cyanide, promoted as a cancer cure
Bioflavonoids
“Vitamin P” --no nutritional requirement
Pangamic Acid
“Vitamin B-15” and is illegal
Cancer
Many diseases
Formation of tumors (neoplasms)
Benign
Malignant
Types of Cancers
Carcinomas
Cells that covers the body, including the secretory organs
Sarcomas
Connective tissues and bones
Leukemias
Blood forming tissues
Lymphomas
Lymph nodes or lymphoid tissues
Cancer Deaths
Carcinogenesis
Protooncogenes
Genes that cause a resting cell to divide
Tumor Suppressor Genes
Genes that prevent cells from dividing
P53 gene finds error on the DNA and repairs it
Oncogene
The cancer gene
A protoonocogene out of control
DNA Repair Mechanism
Cell Replication
Telomeres
Caps at the ends of chromosomes
Telomerase
Enzyme that maintains the length and completeness
Daughter cells are slightly shorter and telomerase activity decreases
Cell undergoes apoptosis
Malignant tumor cells, the telomerase activity increases —the cells can live indefinitely
Cancer Initiation, Promotion, and
Progression
Cytochrome P-450
Prevents cancer initiation
In the liver and intestinal cells
Converts dangerous compounds into harmless water-soluble metabolites
Cancer Initiation
Exposure to carcinogen
Alteration of DNA
Is relatively short
Cancer Promotion
May last for months or years
Damage is “locked” in
Cell division increases
Promoters: estrogen, alcohol, maybe dietary fat
Decrease time available for repair
Cancer Progression
Final stage
Cancer cells proliferate and form a mass
Invade surrounding tissue
Metastasize to other tissues
Heredity can only explain a small percentage of cancers
Environment contributes to most cancer
Role of Diet
Excessive intake of calories increases the risk of cancer
Excessive body fat affects sex hormone production
High intake of fruits and vegetables is associated with lower risk
High intake of meats and protein is associated with higher risk
Excessive alcohol increases the risk
Excessive charcoal broiling increases risk
Nitrosamines (from nitrite) increases risk
Mycotoxins (from fungi) increases risk
Fat and Cancer
The National Academy of Sciences recommends 30% of total calories from fat
Effects of the type of fat to cancer
There are still wide gaps in knowledge linking fat and cancer
Excessive intake is a more likely cause
Calcium,Vitamin D and Cancer
Calcium intake is inversely related to cancer
Calcium binds to bile acids in the colon
Vitamin D inhibits progression of cancerous polyps
Vitamin D inhibits rapid colon/rectal cell growth in patients with ulcerative colitis
Recommendations to Reduce the
Risk for Cancer
Remain physically active
Avoid obesity
Engage in physical training that promotes lean muscle mass
Consume abundance of fruits and vegetables
Consume plenty of low-fat/nonfat dairy products
Avoid high intakes of red meat and animal fat
Avoid excessive alcohol
Warning Signs
(CAUTION)
Early detection is critical
Unexplained weight loss
A c hange in bowel or bladder habits
A sore that does not heal
U nusual bleeding or discharge
A t hickening or lump in the breast or elsewhere
I ndigestion or difficulty in swallowing
An o bvious change in a wart or a mole
A n agging cough or hoarseness