THE BLOOD
advertisement

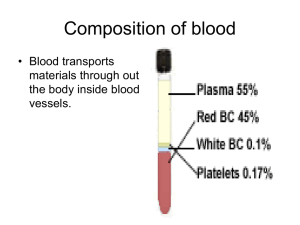
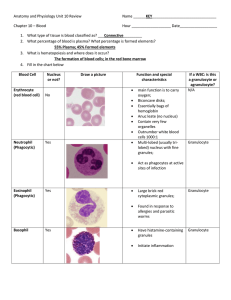
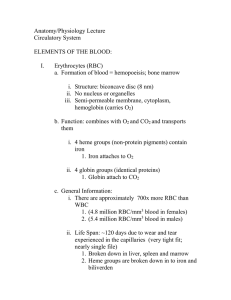
The Cardiovascular system • Components: – Blood – Heart – Blood vessels THE BLOOD • Blood Components – Plasma – 55% of blood – Water – 91% – Proteins (most abundant molecules): • Albumins – osmotic pressure - buffer • Globulins – immunity • Fibrin – blood clots – Electrolytes: Na, Ca, Cl, Mg – Nutrients, wastes Formed elements • • • • • Red blood cells White blood cells Platelets All formed in the bone marrow Within the bone marrow, all blood cells originate from a single type of unspecialized cell called a stem cell. • When a stem cell divides, it first becomes an immature red blood cell, white blood cell, or platelet-producing cell. • The immature cell then divides, matures further, and ultimately becomes a mature blood cell. • The rate of blood cell production is controlled by the body’s needs. • Normal blood cells last for a limited time (ranging from a few hours to a few days for white blood cells, to about 10 days for platelets, to about 120 days of RBC’s ) • Therefore, these cells must be replaced constantly. • Certain conditions may trigger additional production of blood cells. • When oxygen content of body tissues is low or the number of red blood cells decreases, the kidney’s produce and release erythropoietin, a hormone that stimulates the bone marrow to produce more red blood cells. • More WBC’s are produced and released in response to infection. • It produces and releases more platelets in response to bleeding. • Red Blood Cells – Carry oxygen gas to body tissues – Filled with hemoglobin • Four subunits; each has heme + iron • Heme binds and releases oxygen gas • Strong affinity for carbon monoxide – Life cycle of red blood cell • • • • Born in the bone marrow Synthesizes hemoglobin, matures Goes into circulation Physical wear and tear accumulates • After about 120 days, sticks in liver or spleen • Cell is phagocytised by macrophages • Hemoglobin protein is digested • Heme broken down to bilirubin – build up = jaundice • Iron is recycled to new hemoglobin • Hormone erythropoietin controls rate of red cell production in the bone marrow • White blood cells – 4,000 – 11,000 per cu. mm of blood – Clean up wastes and debri – phagocytosis (cell eating) – Protect against disease (immune system) – There are 5 different kinds of WBC’s • Neutrophils: 60-70% - function phagocytosis. • Eosinophils: 2-4% - Destroy parasitic worms. Combat effects in allergic responses caused by histamine. • Basophils: 0.5 – 1% - Produce heparin and histamine. • Lymphocytes: 25% - round nucleus, small amount of cytoplasm – mediate immune response – B cells form antibodies – T cells attack invaders. • Monocytes: largest WBC – kidney shaped nucleus – phagocytosis • Platelets or thrombocytes: Cell fragments (megakaryocyte) circulating in the blood – involved in the cellular mechanisms of hemostasis or blood clotting • Dysfunction or low levels of platelets predisposes to bleeding. • High levels usually asymptomatic, but may increase the risk of thrombosis - clotting Blood Types • What are the different blood groups? • The differences in human blood are due to the presence or absence of certain carbohydrate or protein molecules called anigens and antibodies. The antigens are located on the surface of the RBC’s and the antibodies are in the plasma. Individuals have different types of combinations of these molecules. The blood group you belong to depends on what you have inherited by your parents. • ABO and Rh systems are the most important ones used for blood transfusions • Not all blood groups are compatible with eachother. • Mixing incompatible blood groups leads to blood clumping or agglutination, which is dangerous for individuals and can be fatal. • ABO blood grouping system • Blood group A – If you belong to the blood group A, you have A antigens on the surface of your RBC’s and B antibodies in your plasma. • Blood group B – If you belong to the blood group B, you have B antigens on the surface of your RBC’s and A antibodies in your plasma. • Blood group AB – If you belong to the blood group AB, you have both A and B antigens on the surface of your RBC’s and no A or B antibodies at all in your blood plasma • Blood group O – If you belong to the blood group O (null), you have neither A nor B antigens on the surface of your RBC’s but you have both A and B antibodies in your plasma. Rh grouping • Many people also have an Rh factor on their RBC’s surface. This is also an antigen. • Those who have it are called Rh+. Those who do not are called Rh-. • A person with Rh- blood does NOT have Rh antibodies in the plasma. But a person with Rhblood CAN DEVELOP Rh antibodies in the plasma if they receive Rh+ blood in a tranfusion. • A person with Rh+ blood can receive blood from a person with Rh- blood without any problems. Hemolytic Disease - Anemia • • • • Reduction in RBC population Diagnosed by hematocrit Sickle cell anemia Malaria Leukemia • Types of cnacer of the bone marrow • White blood cells abnormal • Risk factors include exposure to ionizing radiation and carcinogens • Acute and chronic • Myeloid and lymphoid Carbon Monoxide Poisoning • CO is odorless • Bonds much stronger to hemoglobin molecule than oxygen • Fumes from burning fuels primary cause • Can be treated if detected early Blood Clotting • When a blood vessel is damaged, clot plugs hole – Damaged cells release chemical signals – Platelets collect at site of damage – Enzyme cascade produces fibrin (protein strands that form a web) – Clot is formed • Hemophilia: genetic deficiency in clotting factor