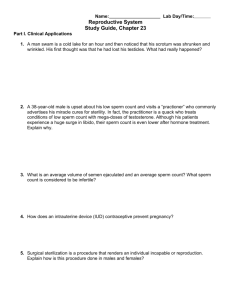
The Reproductive System
advertisement

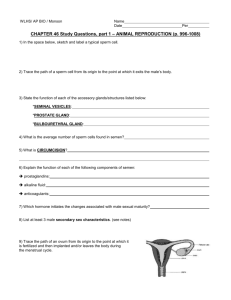
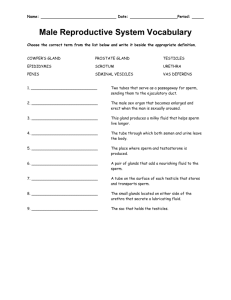
The Reproductive System Chapter 16 • ___________________-primary sex organs-ie. Testes and ovaries • _______________________--sex cells produced by gonads as well as gonads secrete sex hormones • _______________________________-remaining reproductive structures • Joint purpose of Reproductive system is produce offspring--via sperm in males and ___________ in females gonads gametes Accessory reproductive organs ova • Zygote becomes embryo and then fetus • Anatomy of Male Reproductive System • Testes have exocrine-sperm producingfunction and endocrine-testosterone producing • Accessory structures in delivery of sperm to exterior or to female TESTES- Tunica albuginea • Plum shaped---4 cm –sized surrounded by fibrous connective tissue capsule-_____________________________-“white coat” • Extensions of capsule extend into testes and divide into wedge-shaped ______________________each containing 14 _____________________________-sperm producing portion lobules Seminiferous tubules • Seminiferous tubules empty into another set of tubules--____________________on each side of testis-sperm travel from rete to enter 1st part of duct system____________________-hugging external testis • In soft tissue around seminiferous tubules are __________________-that produce androgens-esp. testosterone---thus different tissue process sperm and then hormones Rete testis epididymis Interstitial cells • DUCT SYSTEM-inc. edididymis,ducus deferns, and urethra • A.___________________________-highly coiled tube-~6 mcapping superior testis and extends posterolaterallytemporary storage for immature sperm entering from testis • Takes sperm about _____________days to travel epididymis,maturing along the way...and become motile • During ejaculation,epididymis contracts to expel ___________into--_________________________________ epididymis 20 Sperm….ductus deferens • . Ductus Deferens (= vas deferens)-extends upward from epididymis through inguinal canal,to pelvic cavity and arches over superior bladder…enclosed w/ blood vessels and nerves and connective tissue sheath-______________________ and it travels up through inguinal canal Spermatic cord • Loops medially over ureter and goes down posterior bladder-expands as ampulla and empties into _________________--this passes through prostate gland and merges w/ urethra • Main function of ductus deferens is to _________________________ • At ejaculation smooth muscle squeeze sperm forward by ___________________ Ejaculatory duct Propel live sperm from storageepididymis and distal vas deferns peristalsis • A __________________________________is a contraceptive procedure that ligates-“tiesoff” ducus deferns in part that lies in scrotum---sperm are still produced-but don’t reach body exterior and are phagocytizedrendering male sterile vasectomy Urethra • From base bladder to tip of penis-terminal feature of male system-carries urine and sperm-however both never travel @ same time---bladder sphincter constricts @ ejaculation preventing this • 3 regions: 1) ______________-surrounded by prostrate • 2)_____________-from prostatic urethra to penis and 3)__________-runs length of penis Prostatic urethra Membranous urethra Spongy (penile)urethra ACCESSORY GLANDS AND SEMEN -inc. paired seminal vesicles,single prostate,bulbourethral glands and semen • A.____________________@ base of bladder make ~60% of seminal fluid-secretion rich in _________________which nourish and activate sperm • Each of its duct joins vas deferens on same side to form __________----thus sperm and seminal fluid enter urethra during ejaculation Seminal vesicles Fructose, vitamin C, proglastins… Ejaculatory duct Prostate-single doughnut –shaped gland-encircles prostatic urethra below bladder • Its glandular , milky secretion helps activate sperm---during ejaculation-fluid enters urethra through several small ducts • Since near rectum,can be palpitated rectally • Older men suffer hypertrophy of gland, strangling urethramaking urination difficult and increases risk of bladder infections-________________ and kidney damage • Treatments include :surgery,drugs or microwaves to shrink prostate,insertion of small balloon to push prostate away from urethra,incineration w/low energy radiation • ___________________-inflammation of prostate-common • _______________-most prevalent cancer in men-slow growing,usually cystitis prostatitis Prostatic cancer • C. _______________________-tiny pea-sized glands posterior to prostate, produce thick,c lear mucus draining into penile urethra----is 1st secretion to pass upon sexual arousal ---functions in cleansing urethra of acidic urine and is a sexual lubricant Bulbourethral glands D. Semen-milky white, somewhat sticky mixture of sperm and gland secretions ;transport medium for nutrients and chemicals that protect and aid in movement of sperm • Sperm have little cytoplasm or stored nutrients so __________________ is energy fuel • pH ~ 7.2-7.6 helps neutralize acidic vagina(3.5-4.0)protecting sperm(sperm are sluggish in acidic environment) • ________________-antibiotic chemical destroying certain bacteria • Hormone_______________-…………………………. fructose seminalplasmin relaxin Semen cont’d • Enzymes to enhance sperm motility • Substances to inhibit female reproductive immune response • Male infertility---causes include obstruction of duct system, hormone imbalance , environmental estrogens ,pesticides, too much alcohol….often _________________is checked to analyze sperm count, motility, and morphology,semen volume ,pH, fructose amount…sperm count should not be below 20 million /mL Semen analysis EXTERNAL GENITALIA-ie. Scrotum and penis • Scrotum-divided sac of skin outside abdominal cavity, normally hangs loosely, rendering testes temperature below body temp.( @ ~ 5.4 degrees lower)-necessary for healthy sperm production ,changes in scrotal surface area help maintain temp—example -wrinkles as pulls toward body during external cold temp’s • Penis-delivers sperm-consists of shaft ,glans penis tip and prepuce or foreskin-loose skin covering-often removed at circumcision/Internally-spongy urethra SURROUNDED by 3 elongated areas of _______________________that fill w/ blood during arousal-causing rigid erection Erectile tissue Male Reproductive Functions • SPERMATOGENESIS=sperm production-begins @ puberty and is lifelong • Millions/day • _________________primitive stem cells @ periphery of each seminiferous tubule/rapid mitotic division to build stem cell line….from birth to puberty spermatogonia Follicle-stimulating hormone Spermatogeneisis cont’d • @ puberty _______________________(FSH) is secreted in increasing amounts by ant. Pituitary gland…from here on out ,each division produces 1 stem cell-type A daughter ---which remains @ tubule periphery to maintain stem population…and 2nd,type B daughter-pushed toward tubule lumen to become primary spermatocyte and will undergo MEIOSIS • Gametes @ this stage are called _______-made by meiosis and have ½ genetic material (2n in humans=23 x 2) • As meiosis occurs ,primar y,then secondary spermatocytes pushed toward tubule of lumen • Spermatids NOT functional sperm-nonmotile and excess cellular baggage spermatids Spermatogenesis cont’d • During last stage-_______________-excess cytoplasm sloughed off and now have _________________________,equipped w/high metabolism and motility • Sperm head has DNA---essentailly nucleus • Anterior to head is ______________made by golgi and similar to large lysosome---which breaks down @ membrane and releases to help sperm penetrate follicle of egg Mature sperm compacted into 3 regionshead,midpiece and tail Acrosomehelmutlike Spermatogenesis cont’d • Filaments make long tail from centriloes in midpiece w/mitochondria wrapped around for necessary ATP • All of spermatogenesis-from primary spermatocyte to release of immature sperm takes 64-72 days • Sperm in lumen nonmotile and can’t fertilize….moved by peristalsis from tubules into epididymis---there further maturation and increased motility • Things that can alter sperm formation:________________- Some antibiotics,radiation,lead,some pesticides,marijuana,tobacco, excessive alcohol Testosterone production • PRODUCED BY INTERSITIAL CELLS • @ puberty FSH prods sperm production and ________________(LH) is also released by anterior pituitary on from here on out testosterone is produced continuosly,rising levels responsible for secondary sexual characteristics:___________________-testosterone not produced and secondary sex characteristics not produced_____________….castration will cause this or malfunction of interstitial cells…also cause sterility Luteinizing hormone Sexual infantilism Deeping voice,increased hair all over most of body-esp. axillary and pubic;skeletal muscle enlargement-more muscle mass;increased bone growth and density of bone FEMALE REPRODUCTIVE ANATOMY • Function in producing gametes(ova) and nurture/protect developing fetus • _____________________primary reproductive organsboth exocrine and endocrine in nature ovaries Ovarian follicles OVARIES Follicle cells • Shape of almonds but about twice as large • Internally __________________-each consisting of an immature egg-oocyte-surrounded by 1 or more layers called __________ • As developing egg matures follicle enlarges and produces fluid filled antrum-At this point follicle is called vesicular or _________________follicle,which is mature and ready to released during ____________________. • After ovulation,ruptured follicle is transformed into ___________________--“yellow body”,which degenerates Graafian follicle ovulation Corpus luteum Ovarian follicle Follicle cells Ovaries cont’d Ovarian ligaments • Ovulation ~ every 28 days….in older women ovaries are scarred and pitted from release of many eggs • Ovaries secured to lateral pelvis by _________________and medially by ______________and in between held by fold of peritoneum-broad ligament Suspensory ligaments DUCT SYSTEM-uterine tube,uterus and vagina • Fallopian(uterine) tubes—internal duct system • receive ovulated oocyte and provide fertilization site • each about 4” long,extends medially from ovary to empty in superior uterus • enclosed and supported by broad ligament • • • • Fallopian tubes cont’d little or no contact between fallopian tubes and ovariesinstead contact @ distal end is by funnel-shaped ____________________that has fingerlike projectionsfimbriae that surround ovary-- WHICH create fluidlike current that carries oocyte into fallopian tube---to thus journey to uterus At this point is where many potential eggs are lost in peritoneal cavity Cilia and peristalsis move oocyte along to uterus-taking about 3-4 days,but egg is viable ~24 hrs. after ovulation,so fertilization is usually in fallopian tube To reach oocyte,sperm must swim up through vagina and uterus to fallopian tubes---swimming against a downward beat of Cilia! infundibulum Fallopian tubes cont’d Pelvic inflammatory disease • Because fallopian tubes and ovaries are not physically continuous,this makes this area vulnerable to infection,such as bacteria of Gonorrhea…maybe causing __________________which can cause scarring and closing of tubes Uterus-located in pelvis between bladder and rectum • Hallow/functions to receive,retain,and nourish a fertilized egg • About the size and shape of a pear in women who haven’t been pregnant • Suspended by broad ligament and anchored by round and uterosacral ligaments • _________________=main portion • _________________-superior,rounded region above fallopian tube entrance fundus body Uterus cont’d • ______________-narrow outlet into vagina below • Wall is thick w/3 layers:1)inner mucosa________________-At implantation-fertilized egg burrows here/This layer sloughs off during ________________-menstruation every 28 days- if not fertilized • 2)______________-interlacing bundles of smooth muscle making bulky middle layercontracts during labor 3) perimetrium-outer serous layer(visceral peritoneum cervix endometrium myometrium menses • __________________________________common in women 30-50-risks factors inc. cervical inflammation,STDs,multiple pregnancies,promiscuity/detected w/Pap smear/slow growing ,usually Cervical cancer • Vagina-thin-walled tube 3-4”long/between bladder and rectum from cervix to body exterior=birth canal./also organ of copulation • Distally partially enclosed by __________mucosawhich is very vascular and bleeds when ruptured hymen EXTERNAL GENITALIA=VULVA • mons pubis-fatty,rounded area overlying pubic symphysishair after puberty • laterally are 2 skin folds w/hair-labia majora (encloses vestibule which houses external urethra opening and vagina)and l.minora • ______________ surround vagina and secretes for distal vagina • Clitoris-small protrusion that is corresponding to penis w/erectile tissue but no reproductive duct • ___________________-between ant. labial folds,anus and ischial tuberosities Greater vestibular glands perineum FEMALE REPRODUCTIVE FUNCTIONS AND CYCLES • OOGENESIS AND THE OVARIAN CYCLE • Females’ reproductive ability begins at puberty and ends around 50’s(menopause) • In developing female fetus,_________-female stem cells multiply rapidly to increase their numbers,then daughter cells-primary oocytes-push into ovary connective tissue and primary follicle forms around them • By birth,oogonia cease to exist and a lifetime supply of primary oocytes are in place---waiting 10-14 years to undergo MEIOSIS! • @ puberty , ant. Pituitary produces_________FSH-stimulates a small # of primary follicles to grow and mature each month and then ovulation occurs monthly….constituting the _________cycle oogonia Follicle-stimulating hormone ovarian • • • • • Oogenesis and ovarian cycle cont’d @ puberty ~ 250,000 oocytes remain w/ a small # activated each month….appx 500 of the 250,000 ova are released in the limited # of years of fertility The FSH prods the follicle to enlarge ,accumulating fluid in central antrum/Primary oocyte replicates chromosomes and MEIOSIS occurs-producing 1 ________________and polar Secondary oocyte body Follicle development to the point of rupture takes about 14 days with ___ovulation________________ occurring at just about this time Ovulation occurs at the response to _luteinizing hormone__LH Secondary oocyte is still surrounded by follicle cell capsule now called_corona radiata(“radiating crown”)…abdominal pain can accompany this-mittelschmerz • 1 developing follicle dominates each month/mature follicles not ovulated are overripe and deteriorate • Besides triggering ovulation each month,LH aso causes ruptured follicle to turn into corpus luteum(Both c.luteum and maturing follicle produce hormones) • If ovulated, secondary oocyte is penetrated by sperm in fallopian tube,THEN oocyte undergoes_________________________________making another polar body and ovum 2nd meiotic division • ….its 23 chromosomes are combined w/23 of sperm in fertilized egg • If not fertilized, deteriorates • Polar bodies deteriorate • Sperm v. egg:-sperm relies mostly on surrounding for nutrients,while—egg larger and______________________stocked w/ nutrients nonmotile UTERINE (MENSTRUAL) CYCLE • receptive to implantation only briefly---~ 7 days after ovulation • events of _____________________ are cyclic changes that endometrium goes through monthly in response to ovarian hormone changes • Anterior pituitary ____________________ hormones FSH and LH regulate Ovarian estrogen and progesterone • Typically cycle is 28 days w/ovulation occurring midway Menstrual cycle gonadotropic Menstrual cycle cont’d • 3 stages: • 1)______________________--superficial functional layer of thick endometrium is sloughed off-accompanied by 3-5 days bleeding---passing out vagina as menstrual flow/average blood loss 50-150mL(1/4-1/2 cup)….By day 5 ovarian follicles begin to produce estrogen • 2)__________________---is stimulated by estrogen levels to cause basal layer of endometrium to regenerate ,glands form w/in and endometrial blood supply increases…endometrium restores to velvety,thick and well vascularized—ovulation @ end of this phase in response to LH Days 1-5Menstrual phase Days 6-14-Proliferative phase Menstrual cycle cont’d • 3)______________________-progestrone levels have risen(by corpus luteum) and act on estrogen charged endometrium and increase blood supply more/also increasing size of endometrial glands and begin supplying nutrients into uterine cavity to sustain an embryo until implanted Days 15-28-Secretory phase • If fertilization does occur,embryo produces hormone similar to LH-causes ______________________________ • If fertilization does NOT occur,c. luteum degenerates and LH levels drop…This causes vessels supplying endometrium to go into spasms and kink—causing endometrial cells-deprived of O2 –to die ….setting stage for next menses • Cycle can vary from 21-40 days ,but time of ovulation is usually @ 14-15 days Corpus luteum to cont. producing its hormones HORMONE PRODUCTION BY OVARIES • Begin @ puberty • Follicle cells of growing follicles produce_______________________-causing the appearance of secondary sex characteristics :enlargement of fallopian tubes, vagina and external genitalia ;development of breasts ;axillary and pubic hair ;increased fat in hips and breasts and in general; Widening and lightening of pelvis; Onset of menses • Estrogen also has metabolic effects---ex-maintaing blood cholesterol(high HDL) and help Ca2+ uptake estrogens • Other ovarian hormone is ______________________________made by c.luteum as long as LH is present in blood…stopping 10-14 days after ovulation/helps establish menses w/estrogen,but does NOT contribute to secondary sex traits…plays a role in pregnancy by inhibiting contraction of endometrium and prepares_____________________(source of progesterone in pregnancy is placenta) For lactation progesterone Mammary glands • • • • • In both sexes ,but has normal functions in female---being important only once reproduction is accomplished— stimulated to increase size by estrogen Are actually modified sweat glands and part of integument ,in that sense….and anterior to pectoral muscles ________________-center pigmented area w/protruding nipple Internally has 15-25 lobes radiating around nipple/lobes are padded and separated by connective tissue and fat Within each lobe are smaller _________________ w/clusters of alveolar glands that _______________-produce milk into lactiferous ducts opening via the nipple to the outside areola lobules lactate • ______________________-2nd most common cause of death in American women---1 in 8 developing this condition….~10% hereditary and half traced to BRCA 1 and 2 gene/80% of women w/ gene contract cancer---other risk factors inc. early menses,late menopause,estrogen replacement therapy….Breast cancer is signaled by change in skin texture ,puckering and nipple leakage…can be detected by self examination and by ___________________-X-rays that reveal tumors too small to feel(<1 cm.) Breast cancer mammography ACCOMPLISHING FERTILIZATION • Sperm must reach secondary oocyte-viable 12-24 hours after leaving ovary/sperm viable ~ 24-48 hrs….Therfore, intercourse must occur no more than 2 days before ovulation and no later than 24 hrs. after ovulation---when oocyte is appx. 1/3 way down fallopian tube • Sperm attracted to oocyte by “homing device” chemicals—locating oocyte • Sperm take __hours to reach fallopian tube,however many leak out or are destroyed by vagina’s acidity---only a few hundred –few thousand make it to area of egg’s location • When sperm reach oocyte,cell surface hyraluronidase enzymes break down “cement” holding follicle cells of corona radiate around oocyte 1-2 • Once path cleared through corona,1000’s sperm undergo_______________________where acrosome membrane break down-releasing enzymes to lyse through oocyte membrane….then a single sperm can make contact w/oocyte membrane receptors---pulling head(nucleus) of sperm pulled into oocyte cytoplasm….****sperm reaching this point after acrosomal reactions have started are the more likely to fertilize • After a sperm has reached oocyte,2nd meiosis occurs--making ovum and polar body • Changes in fertilized egg preventing other sperm entry • _________________occurs @ moment genetic material of sperm combines w/ that of ovum to make________________-fertilized egg Acrosomal reaction zygote fertilization EVENTS OF EMBRYONIC AND FETAL DEVELOPMENT • Rapid MITOTIC division as zygote goes down fallopian tube-________________,w/daughter cells becoming smaller and smaller—large # of cells will be building block of embryo-until 9th week • By time embryo reaches uterus(3 days after ovulation)=_________________-ball of 16 cells looking like a raspberry…Since uterus not totally prepared for embryo yet, embryo floats in uterine cavity---using uterine secretions for nutreints @ this time--Unattached,continues to develop to ~ 100 cells---It then hallows out to form_________or chorionic vesicle morula cleavage blastocyst • @ this same time ,it is secreting a hormone called______________________(hCG)-this prods c.luteum of ovary continue hormone production(otherwise,endometrium would shed) • Pregnancy tests usually detect______________levels • Blastocyst also has __________________-forming large fluidfilled sphere and also an inner cell mass-small cell cluster to one side • By day 7 after ovulation,blastocyst attahes to endometrium,eroding away some of lining and envelops into thick mucosa Human chorionic gonadotropin hcg trophoblast • During this time the primary germ layers are forming from inner mass: • ______________________gives rise to nervous system and epidermis • ______________________forms mucosa and associated glands • __________________________gives rises to basically everything else ectoderm endoderm mesoderm • By day 14 after ovulation,implantation is complete and mucosa grown over embryo…The ______________of the blastocyst develops projections called chorionic villi,combining w/uterus to produce __________________________ trohoblast placenta • Once placenta has formed,embryonic body is surrounded by_____________________________-fluid –filled sac and attaches w/blood vessel stalk_____________________________________ • By 3rd week,placenta delivers nutrients and O2 to and removes wastes from embryonic blood---all through ____________________________ • By end of 2nd month,placeta becomes endocrine organ producing estrogen,progesterone,and other hormones to maintain pregnancy…c.luteum becomes inactive amnion Umbilical cord Placental barrier • By week 8--all organ systems laid down in some form and looks human • Week 9—Now called__________-now growth and organ specialization are major activities • As fetus,grows from ~ 3cm. and 1g to 36 cm(14”),~4kg(6-10 lbs.)…at birth ~ 22” • 270 days-10th lunar month-full term fetus 7 wks. EFFECTS OF PREGNANCY ON MOTHER • ___________________________-period from conception to birth • Anatomical changes• Uterus goes from fist sized to eventually nearing level of xiphoid processthorax widens as organs press on diaphragm • Center of gravity changes sometimes causing lordosois---thus backaches • Placental hormone____________________causes pelvic ligaments and pubic symphsis to relax,widen and become more flexible • Good nutrition necessary—needing only about 300 calories extra/day • Substances that can cross placental barriers are alcohol,nicotine,many drugs and maternal infections • _________________ termination of pregnancy by loss of fetus--spontaneous abortion is a miscarriage pregnancy relaxin abortion • Physiological Changes • GI system-morning sickness usually first trimester,as mother adjusts to elevated estrogens;heartburn because of displaced esophagus and displaced stomach;constipation –because GI motility decreased • Urinary system-kidneys now need to dispose of fetal metabolic wastes,producing MORE urine;also uterus compresses bladder---frequent urination-Ie. stress incontinence • Respiratory System-nasal mucosa responds to estrogen by swelling and congested,maybe nosebleeds ;respiratory rate increases but residual volume declines causing_______________-difficult breathing in later stages • Cardiovascular system-Total body water rises and blood volume increases 25-40%---helping in safeguarding from blood loss effects during labor;BP and pulse increase and raise cardiac output 20-40%;venous return from lower limbs may be impaired---maybe causing varicose veins dyspnea parturition CHILDBIRTH=________________________ • Usually w/in 15 days of calculated due date (280 days from last menstrual period) • _________________-series of events that expel infant from uterus • Initiation of labor • Estrogen has reached highest levels causing myometrium to form much ________________receptors-to be receptive to that hormone • AND interfering with progesterone’s quieting influence on uterine muscle—causing weak uterine contractions---called _________________contractions—often producing false labor labor oxytocin Braxton-Hicks contractions • Then ,cells of fetus produce oxytocin and this stimulates placenta to release _______________________stimulating more frequent and powerful contractions • Mom’s hypothalamus activated by emotional and physical stress---signals oxytocin release by posterior pituitary gland --rhythmic ,expulsive contractions-TRUE LABOR…positive feedback mechanism now w/hypothalamus,strengthening contractions • Anything that interferes w/oxytocin or proglastins can hinder onset of labor….example--antiproglastin drugs such as aspirin and ibuprofen proglastins Stages of Labor • 1st-_____________________________from time of true contractions until full-10 cm-dilation of cervix….contractions move from upper uterus to vagina,becoming more vigorous and softening cervix and thinning….amnion ruptures-“water –breaking”----usually 6-12 hours or MORE!!! Dilation stage • 2nd-Expulsion stage-full dilation to delivery…urge increases to push 20 min -50 min.---sometimes 2 hrs • Infant should be head first-Vertex position-skull as a wedge to dilate cervix…after head,rest of body comes out more easily…umbilical cord clamped off • _______________-buttocks-first • _________________-during a difficult 2nd stage,O2 delivery inadequate leading to cerebral palsy or epilepsy….often a Csection done to prevent these • 3rd-____________________-w/in 15 min.placenta usually expelled---placenta and other fetal membranes constitute ____________________ breech dystocia Placental stage afterbirth DEVELOPMENTAL ASPECTS • Gonads from 8th week and then accessory structures and external genitalia….all depends on presence or absence of testosterone • If genetic male fails to produce testosterone-female accessory structures form and external genitalia… • --If genetic female exposed to testosterone-male accessory ducts and glands as well as penis and scrotum….both cases are pseudohermaphrodites----a true hermaphrodite possesses ovaries and testes-rare case • XO female appears normal but lacks ovaries/YO males perish • __________________narrowing of foreskin of penis and misplaced urethral openings • _______________________-failure of full descent of testes phimosis cryptorchidism • _______________=period ~11-13---taking another 2 years for dependable ovulation • Most common problem in females are infection-sometimes caused by STD’s • Male inflammatory conditions include _______________________,maybe following STD transmission • ______________-inflammation of testes….maybe following STD or mumps • Neoplasms a danger in both genders orchiditis • Women reach peak reproductive abilities @ late 20’s,estrogen declines eventually producing________________-producing a ceasing of menses—irritability and mood changes can accompany • Dangers can accompany HRT • Its all downhill…! Urethritis,prostatitis,epi • Puberty @ 10-15 yrs. didymitis puberty menopause