Ethics and Informed Consent - Appalachian State University

Ethical Concerns with
Providing Informed Consent
Bob Hill, Ph.D.
Department of Psychology
Appalachian State University
ASU Summer Psychotherapy Institute
2004
Bob Hill Contact Info
Email: hillrw@appstate.edu
Web site: www1.appstate.edu/~hillrw
Practice Areas of Greatest
General Legal Risk
Failure to obtain/document informed consent
Client Abandonment
Marked departure from established therapeutic practice
Practicing beyond scope of competency
Misdiagnosis
Repressed or False Memory
Multiple Relationships with clients
Failure to control a dangerous client
Corey, Corey & Callanan (2003) Issues and Ethics in the
Helping Professions
Informed Consent:
Purpose for Clients
To be informed about therapy
To make autonomous, voluntary decisions regarding participation
To understand benefits and risks of treatment (or assessment)
To understand alternatives to therapy
APA Code
Regarding Informed Consent:
“Psychologists inform clients/patients as early as is feasible in the therapeutic relationship about the nature and anticipated course of therapy, fees, involvement of third parties, and limits of confidentiality and provide sufficient opportunity for the client/patient to ask questions and receive answers”
(10.01)
Capacity for Informed Consent
Client Capacity- to make informed decisions (if not, involve parent/guardian)
Comprehension- provide clear information and check client’s understanding
Voluntariness- client is consenting freely and are free to withdraw
– When services are court mandated, inform about services, and any limits of confidentiality beforehand
If Limited Client Capacity
APA Code: “psychologists nevertheless
(1) provide an appropriate explanation,
(2) seek the individual's assent,
(3) consider such persons' preferences and best interests, and
(4) obtain appropriate permission from a legally authorized person,
– if such substitute consent is not (available) psychologists take reasonable steps to protect the individual's rights and welfare. “ (3.10)
Educating About Informed Consent
Encourage Client’s questions about Tx
Provide ongoing opportunities to raise questions about Tx, including expectations
– Clients do not comprehend informed consent after an initial session with a signed form (Welfel, 2002)
– Informed consent can be a means of sharing power with client- developing a collaborative relationship
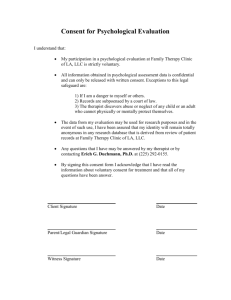
Written Informed Consent
Written (rather than verbal) informed consent provides:
Consistent documentation of informed consent
Ease of administering informed consent
Standardization of content of informed consent
Now the “community standard”
Checklist for Informed Consent
Overview: 16 point Checklist for content of
Informed consent
Derived from various sources (see refs.)
Not exhaustive
Needs modifying for particular settings
Checklist for Informed Consent
1) Therapist Rolewhat will therapist provide
(psychotherapy) a) Therapy Orientationbrief explanation of type of therapy employed:
(e.g. Cognitive Behavioral Tx, Interpersonal)
Consent Checklist Cont.
b) Anticipated Length of treatment
- Provide expectation consistent with preferred intervention strategy about course of treatment
– Discuss any agency or third party payer limitation
– Clients often have mistaken expectations about length of treatment
Case Illustration: Length Tx
Rosemary calls for help with chronic back pain and depression, hoping hypnosis will help. She has traditionally relied on physicians, and expects 1-2 sessions.
When should therapist provide realistic description of treatment duration?
What are risks of “rosey” expectations?
Consent Checklist Cont.
c) Recognized techniques and procedures if Not using generally recognized procedure, inform client about developing nature of treatment and potential risks
A recognized procedure will have empirical evidence documenting usefulness
Describe alternative treatments available
(e.g. self-help groups, other professional practitioners)
Consent Checklist Cont.
d) Therapist Availability
Describe limits to availability
Provide office number and expectation for return calls
Emergency Number (where therapist can sometimes be reached if desired)
Other Emergency number (local hospital, mental health)
Consent Checklist Cont.
2) Voluntary Participationclient voluntarily agrees to treatment and can terminate without penalty
Consent Checklist Cont.
3) Risks Associated with treatmenttherapy may not lead to improvement or anticipated results therapy may impact current relationships therapy may involve psychiatric consultation therapy may be emotionally painful at times
Other risks?
Case: Therapy Makes it Worse
After 4 sessions of therapy for depression and GAD, Stella reports that she feels worse than when she started, and describes crying spells, pessimism and relationship distress.
Should the client be surprised?
Should the therapist discontinue treatment?
Therapist response?
Consent Checklist Cont.
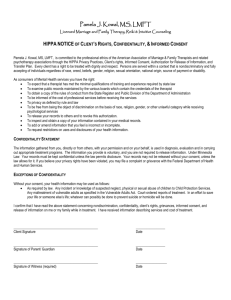
4) Confidentiality
– Information presented during therapy is private and confidential
– Therapist has professional and legal duty to safeguard information
Consent Checklist Cont.
5) Limits on Confidentiality a) suspected child abuse, elder abuse, or dependent adult abuse b) When threat to injure or kill oneself is communicated c) “Tarasoff ”situations where serious threat to a reasonably well-identified victim is communicated
Consent Checklist Cont.
5) Limits on Confidentiality Cont.
d) client signs release providing access to
Third party payer e) client signs release for records if involved in litigation (or other matters): discuss possibilities of legal involvements f) records (and notes on sessions) and phone calls can be subject to court subpoena
Consent Checklist Cont.
Limits on Confidentiality Cont.
g) Couple, family, and group work provide limits
(discretion encouraged & exercised) h) Consultation“I may at times speak with professional colleagues about our work without asking permission” i) Clients under 18 do not have full confidentiality from their parents
Consent Checklist Cont.
Limits on Confidentiality Cont.
j) Cell phones, portable phones, faxes, and emails are used on some occasions and All electronic communication may compromise confidentiality k) Disguised use of client material for teaching purposes
Case Experience with Need to
Break Confidentiality?
E.g. Involuntary hospitalization
E.g. Contacting DSS to report allegation of child abuse
Anecdotal dilemmas?
Consent Checklist Cont.
6) Fees
Describe fees for specific services
Describe how collected ( e.g. billed, collected at beginning of session)
7) Insurance Reimbursement
Co-payment responsibilities
What responsibility will therapist take?
Discuss disclosure of diagnosis to insurance Co.
Consent Checklist Cont.
8) Credentialsa) education b) license- with name of licensing Board
(e.g. NC Psychology Licensing Board) c) if trainee, describe status and supervision
Agencies with trainees may wish to provide a handout describing trainees and credentials of staff
Consent Checklist Cont.
9) Ethical and professional Guidelines
• Under what standards does therapist practice. Provide source of standards. (e.g. APA Ethical Code)
•For your purposes APA code available: web APA.org/ethics
Consent Checklist Cont.
10) Cancellation Policy
Including notice and fee required
11) Affiliation with other Practitioners
Describe independence or relationship with others in office suite
12) Supervisory Relationship
Describe any required supervisory relationship
Provide supervisors name and credentials
Case Illustration: Supervision
Ms. Real, an LPA, provides a handout to new clients, describing her practice, including the name and credentials of her supervisor. Occasionally clients decline her services, because they know her supervisor socially, or professionally, and want greater privacy.
What if she omitted that supervisory disclosure?
Consent Checklist Cont.
13) Disputes and Complaints a) how will fee and other disputes be resolved?
b) consider Agreement for Arbitration (rather than court) c) Client agrees to pay collection or legal costs?
Consent Checklist Cont
14) Contacts Permission:
Obtain permission and names, phone numbers of persons (family or friends) to contact in case of emergency (like suicidal, or manic impaired)
Consent Checklist Cont.
15) Clients Signature a) under sentence describing agreement, opportunity to ask questions, and satisfaction with answers
16) Therapists Signature a) with sentence documenting discussion of diagnosis and treatment plan with client and assurance of mental capacity for consent
Sample Therapist Sig.
Statement of the Therapist
This document was discussed with the client and questions regarding fees, diagnosis, and treatment plan were discussed. I have assessed the client’s mental capacity and found the client capable of giving an informed consent at this time.
Date________________ and Initial of Therapist
__________.
Scenario: No Informed
Consent
Paul Smith, reads the standard informed consent document presented by Dr. Hill and declines to sign because
He objects to the therapist consulting with colleagues
He objects to a documented diagnosis
He objects to information being provided to third party payer
Strategies to Provide Written
Informed Consent
Client Information Brochure
– With detailed information about Tx and contains the Informed Consent Checklist
Client Question List
Structure for client to interview psychologist e.g. What will we do in therapy?
How will I know when I am better?
How do I reach you in emergency?
Strategies to Provide Written
Informed Consent
Psychotherapy Contract or
Consent to Treatment Form
– Rights and Responsibilities of Client and
Therapist outlined
Consider using multiple strategies to provide informed consent
Written strategies require supplemental verbal discussion
(Welfel, 2002)
Case Illustration: Written Form
Dr. Besness trained his receptionist to provide clients with an informed consent document in the waiting area, and to review a protocol of points with them prior to intake. Dr. B. thus rarely found the need to discuss informed consent issues with clients.
Is this practice consistent with current standards?
Guidelines for Ethical
Practice: Consent
1) Use a written informed consent a) Document review of informed consent with client
2) Educate and review client’s role in consent process as needed
3) Include the Features listed in Checklist
4) Remember to include HIPPA Informed
Consent
HIPAA Practices
Provide separate or additional notice of
Privacy Practices for Protected Health
Information
– (often a lengthy document itself) separate or additional Informed Consent statement specific to use and disclosure of
Protected Health Information
Close: Informed Consent
Opportunity to address Informed Consent
Concerns or Experiences
Dual Relationships
When a professional holds 2 or more relationships with a client at the same time or sequentially
For example:
Therapist and friend
Therapist and instructor
Therapist and business partner
Therapist and sexual partner
Dual Relationships
Among the 12 most common areas where therapists leave themselves open to law suits and licensing board complaints are:
A) Sexual Relationship with client (whether current or former client)
B) Business Relationships with client
C) Out of Office Contact with client
(Caudil, B. Malpractice & Licensing Pitfalls for Therapists: A
Defense Attorney’s List)
Dual Relationships: Sexual
Sexual intimacy with a client is one of the most common reasons for malpractice suits
Sexual intimacy prohibited in the codes of most professional organizations
Sexual intimacy with former clients also prohibited “except in the most unusual of circumstances” (APA Ethics Code, 2002)
Dual Relationships: Non-Sexual
Recent trend with state licensure boards has been to prohibit all dual relationships
Intent of banning dual relationships has been to prohibit any dual relationship that:
1) may impair the judgment of the therapist
2) may be potentially exploitive of clients
Such a broad ban has been controversial
Dual Relationships
Lazarus (1994) has admitted to socializing with clients, playing tennis, taking walks, accepting gifts and giving gifts
Lazarus suggested that the accountable therapist must consider:
– The risks of harming a client
– Possible conflicts of interest
– If dual relationship may impair therapist’s judgment
– If the client’s rights or autonomy will be infringed
– If the therapist will gain a personal advantage
Dual Relationships: Data on
Frequency
A survey of 4,800 psychologists, psychiatrists and social workers re beliefs and behaviors about Dual Relationships
(Borys & Pope, (1989) Professional Psychology: Research and
Practice)
Dual Relationships: Data
Results of survey of Behaviors (N=1021)
1= no client 2 = few clients, 3= some clients, 4 = most clients, 5 = all clients
Accepted a client's invitation to a special occasion
1 2 3 4 5
64.0 28.0 3.3 2.4
1.4
Accepted a service or product as payment for therapy
82.6 13.9 2.8
0.2
0.1
Became friends with a client after termination
69.0 26.5 3.2
0.2
0.3
Provided therapy to an employee
87.5 9.3
1.7
0.3
0.2
Dual Relationships: Data
1 2 3 4
Engaged in sexual activity with a client after termination
95.3
3.9
0.0
0.0
Went out to eat with a client after a session
87.4
10.5
0.9
.2
Disclosed details of current personal stresses to a client
60.1
30.7
7.4
.2
Bought goods or services from a client
77.6
20.5
1.1
0.1
Provided individual therapy to a relative, friend, or lover of an ongoing client
38.0
36.0
21.6
2.1
Dual Relationships: Friendships
Do social relationships interfere with current therapy relationships?
Defenders of social relationships suggest that sometimes a “blended” role can assist a client. Examples?
Most therapists would agree that social relationships with clients are unwise
Senario: Friendships
Senario: A member of your church (or local civic group) makes an appointment and requests therapy services.
– What are your concerns?
– Do you share your concerns with the client?
– What options do you have?
Guidelines for Friendships
Maintain clear boundaries with clients regarding potential blended roles (e.g. therapist/coach of client’s son)
Former clients may need therapy in future
(rather than a friendship)
Power differential difficult to change
Safest to avoid social relationships with former clients
Dual Relationships: Bartering
Barter: is the acceptance of goods, services, or other non-monetary remuneration
“Psychologists may barter only if
(1) it is not clinically contraindicated, and
(2) the resulting arrangement is not exploitative” (APA, 2002)
Dual Relationships: Bartering
Senario
A client of 14 sessions advises that she has lost her insurance and can not continue. She asks if therapist is willing to exchange childcare for therapy.
1) Could this be an ethical agreement in the eyes of professional peers?
2) What if the offer was dry-cleaning at her family business, or bulk meat from her butcher business?
1)
2)
3)
4)
5)
6)
Bartering: Guidelines for
Practice
Will barter put you at risk for impaired professional judgment, or negatively impact therapy?
Better to exchange goods than services
Determine value of goods or services in collaborative fashion
Determine appropriate length of time for barter
Document arrangement, including value of goods, end date, and have client sign
If misunderstanding develops, use mediator
Dual Relationships: Gifts
Few ethics codes address the topic of gifts
However, AAMFT (2001): “Marriage and family therapists do not give or receive from clients (a) gifts of substantial value or
(b) gifts that impair the integrity or efficacy of the therapeutic relationship”
Clearly, lavish gifts represent ethical problem, but small personal gifts may not
Dual Relationships: Gifts
Senario: A client presents his therapist with a amber pendant and describes his belief that the therapy process has changed his life for all time. He asks the therapist to accept his gift in appreciation and celebration of his treatment progress.
What concerns bear on this decision to accept the gift or not?
1)
2)
3)
4)
5)
Dual Relationship: Gift
Evaluation
What is the monetary value of the gift?
What are the clinical implications for accepting or rejecting the gift?
When in the therapy process is the gift occurring?
What are the therapists motivations for accepting or rejecting the gift?
What are the cultural implications of offering a gift?
1)
2)
3)
4)
5)
Dual Relationship: Gift
Guidelines
Consider putting a statement in informed consent declaring a policy of not accepting gifts
Refuse gifts that are expensive, that suggest a social relationship
Refuse gifts occurring early in therapy
Consider discussing clinical implications of gift with client
Develop clear boundaries regarding gifts to practice with clients
Appalachian Summer
Psychotherapy Workshops 2005
June 2005 at Appalachian State
University, Boone, NC
Presented by Faculty from the Department of Psychology, Appalachian State Un.
Co-sponsored by NW AHEC
Mental Health Education (3 CE Credits
Offered for each Workshop)
References
Corey, Corey & Callanan (2003) Issues and
Ethics in the Helping Professions (6 th Ed.)
Hedges (2000). Facing the Challenge of Liability in Psychotherapy, (Aronson).
Nagy (2000). Ethics In Plain English (APA).
Wefel (2002). Ethics in Counseling and
Psychotherapy (2 nd Ed, Brooks/Cole).
http://kspope.com/ethics/index.php