Morphology of Coagulation necrosis
advertisement

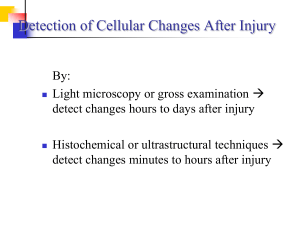
Cell injury By Dr. Abdelaty Shawky Dr. Gehan Mohamed Fatty Change * Definition: abnormal accumulation of triglycerides within parenchymal cells. * Site: liver, most common site which has a central role in fat metabolism. it may also occur in heart as in anaemia or starvation (anorexia nervosa) Other sites: skeletal muscle, kidney and other organs. * Causes: 1. 2. 3. 4. 5. Toxins (most importantly: Alcohol abuse) Diabetes mellitus Protein malnutrition (starvation) Obesity Anoxia * The significance of fatty change: Depends on the severity of the accumulation. Mild: it may have no effect . Severe: form, fatty change may precede cell death, and may be an early lesion in a serious liver disease called nonalcoholic steatohepatitis * Is Fatty liver reversible? • Fatty change is reversible except if some vital intracellular process is irreversibly impaired . * Prognosis of Fatty liver: • In Mild cases: 3% will develop cirrhosis • Moderate to sever: inflammation, degeneration in hepatocytes, fibrosis (30% develop cirrhosis). Other form of accumulation • Cholesteryl esters: • These give atherosclerotic plaques with their characteristic yellow color and contribute to the pathogenesis of narrowing of the blood vessels. • This is called atherosclerosis Accumlation of Exogenous pigment • Tattooing: Indian ink pigments produce effective tattoos because they are engulfed by dermal macrophages which become immobilized and permanently deposited. • Anthracosis: inhalation of carbon dust particles. When inhaled, it is phagocytosed by alveolar macrophages and transported through lymphatic channels to the regional tracheobronchial lymph nodes. Anthracosis Accumulation of Endogenous pigments Hemosiderin ( iron) is a hemoglobin-derived granular pigment that is golden yellow to brown and accumulates in tissues when there is a local or systemic excess of iron. Iron is normally carried by specific transport proteins, transferrins. In cells, it is stored in association with a protein, apoferritin, to form ferritin micelles. Ferritin is a constituent of most cell types. When there is a local or systemic excess of iron, ferritin forms hemosiderin granules. Hemosiderosis * Causes of Hemosiderosis: 1. Increased absorption of dietary iron 2. Impaired utilization of iron 3. Hemolytic anemias 4. Repeated blood transfusions (the transfused red cells constitute an exogenous load of iron). 5. Hereditary hemochromatosis with tissue injury including liver fibrosis, heart failure, and diabetes mellitus . Although hemosiderin accumulation is usually pathologic, small amounts of this pigment are normal. Where? in the mononuclear phagocytes of the bone marrow, spleen, and liver. Why? there is extensive red cell breakdown. Hemosiderosis (systemic overload of iron) It is found at first in the mononuclear phagocytes of the liver, bone marrow, spleen, and lymph nodes and in scattered macrophages throughout other organs. With progressive accumulation, parenchymal cells throughout the body (principally the liver, pancreas, heart, and endocrine organs) will be affected Hemosiderin H&E: golden brown pigment Prussian blue stain: blue Lipofuscin • “Wear-and-tear pigment" is a brownish-yellow granular intracellular material that seen normally in a variety of tissues (the heart, liver, and brain) as a function of age or atrophy. • Consists of complexes of lipid and protein that derive from the free radical-catalyzed peroxidation of lipids of subcellular membranes. • It is not injurious to the cell but is important as a marker of past free-radical injury. • The brown pigment when present in large amounts, imparts an appearance to the tissue that is called brown atrophy. Pathological calcification • It implies the abnormal deposition of calcium salts in tissues rather than bone and teeth. • It has 2 types: Dystrophic calcification: When the deposition occurs in dead or dying tissues e.g. areas of necrosis or atherosclerotic patches. it occurs with normal serum levels of calcium Metastatic calcification: The deposition of calcium salts in normal tissues It almost always reflects hypercalcemia. Irreversible cell injury * Mechanism: • • • Persistent or severe injury (hypoxia) takes the cell to the "point of no return" where the injury becomes irreversible. At this point no intervention can save the cell. Two phenomenon characterize irreversible injury: 1. Mitochondrial damage. 2. Damage to the structural integrity of plasma membrane. • Calcium plays a major role in irreversible injury. 1. Mitochondrial damage: • Marked reduction in ATP production leads to mitochondrial damage results in formation of high conductance channels (Mitochondrial Permeability Transition (MPT) channels) which Release cytochrome c into cytosol which is a trigger for apoptosis. MITOCHONDRIAL DYSFUNCTION or INJURY ↓ATP production H+ Mitochondrial Permeability Transition (MPT) Cytochrome C Apoptosis 2. Damage to plasma membrane: • Due to: – Decreased production of membrane phospholipids: due to mitochondrial dysfunction and decreased ATP production. – Loss of membrane phospholipids: due to the action of phospholipases. – Damage to cytoskeleton due to the action of proteases. * Consequences of membrane damage: • Mitochondrial membrane: – Formation of MPT (mitochondrial permeability transition channels). – Release of cytochrome c activates apoptosis. • Plasma membrane: – Loss of osmotic balance. – Influx of fluids and ions. – Loss of proteins, enzymes, RNA. • Lysosomal membrane: – Leakage of lysosomal enzymes and their activation • RNases, DNases, proteases, phosphatases, glucosidases. – Enzymatic digestion of cell components – Cell death by necrosis. * Role of calcium in irreversible cell injury: • Increased cytosolic calcium: Leads to : 1. Enzyme activation: ATPases: Hasten ATP depletion Phospholipases : cause membrane damage increased permeability. Proteases damages membrane and structural proteins Endonucleases damages nuclear chromatin and DNA, causing fragmentation (karyorrhexis). 2. Increased mitochondrial permeability : release of cytochrome c (activates apoptosis) INJURIOUS AGENT Ca 2+ Ca 2+ Ca 2+ Increased Cytosolic Ca2+ ATPase ATP Phospholipase Phospholipids Protease Disruption of membrane & cytoskeletal Proteins Endonuclease Nuclear Chromatin damage Morphology of irreversible cell injury Light microscopy of irreversible cell injury • Pyknosis = Shrinkage and darkening of the nucleus. • Karyorrhexis = fragmentation and breakdown of the nucleus, (into "nuclear dust"). • Karyolysis = dissolution of the nucleus. Karyorrhexis Nuclear pyknosis Karyolysis * Types of cell death: • Necrosis: local death of a group of cells within the living body. • Apoptosis: genetically controlled programmed single cell death. Some important terms! • Autolysis: degradation of cell and its constituents caused by its own enzymes. • Heterolysis: degradation of cell and its constituents by enzymes derived from sources extrinsic to the cell (e.g. neutrophils, bacteria). • Putrefaction: lysis of dead tissue by bacterial enzymes. Morphological types of necrosis: 1. 2. 3. 4. Coagulation necrosis. Liquefactive necrosis. Caseation necrosis. Fat necrosis. A. Traumatic. B. Enzymatic . 5. Fibrinoid necrosis. 6. Gangrenous necrosis. 7. Gummatous necrosis. Coagulative necrosis * Mechanism: – Denaturation and coagulation of structural and enzymatic proteins due to intracellular acidosis. • Denaturation of lysosomal enzymes by intracellular acidosis prevents autolysis. • Preserving cell outlines and tissue architecture. * Etiology: a. ischemia (secondary to atherosclerosis thrombus formation). The most common cause. b. Heavy metal poisoning (lead). c. Irradiation. * Organs affected: Commonly seen in solid organs like Heart, kidney, spleen Infarction – Refers to a localized area of tissue necrosis resulting from loss or reduction in blood supply (= ischemic necrosis). – The dead tissue is called an infarct. • Coagulative necrosis is the type of necrosis associated with infarction except in infarction of brain. • In Brain: – Lack of good structural support. – Cells rich in lysosomal enzymes result in liquefactive necrosis. Infarction of the spleen (ischemic coagulative necrosis) * Morphology of Coagulation necrosis: * GROSS APPEARANCE: – The necrotic tissue appears firm and dry. – Cut surface: grey white. * MICROSCOPY: – Loss of the nucleus but preservation of cellular shape. – Increased cytoplasmic eosinophilia. Area of necrosis Area of Necrosis Preservation of cellular shape. Increased cytoplasmic eosinophilia Good luck