one year outcomes after medical therapy, percutaneous
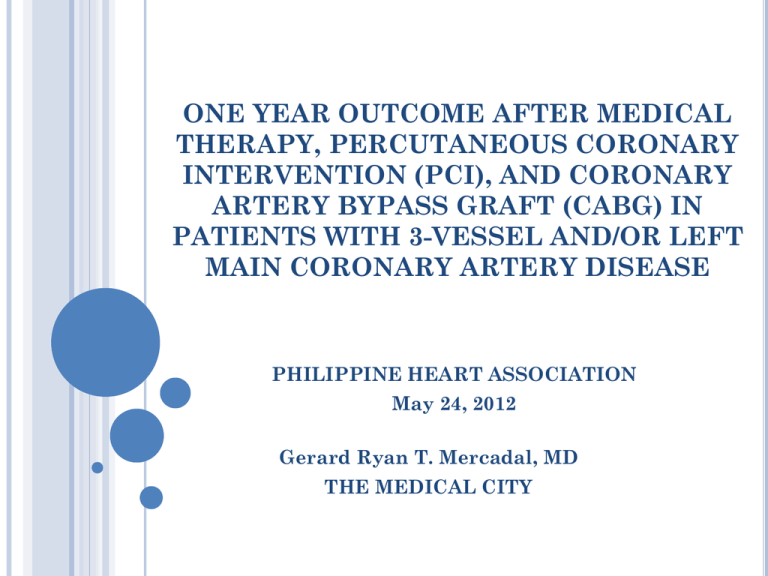
ONE YEAR OUTCOME AFTER MEDICAL THERAPY, PERCUTANEOUS CORONARY INTERVENTION (PCI), AND CORONARY ARTERY BYPASS GRAFT (CABG) IN PATIENTS WITH 3-VESSEL AND/OR LEFT MAIN CORONARY ARTERY DISEASE PHILIPPINE HEART ASSOCIATION May 24, 2012 Gerard Ryan T. Mercadal, MD THE MEDICAL CITY
OBJECTIVES
PRIMARY OBJECTIVES
•Investigate the one-year clinical outcomes of patients with three vessel and/or left main coronary artery disease who underwent medical therapy, percutaneous coronary intervention and coronary artery bypass graft, admitted at The Medical City from January to December 2010 .
SPECIFIC OBJECTIVES
• To identify patients with three-vessel and/or left main coronary artery disease (CAD) on coronary angiography performed at the Cardiac Catheterization Laboratory of The Medical City from January to December 2010.
• To categorize these patients into those who had medical therapy (MT), percutaneous coronary intervention (PCI) and coronary bypass graft (CABG).
SPECIFIC OBJECTIVES
•To determine and compare the baseline characteristics of patients in the three treatment group including risk factors and indication for coronary angiography.
•To identify and assess the angiographic characteristics of the three treatment groups consisting of SYNTAX score, vessels and number of lesions involved and presence of total occlusion.
SPECIFIC OBJECTIVES
•To determine and assess the maintenance medications given to patients in each group.
•To identify and compare the clinical events and outcomes of these CAD patients in hospital, 30 days, 6 months and 12 months after, according to treatment groups and SYNTAX category.
METHODOLOGY
MEDICAL CORONARY ANGIOGRAPHY FROM JAN-DEC 2010
MEDICAL AND CATHETERIZATION RECORDS
3-VESSEL AND/OR LEFT MAIN INVOLVEMENT CABG PCI
BASELINE CHARACTERISTICS
•gender •age •body mass index (kg/m 2 (mg/dl) ) •risk factors •creatinine clearance •ejection fraction (%) •indication for coronary angiography
ANGIOGRAPHIC CHARACTERISTICS
•SYNTAX SCORE •Vessels and number of lesions involved •Presence of total vessel occlusion
SYNTAX SCORE
•algorithm available on the SYNTAX score website ( www.syntaxscore.com
) •each coronary lesion producing > 50% luminal obstruction, in vessels > 1.5 mm, was separately scored and added to provide the overall SYNTAX score.
EXCLUSION CRITERIA
• Previous percutaneous coronary intervention (PCI) • Severe hepatic or renal disease • Neutropenia or thrombocytopenia • Intolerance or contraindication to acetylsalicylic acid or thienopyridines • Need for concomitant major surgery • Life-limiting major concomitant non-cardiac diseases
FOLLOW-UP
Review of outpatient records Maintenance medications Phone calls Procedures or treatment in other institutions
CLINICAL ENDPOINTS
MAJOR ADVERSE CARDIAC AND CEREBROVASCULAR EVENTS (MACCE) In hospital 30 days 6 months 12 months DEATH FROM ANY CAUSE (CARDIAC, CARDIOVASCULAR AND NON-CARDIOVASCULAR) STROKE MYOCARDIAL INFARCTION REPEAT REVASCULARIZATION
SECONDARY ENDPOINTS
In hospital 30 days 6 months 12 months Other cardiac and non cardiac events Incidence of angina and heart failure symptoms
STATISTICAL ANALYSIS
STATISTICAL ANALYSIS
• Microsoft Office and SPSS v16 • Categorical data: frequencies and percentages ( Chi-square test) • Numerical data: mean ± standard deviation (SD) (One Way Anova).
• 12-month rates of MACCE according to the treatment group and SYNTAX score classification: Chi-square test • Cumulative survival function and event rates: Kaplan–Meier method
RESULTS
MEDICAL (N=17 ) CORONARY ANGIOGRAPHY FROM JAN-DEC 2010 (N= 616 PATIENTS) CABG (N=33) 3-VESSEL AND/OR LEFT MAIN INVOLVEMENT (N= 75) PCI (N=17) NO DEFINITE MANAGEMENT/ LOST TO FOLLOW-UP (N=8)
TABLE I. Baseline characteristics of patients with 3-vessel arterial disease and/or left main
involvement on coronary angiography performed at the Cardiac Catheterization Laboratory of the Cardiovascular Center of The Medical City from January to December 2010.
Male Age Body mass index RISK FACTORS Hypertension Diabetes Previous myocardial infarction Dyslipidemia Family history coronary artery disease of Smoker Peripheral disease artery Chronic obstructive pulmonary disease Previous cerebrovascular accident Creatinine (mg/dl) clearance, Ejection fraction (%) MEDICAL (N=17)
12 (70.6%)
62.9 ± 7.9
25.3 ± 4.2
15 (88.2%) 10 (58.8%) 5 (29.4%) 6 (35.3%) 3 (17.6%) 6 (35.3%) 0 (0%) 0 (0%) 2 (11.8%) 57.4 ± 20 61.9 ± 20.4
CABG (N=33)
28 (84.8%)
56 ± 7.8
27.2 ± 3.9
28 (84.8%) 23 (69.7%) 5 (15.2%) 12 (36.4%) 13 (39.4%) 18 (54.5%) 2 (6.1%) 2 (6.1%) 4 (12.1%) 64.1 ± 22.3
59.5 ± 19.8
PCI (N=17)
11 (64.7%)
60.2 ± 11.9
24.5 ± 3.9
13 (76.5%) 9 (52.9%) 1 (5.9%) 4 (23.5%) 5 (29.4%) 8 (47.1%) 3 (17.6%) 2 (11.8%) 0 (0%) 70.7 ± 36.3
65.3 ± 14.7
P-VALUE (< 0.05)
0.236
0.035
0.081
0.627
0.474
0.173
0.637
0.286
0.434
0.134
0.351
0.326
0.345
0.607
MEDICAL (N=17) CABG (N=33) PCI (N=17) INDICATION FOR CORONARY ANGIOGRAPHY NSTEMI STEMI Cardiogenic Shock Stable angina Unstable angina Congestive heart Failure Positive treadmill test Segmental wall motion abnormality on 2d echo Positive CT Angiography Positive stress echo Positive nuclear viability study 4 (23.5%) 9 (27.3%)
3 (17.6%) 4 (12.1%) 0 (0%)
4 (23.5%)
1 (5.9%) 1 (5.9%) 1 (3%) 5 (15.2%) 5 (15.2%) 1 (3%) 3 (17.6%)
5 (29.4%)
1 (5.9%) 2 (11.8%) 2 (11.8%) 1 (5.9%) 2 (11.8%) 1 (3%) 1 (5.9%) 0 (0%) 2 (6.1%) 1 (3%) 1 (5.9%) 0 (0%) 3 (9.1%) 1 (3%) 1 (5.9%) 2 (11.8%) 0 (0%) 0 (0%) 0 (0%)
P-VALUE (< 0.05)
0.951
TABLE II. Angiographic characteristics of patients with 3-vessel arterial
disease and/or left main involvement on coronary angiography
SYNTAX score MEDICAL (N=17)
33.6 ± 17
CABG (N=33) PCI (N=17) TOTAL (N=67)
40.1 ± 11.9 34.4 ± 13.6 37 ± 13.9
P VALUE (<0.05)
0.197
No. of lesions -3 vessel
0.671
-1 vessel with left main -2 vessel with left main -3 vessel with left main Total occlusion
13 (76.5%) 1 (5.9%) 0 (0%) 3 (17.6%) 10 (58.8%) 25 (75.8%) 1 (3%) 2 (6.1%) 5 (15.2%) 24 (72.7%) 14 (82.4%) 0 (0%) 2 (11.8%) 1 (5.9%) 6 (37.5%) 52 (77.6%) 2 (3%) 4 (6%) 9 (13.4%) 40 (60.6%) 0.060
TABLE III. Maintenance medications after hospital discharge of patients
with 3-vessel arterial disease and/or left main involvement on coronary angiography.
MEDICAL (N=17) CABG (N=33) PCI (N=17) P-VALUE (< 0.05) MEDICATIONS Aspirin 14 (82.4%) 21 (67.7%) 16 (100%) 0.032
Clopidogrel Statin 16 (94.1%) 15 (46.9%) 15 (93.8%)
17 (100%) 29 (90.6%) 16 (100%)
0.000
0.198
Angiotensin receptor blocker B-blockers Nitrates
9 (52.9%) 23 (71.9%) 11 (64.7%) 20 (62.5%) 8 (50%) 12 (70.6%) 23 (71.9%) 11 (68.8%) 11 (68.8%) 0.237
0.975
0.913
CLINICAL OUTCOMES
TABLE IV. Clinical events and outcomes according to treatment group
of patients with 3-vessel arterial disease and/or left main involvement on coronary angiography from January to December 2010 in hospital, 3, 6 and 12 months after treatment/procedure
MAJOR ADVERSE CARDIAC AND CEREBROVASCULAR EVENTS (MACCE) ACCORDING TO TREATMENT GROUP IN HOSPITAL, 30 DAYS, 6 AND 12 MONTHS AFTER TREATMENT/PROCEDURE
Medical (n=17) CABG (n=33) PCI (n=17) Total (n=67) p-value (< 0.05)
MACE IN HOSPITAL Death From cardiac causes From cardiovascular Causes From non cardiovascular causes Stroke MI Repeat CABG Repeat PCI
0 (0%) 0 0 0 0 0 0 0 0 3 (9.1%) 2 2 0 0 1 0 0 0 1 (5.9%) 1 0 0 1 0 0 0 0 4 (6%) 3 2 0 1 0 2 0 0 0.437
MACE 30 DAYS AFTER TREATMENT/PROCEDURE Lost to follow-up Medical (n=17)
0 (0%) 0 (0%)
Medical (n=17)
1 (5.9%)
MACE 6 MONTHS AFTER TREATMENT/PROCEDURE Death From cardiac causes From cardiovascular Causes From non cardiovascular causes Stroke MI Repeat CABG Repeat PCI
1 1 0 0 0 1 0 0 0 1 0 0 0 0 0
CABG (n=31)
0 (0%) 0
PCI (n=16)
0 (0%) 6 (19.4%) 0 (0%)
CABG PCI (n=25)
1 (4%)
(n=16)
0 (0%) 0 0 0 0 0 0 0 0 0 2 0 0 1 1 0 0
Total (n=64)
0 (0%) 6 (9.4%)
Total (n=58)
2 (3.4%)
P Value P Value
0.639
MACE 12 MONTHS AFTER TREATMENT/PROCEDURE Death From cardiac causes From cardiovascular Causes From non cardiovascular causes Stroke MI Repeat CABG Repeat PCI Medical (n=16)
1 (6.3%) 1 1 0 0 0 1 0 0
CABG (n=25)
0 (0%) 0 0 0 0 0 0 0 0
PCI (n=16)
1 (6.3%) 0 0 0
Total (n=57)
2 (3.5%)
P- Value (<0.05)
0.445
1 1 0 0 0 1 0 1 0 0 2 0 1
OTHER CARDIAC AND NON CARDIAC EVENTS
TABLE V. Other cardiac and non-cardiac clinical events and
symptoms according to treatment group from hospital admission until 12 months after discharge.
(MULTIPLE) arrhythmia pneumonia Medical (n=17) 1 (6.3%)
0 (0%)
CABG (n=33) 5 (15.2%)
3 (9.1%)
PCI (n=17) 3 (17.6%)
3 (17.6%)
Total (n=67) 8 (12.1%)
4 (6.1%)
P value < 0.05
0.247
0.10
sepsis urinary tract infection CARDIAC SYMPTOMS Angina Failure symptoms
0 (0%) 0 (0%)
5 (29.4%)
3 (17.6%) 0 (0%) 0 (0%)
3 (9.1%)
0 (0%) 2 (11.8%) 1 (5.9%)
1 (5.9%)
1 (5.9%) 1 (1.5%) 0 (0%)
9 (13.4%)
4 (5.9%) 0.225
0.123
0.095
TABLE VI. Clinical events and outcomes according to SYNTAX category of patients with 3-
vessel arterial disease and/or left main involvement on coronary angiography from January to December 2010 in hospital, 3, 6 and 12 months after treatment/procedure
MAJOR ADVERSE CARDIAC AND CEREBROVASCULAR EVENTS (MACCE) ACCORDING TO SYNTAX CATEGORY IN HOSPITAL, 30 DAYS, 6 AND 12 MONTHS AFTER TREATMENT/PROCEDURE
LOW INTERMEDIATE (n=12) (n=15) HIGH (n=40) Total (n=67) p-value (< 0.05)
MACCE IN HOSPITAL
0 (0%) 1 (6.7%) 3 (7.5%) 4 (6%) 0.624
Death From cardiac causes From cardiovascular Causes From non cardiovascular causes Stroke MI Repeat CABG Repeat PCI
0 0 0 0 0 0 0 0
1
0 0 1 0 0 0 0
2
2 0 0
1
0 0 0 3 2 0 1 0 0 0 0
LOW (n=12) INTERMEDIATE (n=14) HIGH n=38) Total (n=64) P-Value (<0.05) MACCE 30 DAYS AFTER TREATMENT/PROCEDURE Lost to follow-up MACCE 6 MONTHS AFTER TREATMENT/PROCEDURE Death From cardiac causes From cardiovascular causes From non- cardiovascular causes Stroke MI Repeat CABG Repeat PCI
0 (0%) 0 (0%) LOW (n=12) 1 (8.3%)
1
1 0 0 0
1
0 0 0 (0%) 2 (14.3%) INTERMEDIATE (n=12) 0 (0%) 4 (10.5%) 6 (9.4%) HIGH (n=34) Total (n=58) 1 (2.9%) 2 (3.4%) 0 0 0 0 0 0 0 0 0 (0%) 0 0 0 0 0
1
0 0 0 (0%) 1 1 0 0 0 2 0 0 0.518
LOW (n=11) INTERMEDIATE (n=12) HIGH (n=34) Total (n=57) P-value (<0.05) MACCE 12 MONTHS AFTER TREATMENT/ PROCEDURE Death From cardiac causes From cardiovascular causes From non cardiovascular causes Stroke MI Repeat CABG Repeat PCI
0 (0%) 0 0 0 0 0 0 0 0 0 (0%) 0 0 0 0 0 0 0 0 2 (5.9%)
1
1 0 0 0
2
0
1
2 (3.5%) 1 1 0 0 0 2 0 1 0.496
KAPLAN-MEIER CURVES
A. MAJOR ADVERSE CARDIAC AND CEREBROVASCULAR EVENTS (MACCE)
1.02
Survival Functions 1.00
.98
.96
.94
.92
.90
-2 0 2 4 time (in months) LOG p-value =.9809 6 8 10 12 14 procedure PCI PCI-censored CABG CABG-censored Medical Medical-censored
B. DEATH FROM ANY CAUSE
1.2
Survival Functions 1.0
.8
.6
.4
.2
0.0
-.2
-2 0 2 4 time (in months) LOG p-value =.6516 6 8 10 12 14 procedure PCI PCI-censored CABG CABG-censored Medical Medical-censored
C. MYOCARDIAL INFARCTION
1.2
Survival Functions 1.0
.8
.6
.4
.2
0.0
-.2
-2 0 2 4 time (in months) LOG p-value =.6015 6 8 10 12 14 procedure PCI PCI-censored CABG CABG-censored Medical Medical-censored
A. MAJOR ADVERSE CARDIAC AND CEREBROVASCULAR EVENTS (MACCE)
1.02
Survival Functions 1.00
.98
.96
.94
.92
.90
-2 0 2 time (in months) LOG p-value =.6625 4 6 8 10 12 14 Syntax Score Hi gh Hi gh-censored Intermediate Intermediate -censored Low Low-censored
B. DEATH FROM ANY CAUSE
1.2
Survival Functions 1.0
.8
.6
.4
.2
0.0
-.2
-2 0 2 4 time (in months) LOG p-value =.3356 6 8 10 12 14 Syntax Score Hi gh Hi gh-censored Intermediate Intermediate -censored Low Low-censored
C.MYOCARDIAL INFARCTION
1.2
Survival Functions 1.0
.8
.6
.4
.2
0.0
-.2
-2 0 2 4 6 8 10 time (in months) LOG p-value =cannot be computed 12 14 Syntax Score Hi gh Hi gh-censored Intermediate Intermediate -censored Low Low-censored
DISCUSSION
PRIMARY GOALS OF REVASCULARIZATION FOR PATIENTS WITH CAD
•to improve survival •relieve symptoms
4. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/ AHA Guideline for coronary artery bypass graft surgery: Executive summary: A report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists and Society of Thoracic Surgeons. Journal of the American College of Cardiology 2011; 58 (24):2584-2614
CABG is a class I indication to improve survival in patients with significant left main and/or 3 vessel coronary artery stenosis.
• Percutaneous coronary intervention is another alternative to CABG (Class IIa)… to improve survival in selected patients: • with significant unprotected left main CAD, with unstable angina or non-ST elevation myocardial infarction who are not eligible for CABG, and in acute ST-elevation myocardial infarction (4) .
4. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/ AHA Guideline for coronary artery bypass graft surgery: Executive summary: A report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists and Society of Thoracic Surgeons. Journal of the American College of Cardiology 2011; 58 (24):2584-2614
THE MEDICAL CITY 2010
• 25.37% of 67 patients: PCI •49.25% : CABG •25.37% : Medical therapy
2368 patients with diabetes and multi vessel CAD with stable symptoms •angiographic features had the associated with extent, location, and nature of CAD greatest influence in the decision to select CABG over PCI in these patients. . •introduction of the first generation drug eluting stents (DES) decreased the likelihood of the selection of CABG 6. Kim LJ, King III SB, Kent K, et al. Factors Related to the Selection of Surgical Versus Percutaneous Revascularization in Diabetic Patients With Multivessel Coronary Artery Disease in the BARI 2D (Bypass Angioplasty RevascularizationInvestigation in Type 2 Diabetes) Trial. JACC: Cardiovascular Interventions 2009; 2(5): 384-392
A meta-analysis of 13 randomized trials on 7964 patients comparing PCI with CABG showed a lower risk of death at five-years 0.025) (risk difference (RD) 2.3%, CI 0.29% to 4.3%, p= and eight-years 0.32% to 6.4%, p= 0.03) (risk difference (RD) 3.4%, CI surgery (7) . for patients with multi vessel disease who underwent bypass 7. Hoffman SN, TenBrook Jr JA, Wolf MP, et al. A meta-analysis of randomized controlled trials comparing coronary artery bypass graft with percutaneous transluminal coronary angioplasty: One- to eight-year outcomes. Journal of the American College of Cardiology 2003; 41(8):1293-1304
A meta-analysis of 4 randomized trials in 3051 patients with multi-vessel disease • No difference was noted in the cumulative incidence of death, stroke and myocardial infarction stenting.
between patients who were randomized to CABG versus PCI with • MACCE was higher in the PCI group as demonstrated by a significantly higher rate of revascularization (28.9 versus 7.8%, p <0.001) (8) .
8. Daemen J, Boersma E, Flather M, et al. Long-term safety and efficacy of percutaneous coronary intervention with stenting and coronary artery bypass surgery for multivessel coronary artery disease: A meta-analysis with 5-year patient-level data from the ARTS, ERACI-II, MASS-II, and SoS Trials. Circulation 2008; 118: 1146 54
…PCI added to optimal medical therapy as an initial management did not decrease the risk of death, myocardial infarction or other major cardiovascular events at 4.6 years (9) . On 2 (10) and 3 (11-12) years follow-up, PCI with drug-eluting stents showed similar long-term mortality with CABG for treatment of multi-vessel CAD but with significantly higher rate of revascularization (10-12) . 9. Boeden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary artery disease. N Engl J Med 2007; 356: 1503-1516 10. Pell JP, Walsh D, Norrie J, et al. Outcomes following coronary artery bypass grafting and percutaneous transluminal coronary angioplasty in the stent era: a prospective study of all 9890 consecutive patients operated on in Scotland over a two year period. Heart 2001; 85: 662-666 11. Park DW, Yun SC, Lee SW, et al. Long term mortality after percutaneous coronary intervention with drug-eluting stent implantation versus coronary artery bypass surgery for the treatment of multivessel coronary artery disease. Circulation 2008; 117: 2079-2086 12. Rodriguez AE, Maree AO, Mieres J, et al. Late loss of early benefit from drug-eluting stents when compared with bare-metal stents and coronary artery bypass surgery: 3 years follow-up of the ERACI III registry. European Heart Journal 2007; 28: 2118-2125
At 13 years follow-up , both CABG and PCI showed comparable long-term survival, degree of angina, functional capacity and use of anti-anginal medication (13) . In a study by Boden, et al, they found that group compared to the medical group (9) rates of angina were consistently lower in the PCI .
In our study, cardiac symptoms and failure symptoms on one-year follow-up were comparable between the medical, PCI and CABG group. 9. Boeden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary artery disease. N Engl J Med 2007; 356: 1503-1516
In the final analysis of the ARTS Randomized trial, no significant difference was found in the mortality rate between patients who underwent stenting versus surgery for multi-vessel disease . However, overall MACCE was higher in the stenting group revascularization (14) . because of the increased need for repeat 14. Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N ENGL J MED 2009; 360: 961-72
SYNTAX score •developed to predict outcomes in patients with three vessel and/or left main disease who undergo either CABG or PCI . •SYNTAX trial: in patients who underwent PCI, the rate of major adverse cardiac or cerebrovascular events was significantly increased among patients with high SYNTAX scores (14 ) . 14. Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N ENGL J MED 2009; 360: 961-72
ARTS II trial showed that patients with multi-vessel disease with low SYNTAX score may be adequately treated with PCI while CABG may be more beneficial for those patients with high SYNTAX scores (15) . In a randomized study of 1800 patients, rates of MACCE was similar among patients with low and intermediate scores in the CABG and PCI groups while in the patients with high score, the adverse event rate was significantly increased in the PCI group (16) . 15. Serruys PW, Ong ATL, van Herwerden LA, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: The final analysis of the Arterial Revascularization Therapies Study (ARTS) Randomized Trial. Journal of the American College of Cardiology 2005; 46:575-581 16. Serruys PW, Onuma Y, Garg S, et al. Five-year clinical outcomes of the ARTS II (Arterial Revascularization Therapies Study II) of the Sirolimus-eluting stent in the treatment of patients with multivessel de novo coronary artery lesions. Journal of the American College of Cardiology 2010; 55(11):1093-1101
In this study, no significant difference in the rates of MACCE among patients with low, intermediate and high scores in the medical, CABG and PCI groups. 10 out of the 17 patients in the PCI group had high SYNTAX scores. The most common reason for choice of treatment was the preference of the patient and relatives even after explaining the benefits, disadvantages and risks of CABG and PCI.
Two patients at high risk for surgery underwent PCI while another three patients had emergency PCI of the culprit vessel for ST elevation myocardial infarction.
LIMITATIONS OF THE STUDY
•Limited by the availability of the pertinent data or values in the hospital records. •Data from this study was dependent on the record keeping and monitoring of the hospital, and were presumed correct and accurate. •Availability of records on follow-up and by the short follow-up interval.
RECOMMENDATIONS
•Prospective study •Include and follow-up all patients undergoing coronary angiography at the Cardiac Catheterization Laboratory of The Medical City and their clinical outcome after definitive treatment for a longer period of time (5 years or more).
CONCLUSION
• Patients who underwent CABG were significantly younger compared to those who opt medical treatment and PCI.
• Clinical events and outcomes of patients with three-vessel difference.
and/or left medical therapy, PCI and CABG group.
main involvement shown were similar in the • MACCE in hospital and on 12 months follow-up showed no statistically significant
CONCLUSION
•Clinical events and outcomes according to SYNTAX category likewise showed no statistical significant difference in the occurrence of major cardiac and cerebrovascular events (MACCE) in hospital and at 30 days, 6 and 12 months after discharge.
T HANK YOU !