zammit_NESS2011 - North East Sleep Society
advertisement

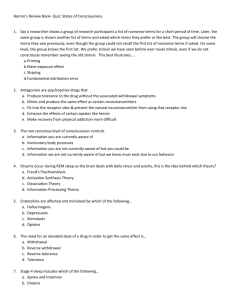
Behavioral versus Pharmacological Therapy for Adult Insomnia Gary K. Zammit, Ph.D. Clinilabs Columbia University College of Physicians and Surgeons Conflict Statement I am deeply conflicted. I have been so for many years. It is an affliction that I blame on my parents, the Catholic church, and several institutions of higher learning. Most of my conflicts were personal, until a few years ago when I had to start revealing my conflicts to the public whenever I gave a lecture. Apparently, this is a rule that only applies to me, since I’ve never seen anyone else reveal all of their potential conflicts. Having been exposed to clinical training and psychoanalytic psychotherapy for many years in my youth, my interpretation of conflict may be more expansive than others, who seem to think that conflicts only relate to one’s finances. I know better; conflicts certainly run deeper than that and often are seated in the unconscious mind. I would be happy to speak with you about all of my conflicts, preferably over a martini. However, if you primarily are interested in learning about my financial conflicts, I can say with brevity and unabashed honesty that I have none. I believe that I should be compensated for an honest day’s work, I seek to obtain such compensation whenever possible, and I encourage anyone who cares to listen to do the same. I see no conflict there, and I will be happy to debate anyone on this topic so long as they do not have other conflicts like I do because I find that those debates require lengthy discussion for which I simply am not equipped and no longer have the time. Conflicts of Interest Grants/Research Support: Abbott, Actelion, Ancile, Apnex, Arena, Aventis, Cephalon Inc., CHDI, Elan, Epix, Evotec, Forest, Galderma, Glaxo Smith Kline, H. Lundbeck A/S, King, Merck and Co., Johnson & Johnson, National Institute of Health (NIH), Neurim, Neurocrine Biosciences, Neurogen, Organon, Orphan Medical, Pfizer, Respironics, Sanofi-Aventis, Sanofi-Synthelabo, Schering-Plough, Sepracor, Shire, Somaxon, Takeda Pharmaceuticals North America, Targacept, Thymon, Transcept, UCB Pharma, Predix, Vanda, Wyeth-Ayerst Research Consultant: Actelion, Alexza, Arena, Aventis, Biovail, Boehringer-Ingelheim, Cephalon, Elan, Eli Lilly, Evotec, Forest, Glaxo Smith Kline, Jazz, King Pharmaceuticals, Ligand, McNeil, Merck, Neurocrine Biosciences, Organon, Pfizer, Renovis, Sanofi-Aventis, Select Comfort, Sepracor, Shire, Somnus, Takeda Pharmaceuticals, Vela, Wyeth Honoraria: Neurocrine Biosciences, King Pharmaceuticals, McNeil, SanofiAventis, Sanofi-Synthelabo, Sepracor, Takeda Pharmaceuticals, Vela Pharmaceuticals, Wyeth-Ayerst Research Ownership, Directorship: Clinilabs, Inc., Clinilabs IPA, Inc., Clinilabs Physician Services, PC. Industry Stocks Held: None outside of mutual funds Presentation and Learning Objectives The objectives of this presentation are to: • Define primary and co-morbid insomnia • Identify drug treatments for insomnia, and present data regarding their efficacy and safety • Identify behavioral treatments for insomnia, and present data regarding their efficacy and safety • Address the merits of behavioral and drug treatments of insomnia, comparing and contrasting the utility of both in clinical practice • Attendees will gain an understanding of behavioral and drug treatments for insomnia, and their possible use in clinical practice. The Definition of Insomnia One or More of the Following Symptoms Must be Present Difficulty Initiating Sleep Difficulty Maintaining Sleep Non-restorative1 or Poor Quality Sleep2 Associated with Clinically Significant1 or Marked2 Distress or Impairment At Least 1 Month in Duration1,2 (3x/Week2) Preoccupation with Sleeplessness and Excessive Concern over its Consequences2 1 2 APA. Diagnostic and Statistical Manual of Mental Disorders - 4th Edition, Text Revision. 2000. WHO. International Statistical Classification of Diseases and Related Health Problems, 10 th Revision, 2006 Prevalence of Insomnia The American Insomnia Survey Methods: Epidemiological survey of managed health care plan subscribers (n = 10,094), assessed for insomnia with the Brief Insomnia Questionnaire, a clinically validated scale generating diagnoses according to DSM-IV-TR; International, ICD-10, and RDC criteria Results: Insomnia prevalence estimates varied widely, from 22.1% for DSM-IV-TR to 3.9% for ICD-10 criteria • Although ICD insomnia was associated with significantly worse perceived health than DSM or RDC/ICSD insomnia, DSM-only cases also had significant decrements in perceived health. Conclusions: Insomnia is highly prevalent and associated with substantial decrements in perceived health. Roth, T., Coulouvrat, C., Hajak, G., et. al., 2011, Biological Psychiatry, 69, 592 – 602. Landmark Report on Insomnia State-of-the-Science Estimates 10% of adults with insomnia associated with impairment National Institutes of Health State-of-the-Science Conference on the Manifestations and Management of Chronic Insomnia in Adults (2005) 1 • Underscores need for appropriate diagnosis and treatment of insomnia • Emphasizes need for further education and research on insomnia as a condition2 Chronic insomnia is a major public health problem affecting millions of individuals, along with their families and communities 1. NIH State-of-the-Science Conference Statement on Manifestations and Management of Chronic Insomnia in Adults. J Clin Sleep Med. 2005; 412 - 421 2. Colten HR et al. Institute of Medicine of the National Academies. Washington, DC. National Academies Press. 2006. Sleep Maintenance Insomnia Most Common US results (n=2,061): 27.1% insomnia prevalence • from an international telephone survey (N=5,132) Of US patients with sleep disturbances:* • 42% have sleep problems [nearly] every night Difficulty falling asleep ~50% Sleep maintenance problems† ~70% Poor sleep quality ~40% • Mean number of symptoms is 1.9 • 24% report all 3 symptoms *n=570 †Interrupted sleep and early morning awakening. Leger D et al. Curr Med Res Opin. 2005;21:1785-1792. Symptoms of individuals who reported sleep disturbances during last 12 months Sleep Maintenance Insomnia: A Clinically Relevant Distinction METHODS: Cross-sectional telephone study was performed in the non-institutionalized general population of France, the United Kingdom, Germany, Italy and Spain. • Representative sample of 22,740 non-institutionalized individuals age ≥15 • DRS defined as a complaint of difficulty in resuming or inability to resume sleep occurring at least three nights per week and lasting for at least one month. RESULTS: A total of 16.1% [95% CI: 15.6-16.6] of the sample had DRS • Prevalence higher in women and increased with age, mean duration 40 months • DRS individuals slept on average 30 min less than other subjects with insomnia symptoms and 60 min less than the rest of the sample • Psychiatric conditions more common. Daytime impairment was observed in 52.2% of DRS individuals compared to 32.8% in individuals with classical insomnia symptoms (p < 0.0001). CONCLUSIONS: • DRS affect a large segment of the population • DRS is a good indicator of an ongoing sleep or mental disorder • DRS has a stronger impact on daytime functioning than classical insomnia symptoms (OR: 4.7). Ohayon, M. 2009. Journal of Psychiatry Research, 43, 934 – 940. Symptoms of Insomnia are Persistent: Chronicity Documented by Empirical Research Insomnia is a chronic condition1 Insomnia is a chronic condition in the elderly2 Epidemiological study included 870 subjects with insomnia • 69% continued to have insomnia at 12-month follow-up3 64-month longitudinal data in 28 patients well-characterized with insomnia4 • Initial 100% • 40 months 70.4% • 64 months 88.2% Seven-year follow-up study of young adults with insomnia indicates that insomnia persists in 8% - 10%, with recurrent, brief episodes of insomnia in 13% - 19%5,6 1.Katz, McHorney, Arch. Internal Medicine, 1998; 2. Ganguli, M, Reynolds, CF, Gilby, JE. J. Am. Geritric Society, 1996; 3. Morphy, Dunn, Lewis, et. al., Sleep, 2007; 4. Mendelson, WB. Sleep, 1995; 5. Angst, J, Vollrath, M, Koch, R, et. al. Eur. Arch. Psychiatr. Clin. Neurosci., 1989; 6. Vollrath, M, Wicki, W., Angst, J. Eur. Arch. Psychiatr. Clin. Neurosci, 1989 INSOMNIA DURING 2-YEAR FOLLOW-UP Katz and McHorney, Arch Intern Med, 1998 80 70 60 50 40 30 20 10 0 Follow-up status No insomnia n = 801 No insomnia Mild insomnia n = 557 Baseline status Mild insomnia Severe insomnia n = 264 Severe insomnia NIH State-of-the-Science Conference Statement Recognizes Chronic Insomnia: The NIH report indicates that… “the panel is concerned about the mismatch between the potential lifelong nature of this illness and the longest clinical trials, which have lasted 1 year or less…” An Important Paradigm Shift: Recognition of chronic insomnia may influence research and clinical practice, with implications for long-term treatment NIH. National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13-15, 2005, Sleep, 2005 Sep 1;28(9):1049-57. NIH State-of-the-Science Conference and Co-Morbid Insomnia As much as 85% of all insomnia may be comorbid with other conditions “Co-morbid insomnia” is an appropriate term • Mechanistic and causal pathways not known • The term secondary insomnia may promote undertreatment NIH. National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13-15, 2005, Sleep, 2005 Sep 1;28(9):1049-57. Insomnia: Often Comorbid Cardiovascular diseases • Ischemic heart disease • Nocturnal angina Respiratory diseases • Chronic obstructive pulmonary disease • Bronchial asthma Gastrointestinal diseases • Peptic ulcer disease • Gastroesophageal reflux Neurological diseases • Parkinson’s/Alzheimer’s Rheumatic disorders • Fibromyalgia • Osteoarthritis Psychiatric disorders Dyspnea (from any cause) Thase ME. Gen Hosp Psychiatry. 2005;27:100-112. Endocrine syndromes • Diabetes • Menopause • Hyperthyroidism Pain (from any cause) Associated sleep disorders • Sleep apnea • Restless legs syndrome • Periodic limb movement disorder Miscellaneous conditions • Dermatologic • Chronic fatigue syndrome • HIV/AIDS • Lyme disease • Systemic cancer • Pregnancy • Medical treatment induced QUALITY OF LIFE IN INSOMNIA METHODS 362 men and women,18 - 75 years of age, were prospectively studied 261 (72%) met criteria for the insomnia group 101 (28%) met criteria for the control group INSOMNIA GROUP Insomnia at least 3 times per week for at least 1 month Typical sleep latency greater than or equal to 30 minutes 3 or more awakenings per night, with difficulty returning to sleep Total sleep time less than 6.5 hours per night No history of serious medical, psychiatric, or sleep disorder Zammit GK et al. Sleep. 1999;22(suppl):S379-S385. CONTROL GROUP No history of insomnia Regular periods of nighttime sleep No history of serious medical, psychiatric, or sleep disorder Burden of Insomnia on Quality of Life Insomnia Impacts Quality of Life 95 SF-36 Scale Score P<.0001 75 N=362 55 Control Insomnia 35 Body Pain General Health Mental Health Role Emotional Role Physical Social Functioning Vitality Physical Functioning Significant differences were observed between insomnia and control subjects on all scales of the SF-36, all significant at the P<.0001 level Zammit GK et al. Sleep. 1999;22(suppl):S379-S385. Health and Insomnia Short sleep duration is associated with myriad health risks • • • • • Obesity Diabetes Hypertension Hypercholesterolemia Depression Insomnia is associated with risk of psychiatric illness • Depression • Anxiety Gangwisch, J., et. al., 2005, Sleep, 28, 1289 – 1296; Gangwisch, J. et. al., 2007, Seep, 30, 1667 – 1673; Gangwisch, J. E., et. al., 2006, Hypertension, 47, 833 – 839; Gangwisch, J. E., 2010, Sleep, 33, 956 – 961; Gangwisch, J. E., 2010, 33, 97 – 106; Breslau, N., et. al., 1996, Arch. Gen. Psychiatry.; Buysse, D., et. al., 2008, Sleep. The Debate: Treatment Considerations Insomnia is a common condition • Treatment should be widely available Sleep maintenance insomnia is the most common form of insomnia • Treatment should enable patients to stay asleep or fall asleep easily after an awakening Insomnia is a chronic condition • Should have sustained efficacy or available for long-term use Insomnia often is co-morbid • Treatment should be able to be used in context of other illness Insomnia is associated with impairment and health risk • Treatment should be safe and reduce impairment and improve health outcomes Treatments for Insomnia Pharmacologic treatments • Hypnotics Behavioral treatments • Sleep hygiene • Stimulus control therapy • Sleep restriction therapy • Cognitive-behavioral therapy • Relaxation therapy • Paradoxical intent Hypnotics are Widely Available Primary care physicians increasingly aware of sleep disorders, including insomnia Primary care physicians and “physician extenders” (e.g., physician assistants) can prescribe hypnotics Common treatment indicated for insomnia is now generic (zolpidem) • Affordability Greater than 56 million prescriptions for insomnia were issued in 2008 indicating wide availability of hypnotics1 1IMS Health, 2009, reference in USA Today 03/01/2009 Eszopiclone Efficacy and Safety Randomized, double-blind, placebo-controlled, multicenter, outpatient study in adults with chronic primary insomnia Entry criteria • Primary insomnia, self-reported average sleep duration 6.5 hrs/night and sleep onset latency > 30 min Treatments and duration • Six month double-blind Tx period: Esz 3 mg vs placebo nightly • Six-month open-label extension period: Esz 3 mg nightly Method • Subjects required to use 3 doses per week (7-day period), or 15 doses per month (30-day period), to continue in study Krystal et al. Sleep. 2003:26;793-799 Self-Reported Sleep Onset Latency (SOL) 70 ESZ Observed ESZ Completers ESZ LOCF Median minutes 60 Placebo Observed Placebo Completers Placebo LOCF 50 40 30 ** 20 ** ** ** ** ** ** 1 2 3 4 5 6 10 0 0 Month **P < 0.01; P-values represent within-group pairwise comparisons at each point for all groups. Krystal et al. Sleep. 2003:26;793-799 Median minutes Self-Reported Wake Time After Sleep Onset (sWASO) 60 ESZ Observed Placebo Observed 50 ESZ Completers ESZ LOCF Placebo Completers Placebo LOCF 40 30 20 * 10 * * * * * * 2 3 4 5 6 0 0 1 Month *P < 0.05; +P = 0.07 for Observed; P-values represent within group pairwise comparisons at each point for all groups. Krystal et al. Sleep. 2003:26;793-799 Low-Dose Doxepin Reduces WASO Objective: To evaluate the efficacy and safety of doxepin 1 mg and 3 mg in elderly subjects with chronic primary insomnia Methods: • Randomized, double-blind, parallel-group, placebo-controlled trial • Subjects meeting DSM-IV-TR criteria for primary insomnia were • • • • randomized to 12 weeks of nightly treatment with doxepin (DXP) 1 mg (n = 77) or 3 mg (n = 82), or placebo (PBO; n = 81) Efficacy was assessed using polysomnography (PSG), patient reports, and clinician ratings Objective efficacy data were reported for Nights (N) 1, 29, and 85 Self-report efficacy data during Weeks 1, 4, and 12, Clinical Global Impression (CGI) scale, and Patient Global Impression (PGI) were obtained Safety assessments were conducted throughout the study. Krystal, A., et. al., 2010, Sleep, 33 (11), 1553 - 1561 Low-Dose Doxepin Reduces WASO *P< 0.05,** p< 0.0001 130 120 110 100 * * 90 80 ** ** 70 Baseline Placebo Night 1 Doxepin 1 mg Night 85 Doxepin 3 mg Efficacy of Non-Nightly Zolpidem over 8 Weeks: Self Reported Total Sleep Time 420 * * * * Weeks 1-2 Weeks 3-4 Weeks 5-6 Weeks 7-8 minutes 400 380 360 340 320 300 Placebo pill n=71 Zolpidem 10 mg pill n=63 Walsh et al., Sleep, 2000 Placebo no pill n=71 Zolpidem no pill n=63 * p < .001 for zolpidem-pill vs. placebo-pill Use of Hypnotics in Co-Morbid Insomnia Depression • Improvements in SL, WASO, and TST after treatment with eszopiclone and fluoxetine1 Generalized anxiety disorder • Total sleep time improved after treatment with zolpidem and escitalopram2 Chronic pain • Eszopiclone significantly improved all patient-reported sleep measures (WASO, SL, and TST), sleep quality, depth of sleep, and daytime function (P < .05 vs placebo); 48% of eszopiclonetreated patients had no clinically meaningful insomnia as assessed by ISI score (versus 30% of placebo-treated patients (P = .03)3 A., et. al., 2007, J. Clinical Sleep Medicine,3, 48 – 55; 2Fava, M., et. al., 2009, J. Clinical Psychopharmacol., 29, 222 – 230; 3Roth, T., et. al., 2007, Primary Care Companion J. Clinical Psychiatry, 11, 292 - 301 1Krystal, Most Common AEs in 5-Week Placebo-Controlled Study of Ramelteon in Adults with Insomnia Placebo n = 131 Ramelteon 8 mg N = 139 Ramelteon 16 mg n = 135 Any 48.1% 51.1% 54.8% Headache NOS 18.3% 19.4% 17.8% Somnolence 1.5% 7.9% 7.4% Fatigue 2.3% 9.4% 4.4% Nausea 2.3% 4.3% 4.4% Nasopharyngitis 3.1% 2.9% 3.7% Diarrhea NOS 1.5% 1.4% 3.7% URI NOS 3.1% 4.3% 0.7% Dizziness 3.8% 3.6% 1.5% Nasal Congestion 0.8% 1.4% 3.0% AE * All reported AEs ≥ 3% Zammit et al. 2007. Journal of Clinical Sleep Medicine, 3, 495 - 504 Low Frequency of Reported Adverse Reactions to Sedative Hypnotics in Hospital Setting •Data derived from 3,000 cases per year of adverse drug reactions •Presented to Drug Outcomes Management Committee for review •AEs entered into database over 3 year period Drug Class Total Doses Dispensed Reported Adverse Events Frequency (%) Chloral Hydrate 2,768 0 0 Pentobarbital 546 0 0 Temazepam 79,016 3 0.004 Triazolam 9,656 2 0.02 Mendelson, W., et. al. (1996). Sleep, 19, 702 – 706; Low Rate of AEs Reported in Outpatient Clinical Practice Uncontrolled surveillance study • Office-based physicians • Examined 16,944 patients with insomnia who were given zolpidem during a four-week period Total of 268 AEs (1/113, 2/53, >2/16) • Overall rate of 0.006% There were 118 discontinuations due to AEs • Nausea (36) • Dizziness (35) • Malaise (23) • Nightmares (20) • Agitation (19) • Headache (18) Hajak, G. & Bandelow, B. (1998). Int. Clin. Psychopharmacol., 13, 157 - 167 Residual Effects of Hypnotics Residual effects refer to continued sedation or impairment in memory and psychomotor functioning following morning awakening Assessed using self-report measures and objective test data • Digit symbol substitution test • Symbol copying test • Immediate and delayed recall tests • Driving performance Residual effects of BZRAs may be related to dose, half-life, and time of dose Recently-approved therapeutics not associated with significant residual effects Blin, et. al., 2006. J. Clin. Psychopharmacol., 26, 284 – 289; Vermeeren, A., 2004, CNS Drugs, 18, 297 - 328 Potential Residual Memory Effects of Benzodiazepine Hypnotics 16 14 12 10 Placebo Flurazepam Lorazepam Triazolam 8 6 4 2 0 Mean Items Immediate Recall Mean Digits Immediate Recall Mean Items Morning Recall Roth, et. al., (1980). Psychopharmacology, 70, 231 - 237 Mean Digits Morning Recall Next-Day Psychomotor Functioning 70 Morning DSST Scores^ Score (median) Improvement 60 50 40 30 20 10 0 Baseline Placebo ^Mean of 3 time points (days 1, 15, & 29) Baseline ESZ 3 mg Mean +/- 1 SD for age group 35-44 norm – Wechsler adult intelligent scale Zammit et al. Curr. Med. Res. Op., 2004, 20, 1979 - 1991 Driving Studies Standardized highway driving tests 100 km (61 miles) over highway circuit at constant speed Primary outcome: standard deviation from lateral position (SDLP) 11 studies using this methodology have provided data • Zaleplon 10 mg, 20 mg: No significant effects > 2hours postadministration • Temazepam 10 mg, 20 mg, 30 mg: Low incidence of driving impairment • Zolpidem 10 mg: Moderate to severe impairing effects 5 – 7 hours post-administration • Flurazepam 30 mg: Severe impairment, greater than equivalent BAC of 1.0 g/L • Triazolam 0.5 mg: Marked residual effects, dose-dependent; with effects in first hour after rising following 0.25 mg and 0.125 mg Vermeeren, A., 2004, CNS Drugs, 18, 297 - 328 Benzodiazepine Use and Risk of Falls1 and Fractures2 in Older Women Relative Risk 2 n=8,127 Short-acting Long-acting 1 0 Frequent falls 1Ensrud Non-spine fracture Outcome Hip fracture KE et al. J Am Geriatr Soc 2002;50:1629–37; 2Ensrud KE et al. Arch Intern Med 2003;163:949–57. Postural Instability and Hypnotic Use SOT Score Change from Baseline Sensory Organization Test Composite Score 0 -5 P =0.837 -10 -15 -20 -25 -30 P <0.001 -35 Placebo Zammit, G. K. 2008. BMC Geriatrics. Ramelteon Zolpidem Abuse and Dependence Liability Hypnotic abuse and dependence are a concern of practitioners and patients Evidence of hypnotic abuse or dependence among people with insomnia is minimal Most indicators of abuse or dependence not evident in people with insomnia who use hypnotics • Withdrawal • Non-therapeutic use • Tolerance • Dose escalation Discontinuation Effects of Hypnotics Rebound insomnia is most frequently reported discontinuation effect • Typically 1 – 2 nights • May occur following even short-term use1 • Does not increase in severity with longer durations of use • More likely to occur with high doses Rebound insomnia must be differentiated from recrudescence or withdrawal2 1. Roehrs, T., et. al., 1992, Psychopharmacology, 107, 480 – 484; 2. Walsh, J., et. al., Principles and Practice of Sleep Medicine, 4th Edition Limited Evidence of Withdrawal Effects with Commonly-Prescribed Hypnotics Period 1 Period 2 Period 3 Period 4 TST Baseline 319.5 320.3 321.2 323.5 1st Night Off 307.0 315.4 334.6 337.5 76.1 75.7 75.9 72.3 *90.1 89.4 76.2 75.5 Baseline 2.35 2.34 2.38 2.41 1st Night Off 2.62 2.25 2.24 2.09 SL Baseline 1st Night Off NAW Walsh, J., et. al., 2000, Sleep, 23, 1087 - 1096 *P < 0.04 Relative Abuse Liability of 19 Hypnotics Pentobarbital Methaqualone Diazepam Flunitrazepam Lorazepam GHB Temazepam Zaleplon Eszopiclone Triazolam Zopiclone Flurazepam Zolpidem Estazolam Oxazepam Diphenhydramine Quazepam Trazodone Ramelteon Likelihood of Abuse Toxicity 0 20 40 60 Score Griffiths R, Johnson M. 2005, J Clin Psychiatry, 66 (suppl 9): 31 - 41 80 100 Sedative-Hypnotic Drug Products Class Safety Labeling December 2006, FDA requested that the whole class of hypnotic drugs revise product labeling to include warnings about the following potential adverse events: Anaphylaxis (severe allergic reaction) Angioedema (severe facial swelling) Complex sleep-related behaviors Letters to health care providers. Patient Medication Guides to inform consumers Treatment Considerations Variable Pharmacotherapy Widely Available Yes WASO or sWASO Yes Sustained Efficacy or Available for Long Term Use Yes Use in Co-Morbid Insomnia Yes Reduce Impairment or Health Risk No Safe Concerns Behavioral Therapy Behavioral Treatment for Insomnia is Not Widely Available Availability of behavioral treatment is severely limited • Lack of trained clinicians • Poor geographic distribution of knowledgeable providers • Inaccessibility to treatments and clinicians Behavioral treatment paid at lower rates than physician visits for medical care Multiple visits required for treatment that meets current standard of care Ritterband, L. M., et. al., 2009, Archives of General Psychiatry, 66, 692 - 698 Meta-Analysis of the Efficacy of Behavioral Treatments for Insomnia Objective: Meta-analysis of behavioral treatments for insomnia Methods: A systematic review was conducted on 37 treatment studies (N = 2246 subjects/patients) published between 1998 and 2004 inclusively Criteria for inclusion of a study were as follows • Main sleep diagnosis was insomnia (primary or comorbid) • At least 1 treatment condition was psychological or behavioral in content • The study design was a randomized controlled trial, a nonrandomized group design, a clinical case series or a single subject experimental design with a minimum of 10 subjects • The study included at least 1 of the following as dependent variables: sleep onset latency, number and/or duration of awakenings, total sleep time, sleep efficiency, or sleep quality Morin, C., et. al., Sleep, 2006, 29, 1398 1414 Meta-Analysis of the Efficacy of Behavioral Treatments for Insomnia Seventeen studies examined CBT in primary insomnia, five of which were randomized, controlled clinical trials Overall, studies showed that CBT had greater improvement on sleep diary and PSG variables than control conditions Twenty-six studies provided follow-up data, indicating the durability of behavioral treatment over short, intermediate, and long (>12 months) periods Benefits observed when specialists or non-specialists (e.g., primary care physicians, nurse practitioners) administered treatment Morin, C., et. al., Sleep, 2006, 29, 1398 1414 Behavioral Therapy Reduces WASO Objective To test the efficacy of a hybrid cognitive behavioral therapy (CBT) compared with both a first-generation behavioral treatment and a placebo therapy for treating primary sleep-maintenance insomnia. Design: Randomized, double-blind, placebo-controlled clinical trial Patients Seventy-five adults (n=35 women; mean age, 55.3 years) with chronic primary sleep-maintenance insomnia (mean duration of symptoms, 13.6 years) Interventions Patients were randomly assigned to receive outpatient CBT (sleep education, stimulus control, and time-in-bed restrictions; n=25), progressive muscle relaxation training (RT; n=25), or a quasidesensitization (placebo) treatment (n=25) for six weeks, with follow-up conducted at 6 months. Main Outcome Measures: Polysomnography and sleep log measures of total sleep time, middle and terminal wake time after sleep onset (WASO), and sleep efficiency Edinger, J., et. al., 2006, JAMA, 285, 1856 - 1864 Behavioral Therapy Reduces WASO Measure Baseline Mean CBT RT Placebo P Value TST Log 336.8m 360.0m 362.0m 361.0m 0.99 TST PSG 352.1m 372.4m 337.9m 334.0m 0.02 CBT>P WASO Log 56.2m 28.1m 44.4m 47.1m 0.004 CBT<RT&P WASO PSG 50.8m 30.1m 50.6m 66.4m 0.02 CBT<P WAST Log 47.7m 21.1m 36.2m 47.0m 0.02 CBT<P WAST PSG 14.1m 4.2m 10.2m 12.4m 0.02 CBT<P SE Log 72.0% 84.3% 78.1% 76.2% 0.002 CBT>RT&P SE PSG 77.8% 85.5% 78.1% 75.7% 0.002 CBT>RT&P Edinger, J., et. al., 2006, JAMA, 285, 1856 - 1864 Post-Hoc Test Behavioral Therapy & Co-Morbid Insomnia Chronic pain: • SOL, WASO, SE improved following CBT versus control1 o o SOL reduced from 55 minutes to 28 minutes SE increased from 72% to 85% Medical Illness • In a study of 51 older adults, WASO and SE improved following CBT or RT versus control2 • In a study of 49 older adults with insomnia associated with medical and psychiatric conditions,3 a combined intervention of stimulus control, relaxation, and education reduced WASO 25 min and increased SE 11% at post treatment o Fifty-seven percent (57%) of treated patients achieved clinically significant improvements on SE relative to 19% of control patients S.R., et. al., 2000, Journal of Consulting and Clinical Psychology, 68, 407 – 416; 2Rybarczyk, B., et. al., 2002, Psychological Aging, 17, 288 – 298; 3Lichstein, K.L., et. al., 2000, Psychol Aging, 15, 232 - 240 1Currie, Brief Behavioral Treatment for Insomnia Objective: To assess the efficacy of individualized behavioral treatment for insomnia, delivered in two sessions and two telephone calls Primary outcome: Categorical status at four weeks following the initiation of treatment Sample: Seventy-nine elderly adults, 54 female, recruited from the community and one primary care clinic Method: Participants were randomly assigned to receive BBTI or IC (information control) over a four-week period. • All treatments were administered by a nurse clinician Buysse, D., et. al., Archives of Internal Medicine, 2011, e-pub January 24, 2011 Brief Behavioral Treatment for Insomnia Outcome After Four Weeks of Treatment 70 60 (P<.001) 60 50 50 40 40 30 30 20 20 10 10 0 Remission Response BBTI (n = 39) Partial Remission IC (n = 40) NonResponse 0 No Longer Meet DSM-IV Criteria BBTI (n = 39) Buysse, D., et. al., Archives of Internal Medicine, 2011, e-pub January 24, 2011 IC (n = 39) Internet Expansion of Access to Care OBJECTIVE: Evaluate structured behavioral Internet intervention for adults with insomnia. DESIGN, SETTING, AND PARTICIPANTS • Forty-five adults randomly assigned to an Internet intervention (n = 22) or waitlist control group (n = 23). INTERVENTION: The Internet intervention based on well-established face-to-face cognitive behavioral therapy incorporating the primary components of sleep restriction, stimulus control, sleep hygiene, cognitive restructuring, and relapse prevention MAIN OUTCOME MEASURES: The Insomnia Severity Index and daily sleep diary data were used to determine changes in insomnia severity and the main sleep variables, including wake after sleep onset and sleep efficiency RESULTS • Insomnia Severity Index significantly improved from 15.73 for the Internet group but did not change for the control group (P < .001) • The Internet group maintained gains at the 6-month follow-up • Internet participants achieved significant decreases in wake after sleep onset (55%) and increases in sleep efficiency (16%) compared with the nonsignificant control group changes of wake after sleep onset 8% and sleep efficiency 3% Ritterband, L.M., et. al. 2009. Arch. Gen. Psychiatry, 66, 692 Comparison of CBT, Zopiclone, and Placebo Objective: To examine short- and long-term clinical efficacy of CBT, zopiclone 7.5 mg, and placebo in older adults experiencing chronic primary insomnia. Design: Randomized double-blinded, placebo controlled trial of 46 adults (mean age, 60.8 y; 22 women) with chronic primary insomnia Intervention: CBT (sleep hygiene, sleep restriction, stimulus control, cognitive therapy, and relaxation; n=18), sleep medication (7.5-mg zopiclone each night; n=16), or placebo (n=12) • All treatment duration was 6 weeks • Follow-up at 6 months. Main Outcome Measures: Ambulatory PSG and sleep diaries Results: • CBT resulted in improved short- and long-term outcomes compared with zopiclone on 3 out of 4 outcome measures. • At 6 weeks, CBT improved sleep efficiency from 81.4% at pretreatment to 90.1% at 6-month follow-up compared with a decrease from 82.3% to 81.9% in the zopiclone group • At 6 months patients receiving CBT had better sleep efficiency using polysomnography than those taking zopiclone Silversten, B. et. al. 2006. JAMA, 295, 2851 Combined use of B and P Objectives To evaluate the added value of medication over CBT alone for acute treatment of insomnia and the effects of maintenance therapies Design: Randomized controlled trial involving 2-stage therapy for 160 adults with persistent insomnia Interventions CBTalone or CBT plus 10mg/d zolpidem for an initial 6-week therapy, followed by extended 6-month therapy. • CBT received monthly maintenance CBT for 6 months or received no additional treatment • Combined continued with CBT plus intermittent use of zolpidem or CBT only Main Outcome Measures SoL, TST, SE derived from diaries; treatment response and remission rates derived from the Insomnia Severity Index Results CBT used singly or in combination with zolpidem produced significant improvements in SoL, SE during initial therapy (all P.001) Larger increase of sleep time was obtained with the combined approach (P=.04) Combined therapy produced a higher remission rate compared with CBT alone during the 6-month extended therapy phase and the 6-month follow-up period (56% vs 43%, P=.05) Best long-term outcome seen in combined therapy initially, followed by CBT alone, as evidenced by higher remission rates at the 6-month follow-up compared with patients who continued to take zolpidem during extended therapy (68% vs 42%, p<.04) Zolpidem 10 Mg PRN Alone and with Stimulus Control Therapy Overview Prospective, observational study in 550 primary care settings in Germany Sample 2,690 patients with chronic insomnia (mean age 59 years) Female 66% Average duration of insomnia = 5.2 years Prior use of patients who received prior pharmacotherapy = 49.7% Method Zolpidem 10 mg HS alone prescribed for “as needed” use, up to a maximum of 5 tablets per week for three weeks After three weeks of treatment, use of standard stimulus control therapy was optional on non-drug nights. Hajak, Bandelow, Zulley, et. al., Annals of Clinical Psychiatry, 14, 2002 Average Zolpidem Use During Treatment Periods 4 3.7 3.7 Tabs Number of Tablets 3.5 3 2.62.6 Tabs 2.5 2 1.5 1 0.5 0 Zolpidem 10 mg PRN After 3 Weeks (Opt. SC) P < 0.00001 Hajak, Bandelow, Zulley, et. al., Annals of Clinical Psychiatry, 14, 2002 Treatment Considerations Pharmacotherapy Behavioral Therapy Widely Available Yes Not Yet WASO or sWASO Yes Yes Sustained Efficacy or Available for Long Term Use Yes Yes Use in Co-Morbid Insomnia Yes Yes Reduce Impairment or Health Risk No No + - Variable Safety Concerns Relative Merits and Considerations Drug treatments are widely available, efficacious, and impact key sleep outcomes (WASO), but safety concerns persist Behavioral treatments are not as widely available but are efficacious, impact key sleep outcomes, and are associated with fewer concerns than drug treatments Neither drug or behavioral treatments have been shown to improve daytime functioning or health outcomes Practice guidelines emphasize the value of clinician judgment in treatment planning “B vs. P” State of the Science Studies are needed to evaluate the effectiveness insomnia treatments in improving measures of clinical significance, such as daytime function, quality of life, health outcomes Further research is needed to comparing the effectiveness of single versus combined drug, device, psychological, or behavioral therapies for insomnia. Further research is to identify patient groups where combination or single therapy is most appropriate. Studies are needed that compare treatments for insomnia with regard to their short and long-term effectiveness, risks/benefits, costs, and patient satisfaction.