biochem ch 22 [12-11
advertisement

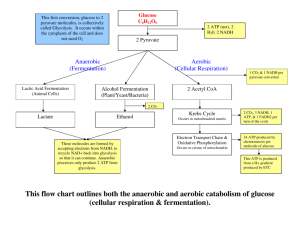
Bio Chem Ch 22 Generation of ATP from Glucose: Glycolysis Glucose – universal fuel for human cells; every cell type able to generate ATP from glycolysis (pathway by which glucose oxidized and cleaved to form pyruvate) Glycolysis begins with phosphorylation of glucose to glucose-6-phophate (glucose 6-P) by hexokinase o In subsequent steps, one glucose 6-P molecule is oxidized to 2 pyruvate molecules with generation of 2 NADH/ net generation of 2 ATP occurs through direct transfer of high-energy phosphate from intermediates of pathway of ADP (substrate-level phosphorylation) When cells have limited supply of O2 (e.g., kidney medulla), or few or no mitochondria (e.g., RBC), or greatly increased demands for ATP (e.g., skeletal muscle during high-intensity exercise), they rely on anaerobic glycolysis for generation of ATP o In anaerobic glycolysis, lactate dehydrogenase oxidizes NADH generated from glycolysis by reducing pyruvate to lactate o Because O2 not required to reoxidize NADH, pathway is anaerobic o Energy yield form anaerobic glycolysis (2 ATP per glucose) much lower than yield from aerobic oxidation o Lactate (lactic acid) released into blood o Under pathologic conditions that cause hypoxia, tissues may generate enough lactic acid to cause lactic acidemia In each cell, glycolysis regulated to ensure ATP homeostasis maintained without using more glucose than necessary o In most cell types, hexokinase (first enzyme of glycolysis) inhibited by glucose 6-P; thus glucose not taken up and phosphorylated by cell unless glucose 6-P enters a metabolic pathway, such as glycolysis or glycogen synthesis o Control of glucose 6-P entry into glycolysis occurs at phosphofructokinase-1 (PFK-1), the rate-limiting enzyme of pathway PFK-1 allosterically inhibited by ATP and allosterically activated by AMP Glycolysis has functions in addition to ATP production; for example, in liver and adipose tissue, glycolysis generates pyruvate as precursor for fatty acid biosynthesis o Glycolysis provides precursors for synthesis of compounds such as AAs and 5-carbon sugar phosphates Hematocrit and Hgb content measured to determine whether oxygen-carrying capacity of blood adequate o Both values can be decreased by conditions that interfere with erythropoiesis, such as iron deficiency o Both can also be decreased during chronic bleeding but not during immediate acute hemorrhage, if interstitial fluid replaces lost blood volume and dilutes out RBCs Glycolysis Pyruvate may be oxidized to CO2 in TCA cycle, and ATP generated from electron transfer to O2 in oxidative phosphorylation If pyruvate and NADH from glycolysis converted to lactate (anaerobic glycolysis), ATP can be generated in absence of O2, via substrate-level phosphorylation Carbs provide 50% or more of calories in most diets, and glucose is major carbohydrate; other dietary sugars oxidized by conversion to intermediates of glycolysis After high-carb meal, glucose is major fuel for almost all tissues (exceptions include intestinal mucosal cells, which transport glucose from gut into blood, and cells in PCT of kidney, which return glucose from renal filtrate to blood) During fasting, brain continues to oxidize glucose because it has limited capacity for oxidation of fatty acids or other fuels Cells continue to use glucose for portion of ATP generation that must be met by anaerobic glycolysis, due to either limited O2 supply or limited capacity for oxidative phosphorylation (e.g., RBC) Glycolysis is anabolic pathway that provides biosynthetic precursors, including those for synthesis of AAs and ribose 5-phosphate (precursor of nucleotides) Glycolytic pathway cleaves 1 mol glucose to 2 mol pyruvate (3-carbon compound) o Consists of preparative phase and ATP-generating phase o In initial preparative phase of glycolysis, glucose phosphorylated twice by ATP and cleaved into 2 triose phosphates o ATP expenditure in beginning of preparative phase called priming the pump because initial utilization of 2 mol ATP per mol glucose results in production of 4 mol ATP per mol glucose in ATP-generating phase o In ATP-generating phase, glyceraldehyde-3-phosphate (glyceraldehyde 3-P, a triose phosphate) oxidized by NAD+ and phosphorylated using inorganic phosphate High-energy phosphate bond generated here transferred to ADP to form ATP Remaining phosphate rearranged to form another high-energy phosphate bond transferred to ADP; because 2 mol of triose phosphate formed, yield from ATP-generating phase is 4 mol ATP and 2 mol NADH; result is net yield of 2 mol ATP, 2 mol NADH, and 2 mol pyruvate Reactions of Glycolysis Glucose metabolism begins with transfer of phosphate from ATP to glucose to form glucose 6-P; phosphorylation of glucose commits it to metabolism within cell because glucose 6-P can’t be transported back across PM; phosphorylation reaction is irreversible under physiologic conditions because reaction has high-negative ΔG0’; phosphorylation doesn’t necessarily commit glucose to glycolysis though o Glucose 6-P is branch point in carb metabolism; is precursor for almost every pathway that uses glucose, including glycolysis, pentose phosphate pathway, and glycogen synthesis Can also be generated from other pathways of carb metabolism, such as glycogenolysis (breakdown of glycogen), pentose phosphate pathway, and gluconeogenesis (synthesis of glucose from noncarbohydrate sources) o Hexokinases (enzymes that acatlyze phosphorylation of glucose) are family of tissue-specific isoenzymes that differ in their kinetic properties Isoenzyme found in liver and β-cells of pancreas has much higher Km than other hexokinases and is called glucokinase In many cells, some of hexokinase is bound to porins in outer mitochondrial membrane (voltage-dependent anion channels), which gives enzymes first access to newly synthesized ATP as it exits mitochondria In remainder of preparative phase, glucose 6-P isomerized to fructose 6-phosphate (fructose 6-P), again phosphorylated, and subsequently cleaved into two 3-carbon fragments o Isomerization (positions keto group next to carbon 3) essential for subsequent cleavage of bond between carbons 3 and 4 Next step of glycolysis, phosphorylation of fructose 6-P to fructose 1,6-bisphosphate (fructose 1,6-bisP) by PFK-1, generally considered first committed step of pathway o Phosphorylation requires ATP and is thermodynamically and kinetically irreversible o PFK-1 irrevocably commits glucose to glycolytic pathway o PFK-1 is regulated enzyme in cells, and its regulation controls entry of glucose into glycolysis o PFK-1 exists as tissue-specific isoenzyme whose regulatory properties match variations in role of glycolysis in different tissues Fructose 1,6-bisP cleaved into 2 phosphorylated 3-carbon compounds (triose phosphates) by aldolase o Dihydroxyacetone phosphate (DHAP) isomerized to glyceraldehyde 3-P (triose phosphate) o Aldolase named for mechanism of forward reaction (aldol cleavage) and mechanism of reverse reaction (aldol condensation); exists as tissue-specific isoenzymes, which all catalyze cleavage of F1,6P2 but differ in specificities for fructose 1-P Uses lysine residue at active site to form covalent bond with substrate during course of reaction; inability to form covalent linkage inactivates enzyme o At this point in glycolysis pathway, 2 mol of glyceraldehyde 3-P produced and continue through path Glyceraldehyde 3-P oxidized and phosphorylated so that subsequent intermediates of glycolysis can donate phosphate to ADP to generate ATP o First reaction catalyzed by glyceraldehyde 3-P dehydrogenase (key to the pathway) Enzyme oxidizes aldehyde group of glyceraldehyde 3-P to enzyme-bound carboxyl group and transfers electrons to NAD+ to form NADH Oxidation step dependent on cysteine residue at active site of enzyme, which forms highenergy thioester bond during course of reaction High-energy intermediate immediately accepts inorganic phosphate to form high-energy acyl phosphate bond in 1,3-bisphosphoglycerate, releasing product from cysteine residue on enzyme; high-energy phosphate bond is start of substrate-level phosphorylation (formation of high-energy phosphate bond where none previously existed, without use of O2) Phosphate transferred to ADP to form ATP by phosphoglycerate kinase; energy of acyl phosphate bond high enough so transfer to ADP is energetically favorable process; another product of this reaction is 3phosphoglycerate o To transfer remaining low-energy phosphoester on 3-phosphoglycerate to ADP, it must be converted to high-energy bond – conversion accomplished by moving phosphate to second carbon (forming 2-phosphoglycerate) and then removing water to form phosphoenolpyruvate (PEP) o Enolphosphate bond is high-energy bond, so transfer of phosphate to ADP by pyruvate kinase energetically favorable Final reaction converts PEP to pyruvate Overall net reaction in glycolytic pathway is Glucose + 2 NAD+ + 2Pi + 2 ADP 2 pyruvate + 2 NADH + 4 H+ + 2 ATP + 2 H2O Confusion can be caused by inadequate delivery of O2 to brain o Neurons have very high ATP requirements, and most of ATP provided by aerobic oxidation of glucose to pyruvate in glycolysis and by pyruvate oxidation to CO2 in TCA cycle o Brain has little or no capacity to oxidize fatty acids so glucose consumption is high o Oxygen demands also high; if cerebral oxygen supply were completely interrupted, brain would last only 10 seconds Only reason consciousness lasts longer during anoxia or asphyxia is that there is still some oxygen in lungs and circulating blood Decrease of blood flow to approximately ½ normal rate results in loss of consciousness Oxidative Fates of Pyruvate and Nicotinamide Adenine Dinucleotide NADH produced from glycolysis must be continuously reoxidized back to NAD+ to provide an electron acceptor for the glyceraldehyde 3-P dehydrogenase reaction and prevent product inhibition; if it doesn’t, glycolysis stops o Aerobic route of NADH oxidation – shuttles transfer reducing equivalents across mitochondrial membrane and ultimately to electron-transport chain and O2 Shuttles required because inner mitochondrial membrane impermeable to NADH, and no transport protein exists that can translocate NADH across membrane directly; NADH converted to NAD+ in cytosol by reaction that transfers electrons to DHAP in glycerol-3-phosphate (glycerol 3-P) shuttle and oxaloacetate in malate-aspartate shuttle NAD+ formed in cytosol returns to glycolysis, and glycerol 3-P or malate carries reducing equivalents that are ultimately transferred across inner mitochondrial membrane o Anaerobic route – NADH reoxidized in cytosol by lactate dehydrogenase (LDH), which reduces pyruvate to lactate Fate of pyruvate depends on which route used for NADH oxidation: if NADH oxidized in shuttle system, pyruvate can be used for other pathways (such as oxidation to acetyl-CoA and entry into TCA cycle); if anaerobic, pyruvate reduced to lactate and diverted away from other potential pathways o Use of shuttle systems allow for more ATP to be generated than anaerobic glycolysis because it allows both oxidizing cytoplasmically derived NADH in electron-transport chain and allowing pyruvate to be oxidized completely to CO2 Glycerol 3-P shuttle is major shuttle in most tissues; cytosolic NAD+ regenerated by cytoplasmic glycerol 3-P dehydrogenase, which transfers electrons from NADH to DHAP to form glycerol 3-P, which then diffuses through outer mitochondrial membrane to inner mitochondrial membrane, where electrons donated to membranebound FAD-containing glycerophosphate dehydrogenase o Glycerophosphate dehydrogenase ultimate donates electrons to coenzyme Q (CoQ), resulting in energy yield of about 1.5 ATP from oxidative phosphorylation o DHAP returns to cytosol to continue the shuttle o Net reaction is: NADHcytosol + NAD+matrix NAD+cytosol + NADHmatrix Malate-aspartate shuttle – cytosolic NAD+ regenerated by cytosolic malate dehydrogenase, which transfers electrons from NADH to cytosolic oxaloacetate to form malate, which is transported across inner mitochondrial membrane by specific translocase, which exchanges malate for α-ketoglutarate o In matrix, malate oxidized back to oxaloacetate by mitochondrial malate dehydrogenase, and NADH generated – this NADH can donate electrons to electron-transport chain with generation of about 2.5 mol ATP per mol NADH o Newly formed oxaloacetate cannot pass back through inner mitochondrial membrane under physiologic conditions, so transamination reactions transfer amino group to oxaloacetate to form aspartate, which is transported out to cytosol (using aspartate-glutamate exchange translocase) and converted back to oxaloacetate through transamination reaction o Net reaction for this shuttle system is: NADHcytosol + NAD+matrix NAD+cytosol + NADHmatrix Anaerobic Glycolysis When oxidative capacity of cell limited (no mitochondria or no oxygen), NADH oxidized to NAD+ in cytosol by reduction of pyruvate to lactate (catalyzed by LD) with net reaction Glucose + 2 ADP + 2Pi 2 lactate + 2 ATP + 2 H2O + 2H+ In both aerobic and anaerobic glycolysis, each glucose generates 2 ATP, 2 NADH, and 2 pyruvate o Energy yield from anaerobic glycolysis is 2 ATP per glucose (pyruvate reduced to lactate) Neither NADH nor pyruvate produced used for further energy generation o When oxygen available and NADH can be oxidized via shuttle system, pyruvate can enter mitochondria and be completely oxidized to CO2 via PDH and TCA cycle Generates 12.5 ATP per pyruvate If cytosolic NADH oxidized by glycerol 3-P shuttle, about 1.5 ATP used, and if by malateaspartate shuttle, 2.5 ATP produced 2 NADH molecules produced during glycolysis can lead to 3-5 ATP being produced With both NADH and pyruvate in mind, 30-32 ATP total produced per glucose oxidized to CO2 o To produce same amount of ATP per unit time from anaerobic glycolysis, it must occur 15x faster and use 15x more glucose; cells achieve high rate of glycolysis by expressing high levels of glycolytic enzymes In certain skeletal muscles and most cells during hypoxic crisis, high rates of glycolysis associated with rapid degradation of internal glycogen stores to supply required glucose 6-P Anaerobic glycolysis results in acid production in form of H+ – glycolysis forms pyruvic acid, which is reduced to lactic acid; at intracellular pH of 7.35, lactic acid dissociates to form carboxylate anion (lactate) and H+ (pKa for lactic acid is 3.85) o Lactate and H+ both transported out of cell into interstitial fluid by transporter on PM and eventually diffuse into blood o If amount of lactate generated exceeds buffering capacity of blood, pH drops below normal range, resulting in lactic acidosis Dental caries caused principally by low pH generated from lactic acid production by oral bacteria; below pH 5.5, decalcification of tooth enamel and dentine occurs o Lactobacilli and S. mutans are major contributors because almost all their energy derived from conversion of glucose or fructose to lactic acid, and they are able to grow well at low pH generated by the process o Acid buffered by bicarbonate and other buffers in saliva, but saliva production decreases in evening, so acid can dissolve hydroxyapatite in tooth enamel during night Many tissues (RBCs, WBCs, kidney medulla, tissues of eye, and skeletal muscles) rely on anaerobic glycolysis for at least portion of ATP requirements o Tissues heavily dependent on anaerobic glycolysis usually have low ATP demand, high levels of glycolytic enzymes, and few capillaries, such that O2 must diffuse over greater distance to reach target cells o Mature RBCs have no mitochondria because oxidative metabolism might interfere with function in transporting oxygen bound to Hgb o Some of lactic acid generated by anaerobic glycolysis in skin secreted as sweat, where it acts as antibacterial agent o Many large tumors use anaerobic glycolysis for ATP production and lack capillaries in core o In tissues with some mitochondria, both aerobic and anaerobic glycolysis occur simultaneously Relative proportion depends on mitochondrial oxidative capacity of tissue and O2 supply and may vary among cell types in same tissue because of cell distance from capillaries When cell’s energy demand exceeds capacity of rate of electron-transport chain and oxidative phosphorylation to produce ATP, glycolysis activated, and increased NADH/NAD+ ratio directs excess pyruvate into lactate (PDH, TCA cycle, and electron-transport chain operating as fast as they can, but tissue needs more) In complete oxidation of pyruvate to CO2, 4 steps generate NADH (pyruvate dehydrogenase, isocitrate dehydrogenase, α-ketoglutarate dehydrogenase, and malate dehydrogenase), 1 step generates FADH2 (succinate dehydrogenase), and 1 step substrate-level phosphorylation (succinate thiokinase) o Because each NADH generates 2.5 ATP, overall contribution by NADH is 10 ATP o FADH2 generates 1.5 ATP, and by definition one substrate-level phosphorylation = 1 ATP o Add it up and 10+1.5+1 = 12.5 ATP for each turn of TCA cycle In response to hypoxemia caused by COPD, patients have increased hypoxia-inducible factor-1 (HIF-1) in tissues o HIF-1 – gene transcription factor found in tissues throughout body that plays homeostatic role in coordinating tissue responses to hypoxia o Each tissue responds with subset of these changes HIF-1 increases transcription of genes for many glycolytic enzymes (PFK-1, enolase, phosphoglycerate kinase, and LD) HIF-1 increases synthesis of several proteins that enhance O2 delivery to tissues (erythropoietin, vascular endothelial growth factor (regulates angiogenesis), and inducible NO synthase (synthesizes NO) o Patients can maintain Hct and Hgb levels that are on the high side of normal, and tissues increase capacity for anaerobic glycolysis Lactate released form cells that undergo anaerobic glycolysis taken up by other tissues (liver, heart, and skeletal muscle) and oxidized back to pyruvate o In liver, pyruvate used to synthesize glucose (gluconeogenesis), which is returned to blood o Cori cycle – cycling of lactate and glucose between peripheral tissues and liver In many other tissues, lactate oxidized to pyruvate, which is then oxidized to CO2 in TCA cycle o Equilibrium of LD reaction favors lactate production, but flux occurs in opposite direction if NADH being rapidly oxidized in eletron-transport chain (or is being used for gluconeogenesis Lactate + NAD+ pyruvate + NADH + H+ Heart, with huge mitochondrial content and oxidative capacity, able to use lactate released from other tissues as fuel During exercise, lactate released into blood from working skeletal muscles might be used by resting skeletal muscles In brain, glial cells and astrocytes produce lactate, which is used by neurons or released into blood LDH is tetramer composed of A-subunits (also called M-subunits for skeletal muscle form) and B-subunits (also called H-subunits for heart) o Different tissues produce different amounts of the 2 subunits, which combine randomly to form 5 different tetramers (M4, M3H1, M2H2, M1H3, and H4) o Isozymes differ only slightly in properties, but kinetic properties of M4 form facilitate conversion of pyruvate to lactate in skeletal muscle, whereas kinetic properties of H4 form facilitate conversion of lactate to pyruvate in heart for energy generation Tissues of eye partially dependent on anaerobic glycolysis – eye contains cells that transmit or focus light, and these cells cannot be filled with opaque structures such as mitochondria or densely packed capillary beds o Corneal epithelium generates most of its ATP aerobically from few mitochondria but still metabolizes some glucose anaerobically Oxygen supplied by diffusion from air o Lens of eye composed of fibers that must remain birefringent to transmit and focus light, so mitochondria nearly absent Small amount of ATP required (principally for ion balance) can readily be generated from anaerobic glycolysis even though energy yield is low Lens able to pick up glucose and release lactate into vitreous body and aqueous humor Doesn’t need O2 and has no use for capillaries Other Functions of Glycolysis Glycolysis generates precursors for biosynthetic pathways o Intermediates of pathway can be converted to ribose 5-phosphate (sugar incorporated into nucleotides such as ATP) o Sugars such as UDP-glucose, mannose, and sialic acid formed from intermediates of glycolysis o Serine synthesized from 3-phosphoglycerate, and alanine form pyruvate o Backbone of triacylglycerols (glycerol 3-P) derived from DHAP in glycolytic pathway Liver is major site of biosynthetic reactions in body o Synthesizes fatty acids from pyruvate generated by glycolysis o Synthesizes glucose from lactate, glycerol 3-P , and amino acids in gluconeogenic pathway o Many of glycolytic enzymes exist as isoenzymes with properties suited for above functions Bisphosphoglycerate shunt is side reaction of glycolytic pathway – 1,3-bisphosphoglycerate converted to 2,3bisphosphoglycerate (2,3-BPG) o RBCs form 2,3-BPG to serve as allosteric inhibitor of O2 binding to heme o 2,3-BPG reenters glycolytic pathway via dephosphorylation to 3-phosphoglycerate and functions as coenzyme in conversion of 3-phosphoglycerate to 2-phosphoglycerate by glycolytic enzyme phosphoglyceromutase Because 2,3-BPG not depleted by this, most cells need only very small amounts Regulation of Glycolysis by Need for ATP One of major functions of glycolysis is generation of ATP, so pathway regulated to maintain ATP homeostasis o PFK-1 and PDH (links glycolysis to TCA cycle) both major regulatory sites that respond to feedback indicators of rate of ATP utilization o Supply of glucose 6-P for glycolysis is tissue-dependent and can be regulated at steps of glucose transport into cells, glycogenolysis (degradation of glycogen to form glucose), and rate of glucose phosphorylation by hexokinase isoenzymes o All regulatory enzymes of glycolysis exist as tissue-specific isoenzymes, which alter regulation of pathway to match variations in conditions and needs in different tissues In liver, isoenzyme of pyruvate kinase introduces additional regulatory site in glycolysis that contributes to inhibition of glycolysis when gluconeogenesis activated AMP levels in cytosol provide better indicator of rate of ATP utilization than ATP concentration itself because concentration of AMP in cytosol determined by equilibrium position of adenylate kinase reaction (2 ADP AMP + ATP) o Equilibrium such that hydrolysis of ATP to ADP in energy-requiring reactions increases both ADP and AMP contents of cytosol o ATP present in much higher quantities than AMP or ADP, so small decrease of ATP concentration in cytosol causes much larger percentage increase in small AMP pool In skeletal muscles, ATP levels can drop by no more than 20%, but this causes ADP levels to increase 50% and AMP levels to increase 300% o AMP activates several metabolic pathways: glycolysis, glycogenolysis, and fatty acid oxidation (particularly in muscle tissues) ti ensure ATP homeostasis maintained Hexokinases exist as tissue-specific isoenzymes whose regulatory properties reflect role of glycolysis in different tissues; in most tissues, hexokinase is low-Km enzyme with high affinity for glucose o Hexokinase inhibited by physiologic concentrations of its product (glucose 6-P) – if glucose 6-P does not enter glycolysis or another pathway, it accumulates and decreases activity of hexokinase o In liver, isoenzyme glucokinase is high-Km enzyme not readily inhibited by glucose 6-P, so glycolysis can continue even when energy levels high, so anabolic pathways (synthesis of major energy storage compounds, glycogen, and fatty acids) can occur PFK-1 is rate-limiting enzyme of glycolysis and controls rate of glucose 6-P into glycolysis in most tissues o PFK-1 is allosteric enzyme that has total of 6 binding sites (2 for substrates [MgATP and fructose 6-P], and 4 for allosteric regulatory sites) o Allosteric regulatory sites occupy physically different domain on enzyme than catalytic site; allosteric effectors change conformation of active site and may activate or inhibit it o Allosteric sites for PFK-1 include inhibitory site for MgATP, inhibitory site for citrate and other anions, activation site for AMP, and activation site for F2,6P2 and other bisphosphates o Several different tissue-specific isoforms of PFK-1 affected in different ways by concentration of substrates and allosteric effectors but all contain the 4 allosteric sites o 3 different types of PFK-1 isoenzyme subunits exist: M (muscle), L (liver), and C (other tissues) Variable expression of subunits in different tissues, with some having more than one type Mature muscle expresses only M-subunit, liver expresses principally L-subunit, and erythrocytes express both M and L-subunits C-subunit highest in platelets, placenta, kidney, and fibroblasts but relatively common to most tissues Both M and L-subunits sensitive to AMP and composed of 4 subunits Within muscle, M4 form predominates; in tissues that express multiple isoenzymes of PFK-1, heterotetramers can form that have full activity o ATP binds to 2 different sites on PFK-1: substrate-binding site and allosteric inhibitory site Under physiologic conditions in cell, ATP concentration usually high enough to saturate substrate-binding site and inhibit enzyme by binding to ATP allosteric site – effect opposed by AMP, which binds to separate allosteric activator site For most PFK-1 isoenzymes, binding of AMP increases affinity of enzyme for fructose 6-P (shifts kinetic curve to left) Increases in AMP concentration can greatly increase rate of enzyme, particularly when fructose 6-P concentrations low o F2,6P2 – allosteric activator of PFK-1 that opposes ATP inhibition (different binding site than AMP) F2,6P2 not an intermediate of glycolysis but is synthesized by enzyme that phosphorylates fructose 6-P at 2-position (PFK-2) o PFK-2 is bifunctional enzyme with 2 separate domains: kinase domain and phosphatase domain At kinase domain, fructose 6-P is phosphorylated to F2,6P2 At phosphatase domain, F2,6P2 hydrolyzed back to fructose 6-P PFK-2 regulated through changes in ratio of activity of 2 domains In skeletal muscles, high concentrations of fructose 6-P activate kinase and inhibit phosphatase, thereby increasing concentration of F2,6P2 and activating glycolysis PFK-2 can be regulated through phosphorylation by serine-threonine protein kinases Liver isoenzyme contains phosphorylation site near amino terminal that decreases activity of kinase and increases phosphatase activity (phosphorylated by cAMP-dependent PKA and is responsible for decreased levels of liver F2,6P2 during fasting conditions (as modulated by circulating glucagon levels) Cardiac isoenzyme contains phosphorylation site near carboxy terminal that can be phosphorylated in response to andrenergic activators of contraction (i.e., norepinephrine) and by increased AMP levels – phosphorylation at this site increases kinase activity and increases F2,6P2 levels, thereby contributing to activation of glycolysis o Function of citrate-anion allosteric site is to integrate glycolysis with other pathways Inhibition of PFK-1 by citrate plays role in decreasing glycolytic flux in heart during oxidation of fatty acids In skeletal muscles, amount of aerobic versus anaerobic glycolysis that occurs varies with intensity of exercise, duration of exercise, type of skeletal muscle fiber involved, and level of training o Skeletal muscles usually combinations of type I (fast glycolytic fibers or white muscle fibers) and type IIb fibers (slow oxidative fibers or red muscle fibers) Designation of slow and fast refer to fibers’ rate of shortening, which is determined by level of isoenzyme of myosin ATPase present Compared with glycolytic fibers, oxidative fibers have higher content of mitochondria and myoglobin, which gives them a red color Gastrocnemius has high content of type IIb fibers, but these fibers will still produce lactate during sprints when ATP demand exceeds oxidative capacity Under ischemic conditions, AMP levels in heart increase rapidly because of lack of ATP production via oxidative phosphorylation o Increase in AMP levels activates AMP-activated protein kinase, which phosphorylates heart isoenzyme of PFK-2 to activate kinase activity, resulting in increased F2,6P2, which activates PFK-1 along with AMP so rate of glycolysis can increase to compensate for lack of ATP production via aerobic means Pyruvate kinase exists as tissue-specific isoenzymes designated R (RBCs), L (liver), and M1/M2 (muscle and other tissues o M1 form present in brain, heart, and muscle contains no allosteric sites, and pyruvate kinase doesn’t contribute to regulation of glycolysis in these tissues (these tissues don’t undergo significant gluconeogenesis) o L form can be inhibited through phosphorylation by cAMP-dependent protein kinase and several allosteric effectors that contribute to inhibition of glycolysis during fasting conditions Can be activated by fructose 1,6-bisP (ties rate of pyruvate kinase to that of PFK-1) and inhibited by ATP (signifies high energy levels PDH regulated principally by rate of ATP utilization through rapid phosphorylation to inactive form o Normally respiring cell with adequate supply of O2 – glycolysis and TCA cycle activated together, and glucose can be completely oxidized to CO2 o When tissues don’t have adequate supply of O2 to meet ATP demands, increased NADH/NAD+ ratio inhibits PDH, but AMP activates glycolysis; proportion of pyruvate reduced to lactate to allow glycolysis to continue During MI, ischemic area in heart has limited supply of O2 and blood-borne fuels; absence of O2 for oxidative phosphorylation decreases levels of ATP and increases AMP (which activates PFK-1 and AMP-dependent protein kinase), resulting in compensatory increase of anaerobic glycolysis and lactate production o Obstruction of vessel leading to heart decreases lactate removal, resulting in decrease of intracellular pH o At low pH levels, glycolysis inhibited and unable to compensate for lack of oxidative phosphorylation Lactic Acidemia Several methods can be used to determine lactate levels in blood o Conversion of lactate to pyruvate (which also converts NAD+ to NADH) in presence of lactate dehydrogenase Because NADH has considerable light absorption at 340 nm (and NAD+ doesn’t), one can follow increase in absorbance at this wavelength as reaction proceeds and determine levels of lactate that were initially present in sample To ensure all lactate is measured, hydrazine added to reaction because it reacts with pyruvate to remove product of LDH reaction, which forces reaction to go to completion o Lactate oxidase, which converts lactate (in presence of O2) to pyruvate and H2O2 Second enzymatic reaction measures amount of H2O2 produced (which removes product of lactate oxidase reaction, ensuring completion of reaction) – uses peroxidase and a chromagen, which is converted to colored product as H2O2 removed Amount of colored product produced allows lactate levels to be determined accurately Lactate production is normal part of metabolism; in absence of disease, elevated lactate levels in blood associated with anaerobic glycolysis during exercise In lactic acidosis, lactic acid accumulates in blood to levels that significantly affect pH (below 7.2) o Generally results from greatly increased NADH/NAD+ ratio in tissues – increased NADH concentration prevents pyruvate oxidation in TCA cycle and directs pyruvate to lactate To compensate for decreased ATP production from oxidative metabolism, PFK-1 (and therefore entire glycolytic pathway) activated Consumption of large amounts of alcohol, which is rapidly oxidized in liver and increases NADH levels, can result in lactic acidosis Hypoxia in any tissue increases lactate production as cells attempt to compensate for lack of O2 for oxidative phosphorylation Several problems that interfere with either electron-transport chain or pyruvate oxidation in TCA cycle result in lactic acidemia o Oxidative phosphorylation diseases (inherited deficiencies in subunits of complexes in electrontransport chain, such as myoclonic epilepsy with ragged red fibers [MERRF]) increase NADH/NAD+ ratio and inhibit PDH Pyruvate accumulates and is converted to lactate to allow glycolytic ATP production to proceed Impaired PDH activity from inherited deficiency of E1 (decarboxylase subunit) or from severe thiamine deficiency increases blood lactate levels Pyruvate carboxylase deficiency can result in lactic acidosis because of accumulation of pyruvate Lactic acidosis can result from inhibition of lactate utilization in gluconeogenesis (e.g., hereditary fructose intolerance caused by defective aldolase gene) If other pathways that use glucose 6-P blocked, glucose 6-P can be shunted into glycolysis and lactate production (e.g., glucose 6-P deficiency) Underperfusion of lungs causes decreased arterial PO2 and increased PCO2 – elevated CO2 content results in increase of H2CO3 and acidity of blood o Decreased O2 delivery to tissues results in increased lactate production from anaerobic glycolysis and elevation of serum lactate o Reduction in arterial pH is then a result of both mild respiratory acidosis (elevated PCO2) and more profound metabolic acidosis (elevated serum lactate level) Mechanism of Glyceraldehyde 3-Phosphate Dehydrogenase Glyceraldehyde 3-P dehydrogenase reaction converts glyceraldehyde 3-P to 1,3-bisphosphoglycerate o Can be considered 2 half-reactions Oxidation of glyceraldehyde 3-P to 3-phosphoglycerate Addition of inorganic phosphate to 3-phosphoglycerate to produce 1,3-bisphosphoglycerate o First half reaction is extremely favorable, but second half-reaction is unfavorable and doesn’t proceed under cellular conditions (ΔG0’ for both reactions negates each other to around 0) o Reaction accomplished by enzyme forming covalent bond with substrate, using essential cysteine residue at active site to form high-energy thioester linkage during course of reaction Energy that would be released as heat in oxidation of glyceraldehyde 3-P to 3-phosphoglycerate conserved in thioester linkage formed (such that ΔG0’ of formation of thioester intermediate from glyceraldehyde 3-P is close to 0) Replacement of sulfur with inorganic phosphate to form 1,3-bisphosphoglycerate relatively straightforward, as ΔG0’ for that conversion is also close to 0, and acylphosphate bond retains energy from oxidation of aldehyde o