Self-management support - California Health Care Safety Net Institute
Self-management support
Thomas Bodenheimer MD with lots of help from
Improving Chronic Illness Care
Self-management support is more than patient education
• Patient education
– Information and skills are taught
– Usually disease-specific
– Assumes that knowledge creates behavior change
– Goal is compliance
– Health care professionals are the teachers
• Self-management support
– Skills to solve patientidentified problems are taught
– Skills are generalizable to all chronic conditions
– Assumes that confidence yields better outcomes
– Goal is increased selfefficacy
– Teachers can be professionals or peers
Why is self-management support important?
• Every person self-manages his/her chronic condition. 99% of chronic care decisions are made by the patient away from the health care system
• The question is, does the person selfmanage well or poorly?
• Managing well improves clinical outcomes
Self-management support and compliance/adherence
• Compliance/adherence may not be helpful concepts
• Noncompliance or non-adherence assumes that 1) the patient has the information needed to make healthy decisions, and 2) the patient was involved in the decisions
• Often, neither 1) nor 2) is true
Compliance/adherence
• Compliance: “the extent to which a person’s behavior
(in terms of taking medications, following diets, or executing lifestyle changes) coincides with medical or health advice.” Lutfey and Wishner, Diab Care
1999;22:635.
• Adherence “the extent to which a patient’s behavior (in terms of taking medication, following a diet, modifying habits, or attending clinics) coincides with medical or health advice.” McDonald et al. JAMA 2002;288:2868.
Compliance/adherence
• Compliance and adherence are synonyms
• They are also the same as “patient selfmanagement behaviors” or “healthy behaviors”
• Use the term “healthy behaviors” as having the same meaning as compliance or adherence
• “Healthy behaviors” doesn’t compare patients with some professionally-set standard
Compliance/adherence
• For doctors, the word “compliance” (with practice guidelines) is appropriate
• Docs chose to be docs. They should held to a standard: do what’s evidence-based
• Patients didn’t choose to be chronically ill. They can’t be held to a standard
• For patients, the words “compliance/ adherence” are less appropriate
Many people fail to choose healthy behaviors because they lack information
• One study: 76% of patients with type 2 diabetes received limited or no diabetes education
• 300 medical encounters: doctors spent average 1.3 minutes giving information
• Another study: only 37% of patients were adequately informed about medications they were taking
Clement, Diab Care 1995;18:1204. Waitzkin. JAMA 1984;252:2441
Many people choose unhealthy behaviors because they lack information
• 50% of patients leave office visit not understanding what the doctor said
• Study of 264 visits to family physicians. During patient initial statement of the problem, physician interrupted after average of 23 seconds.
• Failure to provide information to patients about their chronic condition is associated with unhealthy behaviors. If people don’t know what to do, they don’t do it
O’Brien et al. Medical Care Review 1992;49:435. Kravitz et al.
Arch Intern Med 1993;153:1869. Roter and Hall. Ann Rev
Public Health 1989;10:163. Marvel JAMA 1999;281:283.
Information is necessary but not sufficient
• Information by itself does not improve clinical outcomes; people with diabetes gaining knowledge about their condition do not have lower HbA1c than those uninformed.
Norris et al. Diab
Care 2001;24:561
• An additional factor is needed
• That additional factor appears to be collaborative decision making, which makes the patient an active participant in his/her management.
Patients in empowerment classes have lower
HbA1c than controls.
Anderson, Funnell. Diabetes Care
1995;18:943.
Many people choose unhealthy behaviors because they were not involved in clinical decisions
• Study of 1000 physician visits, the patient did not participate in decisions 91% of the time
• When patients are involved in decisions, healthrelated behavior is improved and clinical outcomes (for example HbA1c levels) are better than if patients are not involved
Braddock et al. JAMA 1999;282;2313. Heisler et al. J Gen Intern
Med 2002;17:243. Greenfield et al. J Gen Intern Med 1988;3:448
Back to compliance/adherence
• One cannot expect a patient to “comply” with a physician’s advice if the patient doesn’t understand the advice
• One cannot expect a patient to “adhere” to a physician’s advice if the patient doesn’t agree with the advice
• Much “noncomplance/nonadherence” (i.e. unhealthy behaviors) is related to inadequate information-giving and lack of collaborative decision making
Does self-management support attempt to improve patient compliance/adherence?
• No, the purpose of self-management support is to encourage patients to become informed and activated
– By providing information
– By encouraging collaborative decision-making
– By assisting people to set their own goals
• Many (not all) patients will choose goals that do improve their health-related behaviors
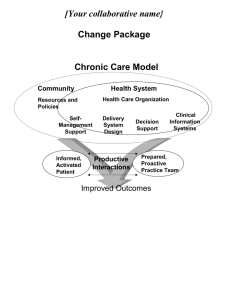
Chronic Care Model
Community Health System
Resources and Policies Health Care Organization
Self-
Management
Support
Delivery
System
Design
Decision
Support
Clinical
Information
Systems
Informed,
Activated
Patient
Productive
Interactions
Prepared,
Proactive
Practice Team
Functional and Clinical Outcomes
Informed, activated patient
Key conclusion:
Informed, activated patients have healthier behaviors and improved clinical outcomes
Golin et al. Diab Care 1996;19:1153. Piette et al. J Gen Intern Med 2003;18:624.
Francis et al. N Engl J Med 1969;280:535. Roter. Health Educ Monographs
1997;5:281. Greenfield, Kaplan et al. J Gen Intern Med 1988;3:448. Heisler et al. J
Gen Intern Med 2002;17:243.
Informed, activated patient
Requires:
Information-giving
Collaborative decision-making
These are the two parts of selfmanagement support
The 15-minute system
Short, unplanned MD visit, no team
Patient not taught about her illness
No collaborative decision making
Uninformed, passive patient
Unprepared practice team
We need to redesign primary care delivery systems to provide selfmanagement support, which creates informed, activated patients
Information-giving
Collaborative decision-making
The 5 A’s
• A clinical algorithm used for tobacco cessation
• Has become part of the US Public Health
Service guidelines on quitting smoking www.surgeongeneral.gov/tobacco/5steps.htm
• It has been adopted for other healthrelated behaviors
ASSESS
Knowledge
Beliefs,
Behavior,
Barriers,
Confidence
Self-management support in office practice
ADVISE
Provide personalized information about condition and benefits of change
ASSIST
Use motivational techniques and teach problem-solving
AGREE
Collaborative goal and action plan
ARRANGE
Follow-up and resources
Assess
• Knowledge
• Skills
• Importance
• Confidence
• Supports
• Barriers
• Risk Factors
Let’s look at Importance and Confidence
Bubble chart
Kate Lorig’s question: “Is there anything you would like to do this week to improve your health?”
Other things?
Physical activity
Reducing stress?
Taking medications
Healthy diet
Checking sugars
If patient picks a domain, assess readiness to make a change
• Readiness = importance and confidence
• If patient doesn’t think it’s important, he/she won’t make a change. Give information
• If patient thinks change is important, but has no confidence that he/she can change, assess and try to increase confidence
Assessing Importance
“How important do you think it is to exercise to improve your blood sugar?”
Not at all convinced
0 1 2 3 4 5 6 7 8 9 10
Totally convinced
Patient says 4
“Why 4 and not zero?”
“What would it take to move it to a 8?”
(From Keller and White, 1997; Rollnick, Mason and Butler, 1999)
Assessing Confidence
How confident are you that you can exercise to improve your blood sugar?
Not at all confident
1 2 3 4 5 6 7 8 9 10
Totally confident
Patient says 4
“Why 4 and not zero?
“What would it take to move it to an 8?”
Advise
Provide specific personalized information about the chronic illness, the health risks and the benefits of change
Advise: provide information
• Information-giving is disease-specific
• Telling people 150 facts about diabetes does not work. It is far more effective to find out what people want to know, and give them the information they want.
• Also, make sure people understand the information given them
• 2 tools
– Ask-tell-ask
– Closing the loop
Advise: Ask-Tell-Ask
• When patients are given a lot of information, they regain only a small amount
• Ask-tell-ask: Ask patients: “What do you know about your diabetes, and what would you like to know? When patients say what they want to know, tell them. Then ask again: what do you think about what you heard, and are there other things you want to know?
Advise
• A study of patients with diabetes found that in only12% of patient visits, the clinician checked to see if the patient understood what the clinician had told the patient
• This is called “closing the loop”
• In 47% of cases of closing the loop, the patient had not understood what the physician said
• When closing the loop took place, HbA1c levels were lower than when it did not take place
• Closing the loop should be an integral part of advising patients
Schillinger et al. Arch Intern Med 2003;163:83
.
Agree
Collaboratively select goals and an action plan to meet those goals
Action plan
1. Something you WANT to do
2. Describe
How
What
Where
Frequency
When
3. Barriers
4. Plans to overcome barriers
5. Confidence rating (1-10)
6. Follow-Up plan
Source: Lorig et al, 2001
Action plan: example
1. Something you WANT to do: Get more activity
2. Describe:
How: With friend
What: Walk
When: After lunch
Where: 3 times around block
Frequency: Mon, Wed, Fri, Sat
3. Barriers: Forget
4. Plan to overcome barriers: Put a note on fridge
5. Confidence rating (1-10): 7
6. Follow-Up plan: medical assistant will call me next week
Action plan
• Base goals on patient priorities
• Action plans are specific steps to help achieve goals
• Action plans should be easily achievable with confidence level 7 or greater
• Purpose is to increase self-efficacy: a person’s confidence that he/she can make changes to improve life
Assist
Problem-solving to help overcome barriers to achieving goals
Problem Solving
1. Identify the problem.
2. List all possible solutions.
3. Pick one.
4. Try it for 2 weeks.
5. If it doesn’t work, try another.
6. If that doesn’t work, find a resource for ideas.
7. If that doesn’t work, accept that the problem may not be solvable now.
Source: Lorig et al, 2001
Arrange
Schedule follow-up to provide ongoing assistance and support to adjust or change or problem-solve the action plan as needed
Arrange: follow-up
• Try a wide variety of methods, whichever patient prefers (in-person, phone, email)
• Make sure follow-up happens, patient trust can be destroyed by missed follow-up
• Use outreach and community opportunities
• Easiest is to see if patient wants to go a group, in which case follow-up takes place in the group
• Follow-up can be done by other patients (buddy system)
Opportunities for self management support
• Before the Encounter
• During the Encounter
• After the Encounter
From Russ Glasgow, PhD
Opportunities for self management support
Before the Encounter
• Pre-visit contact (phone, mail, e-mail, PDA, touchscreen computer, student, medical assistant)
• Pamphlets on “Talking to
Your Provider”
Pre-activation of patients
• 10 minute meeting with health educator to help patients formulate questions for physician led to more patient involvement in decisions
[Roter. Health Educ Monographs
1997;5:281]
• Interactive pre-visit booklet -- to write down agenda topics and learn techniques for recalling physician advice -- led to better retention of information and healthier behaviors -- lifestyle changes and medication use
[Cegala et al. Arch Fam Med 2000;9:57]
Pre-activation of patients
• 20-minute pre-visit meeting to prepare patients with diabetes to participate in decision-making
• Pre-activated patients had greater control over visit agenda (shown by audiotapes) than control patients
• Pre-activated patients had better HbA1c levels than control patients
Greenfield, Kaplan et al. J Gen Intern Med 1988;3:448
Opportunities for self management support
During the Encounter
• Assess what goals patient wants to work on
• See if patient willing to discuss action plan
• Information-giving (ask-tellask)
• Closing the loop
• Referral to community resource
Planned chronic care visits
• Group diabetes visits at Kaiser/Permanente led by nurse educator: significantly lower HbA1c levels and lower hospital use compared with controls
[Sadur et al.Diab
Care 1999;22:2011]
• Diabetes “mini-clinics” at Group Health in Seattle: for patients who regularly attended the clinics, better glycemic control than usual care patients
[Wagner et al.
Diab Care 2001;25:695]
Planned chronic care visits
• Nurse-led diabetes planned visit clinic had better HbA1c levels than controls
[Peters, Davidson.
Diab Care 1998;21:1037]
• Planned diabetes visits with nurse and endocrinologist had lower mortality and lower incidence of MI, revascularization, angina,
ESRD than control patients; median follow-up was 7 years
[So et al. Am J Managed Care 2003;9:606]
• Patients attending planned diabetes empowerment classes had lower HbA1c levels compared with controls
[Anderson, Funnell et al. Diab
Care 1995;18:943]
Planned chronic care visits
• Planned visits are essential to assist people to adopt healthy behaviors
• Planned visit is antidote to “tyranny of the urgent” -- acute issues crowding out chronic care management
• Visits can be with nurses, pharmacists, health educators, nutritionists, promotoras, or trained patients
• Group or individual visits
Opportunities for self management support
After the Encounter
• Referrals (health educator, medical assistant, community resource)
• Phone, e-mail, web follow-up
• Peer support (buddy system)
• Chronic disease selfmanagement course
Regular, sustained follow-up
• VA system: nurse-initiated phone contacts between visits improved glycemic control compared with usual care
[Weinberger et al. J Gen
Intern Med 1995;10:59]
• Cochrane Review: 5 RCTs -- better HbA1c levels in patients with regular follow-up compared with controls
[Griffin, Kinmouth. Cochrane
Library, Issue 3, 2001]
• Regular follow-up is a predictor of proper medication use
[Dunbar-Jacob. Health Psychology
1993;12:91]
Regular, sustained follow-up
• Diabetes education without regular follow-up is unlikely to result in longterm behavior change success
[Clement. Diab
Care 1995;18:1204]
• Follow-up can be done by visits with any caregiver, in groups, patient buddies, promotoras, telephone, e-mail, web
Chronic Disease Self-
Management Program
• Developed and studied by Kate Lorig and colleagues at Stanford
• Peer-leaders (patients with chronic illness), 6 sessions, 2 1/2 hours each
• Addresses multiple conditions
• Goal-setting, action plans, problem solving, skill acquisition
• Patients call each other between sessions
• Outcomes: improved health behaviors and health status, fewer hospitalizations; some improvements sustained for 2 yrs
Lorig et al. Medical Care 1999;37:5, 2002;39:1217
Who can do goal-setting, action plans, follow-up?
• Trained peers
• Health educators
• Nurses
• Physicians
• Medical assistants
• Students
• Any caring person...
Resources
• Book: Rollnick et al. Health Behavior Change. 1999.
• Book: Lorig, Holman, Sobel et al. Living a Healthy
Life with Chronic Conditions. 2nd edition. Palo Alto,
Bull Publishing, 2001.
• Bibliography on self-management: www.improvingchroniccare.org
• Download Action Plan forms in English, Spanish and
Chinese: www.action-plans.org
Web resources
• www.bayerinstitute.com
provides provider training in “Choices and Changes”
• www.motivationalinterview.org
has books, videos and training
• www.stanford.edu/group/perc home of Chronic
Disease Self-Management Program
Take-home points
• Self-management support includes
– Information-giving
– Collaborative decision-making
– Goal-setting/problem-solving
• It can be done before, during, and after a primary care visit. Planned chronic care visits are the ideal place
• A primary care physician cannot do selfmanagement support alone. It takes a team.