Assessing Children's Health: A Guide
advertisement

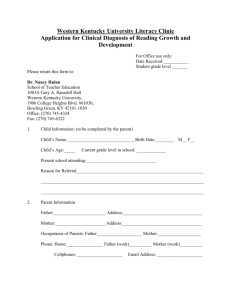
Chapter 3 Assessing Children’s Health ©2015 Cengage Learning. Health Information • Information about a child’s health is available in many forms and from a variety of sources. Health Information • It can be used to: – – – – assess and monitor a child’s health over time identify developmental problems formulate intervention plans make referrals and work with service providers – evaluate a child’s progress Child Health Histories • Information that families provide on health history forms can be useful for understanding the child’s: – Current developmental progress – Special health conditions or needs – Daily habits and preferences, such as eating and sleeping patterns and words used to express personal needs – Concept of family Medical and Dental Records • A complete physical form and immunization record are required for admission to early childhood and public school programs in most states. • Height, weight and BMI measurements provide reliable information about a child’s growth and well-being. Screening • Relatively quick, inexpensive, and efficient • Some tests can be conducted by teachers, • Others require the services of professional clinicians. • Designed only to identify children who may have a condition that requires professional evaluation, never to diagnose or confirm a specific impairment. Sensory System Assessment • Young children learn primarily through their sensory organs – eyes, ears, nose, hands, and mouth. • Teachers see children functioning in a variety of situations and can observe behaviors that may indicate a sensory problem. Vision • What behaviors might suggest that an infant or toddler may be experiencing a potential vision problem? (See Teacher Checklist 3-1) • What behaviors might indicate that an older child may have impaired vision? (See Teacher Checklist 3-2) • What evaluation procedures can be used to determine if a referral is necessary? Identifying vision problems – This is rather difficult until a child is in school. – A few tests are available for the younger child • Snellen Illiterate E • Teller Acuity Cards • Photo Screening – Children often do not know they have a problem, because they do not know what they are looking at. Common Vision Disorders • Amblyopia – a distortion and gradual loss of vision due to a muscle imbalance. – “lazy eye” • Strabismus – a condition in which the eyes appear crossed or not aligned equally. – crossed eyes • Myopia – nearsightedness; child may appear clumsy and ‘accident-prone’ Hearing • What behaviors might indicate a potential hearing problem in an infant or toddler? (See Teacher Checklist 3-4) • What behaviors might be observed in an older child? (Teacher Checklist 3-3) • What formal testing procedures are used to confirm or rule out a hearing disorder? Common Hearing Disorders • Conductive loss – interferes with the ability to hear and distinguish quiet sounds. • Sensorineural and mixed hearing loss – interfere with the child’s ability to hear and/or to interpret sound. Hearing Disorders • What modifications and instructional methods can teachers implement in the classroom to help children who have a hearing impairment? Speech and Language • Developmental milestones provide a functional measure for evaluating a child’s speech and language progress. • A hearing test should be a first step in assessing a child who may have a speech impairment or delay. • Referral for professional evaluation should be made if there are any concerns. Delayed language development or abnormal speech patterns that persist for more than a few months should be evaluated • • • • • • • • no speech by 2 years of age stuttering substitution of word sounds rate of speech that is too fast or unusually slow monotone voice no improvement in speech development speech by age 3 that is difficult to understand inattentive behavior or ignoring others Height and Weight • Measured at 4- to 6-month intervals • Recorded in their permanent health file • Measurements recorded on standardized growth charts allow comparisons to be made with previous data and can be useful The WHO Child Growth Standards Nutritional Assessment • BMI, appearance and behavior provide initial indicators of a child’s nutritional well-being. • Additional assessment tools include dietary/nutrient analysis, measurements compared to norms (e.g. BMI, head circumference), and laboratory tests. Common Nutrition Disorders • Malnutrition – a lack of sufficient food or essential nutrients. May be caused by limited access to food or unhealthy food choices. • Obesity – commonly due to a combination of excess food and calorie intake and inactive lifestyle. Childhood Obesity • In what ways does obesity challenge children’s health? • What can be done to avoid obesity and improve children’s weight management? Referrals • A comprehensive evaluation may be needed to identify a child’s health problem. • The evaluation process must take the child’s family and home environment into consideration. • Teachers should refer families to appropriate health professionals and support their efforts to follow through with recommendations. Case Study A friend encouraged Mrs. Howard to take her son to the developmental screening clinic being held this week at the community recreation center. Parker is nearly 2 years old and speaks only a few words that are understandable. He has few opportunities to play with other children his age because he spends most days with his grandmother while his mother works at a nearby hospital. On the day of the developmental screening, team members checked Parker's height, weight, vision, hearing, speech, cognitive abilities, and motor skills. The team leader also read through the child history form that Mrs. Howard had completed and noted that Parker had several food allergies, as well as frequent upper respiratory and ear infections. All of Parker's screening results proved to be within normal limits, with the exception of his hearing tests, which revealed a significant loss in one ear and a moderate loss in the other. Case Study Questions 1. Is Parker's speech development appropriate for his age? Explain. 2. What significance do Parker's ear infections have to his hearing loss? How might his food allergies be contributing to his hearing loss? 3. Should the screening team's recommendation for Parker include a referral to his physician? Why? 4. What behavioral signs of hearing loss might you expect Parker to exhibit? 5. What strategies might the developmental team suggest to Parker's mother and grandmother for improving his speech development and communication skills?