Diagnosis and Management of Urologic Injuries during Gynecologic
advertisement

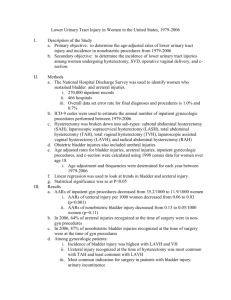
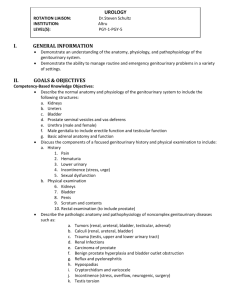
Diagnosis and Management of Urologic Injuries in Gynecologic Surgery Marisa Adelman, MD Assistant Professor Dept. Obstetrics & Gynecology Incidence • Hysterectomy (meta-analysis) – Overall urologic injury: 73/10,000 (0.73%) – Bladder injury: 5-66/10,000 (0.05-0.6%) – Ureteral injury: 2-40/10,000 (0.02-0.4%) • 19.7% repeat surgical rate with injury • 3.4% vesicovaginal fistula rate with injury • 2.4% ureterovaginal fistula rate with injury Adelman MR, Bardsley TR, Sharp HT. J Minim Invas Gyn, 2014. Incidence • Adnexectomy: – Ureteral injury: 0.1% • Pelvic organ prolapse: – Ureteral injury: up to 11% • Slings: – Bladder injury: • TVT: 3-9% • TOT: 0.5% Prevention and Detection • Bladder injury: 84.2% with delayed injury require reoperation • Ureteral injury: 60.7% with delayed injury require reoperation • Intraoperative recognition and primary repair: – Decreases secondary surgical procedures – Decreases morbidity: fistula and loss of renal function Dissection of the ureter • Selective dissection: – Presence of adhesions • Endometriosis • Prior surgery • Pelvic radiation – High-risk procedures • Malignancy • Fibroids near ureter • Routine dissection: – Results in bleeding – Can obscure anatomy – Can obscure tissue planes Bladder distension • Bladder is insufflated with liquid or C02 • Typical volume is 200250 mL • Laparoscopic guidance. Cystourethroscopy • Routine use recommended by ACOG for: – All prolapse and incontinence procedures with a 1-2% risk of injury to the urogenital tract: • TVT • Burch colposuspension • High uterosacral ligament vaginal vault suspension – High-risk procedures which may benefit: • McCall culdoplasty • Colpocleisis • Advanced vaginal and laparoscopic procedures • When injury rate exceeds 2% in hysterectomy – Cost-effective to perform routinely Cystourethroscopy • IV indigo carmine: – Evaluate for ureteral kinking or transection Following suspension procedures Following difficult dissections – Alternatives: • Oral phenazopyridine • Sodium fluorescein Universal preoperative stenting: Why consider it? • Cost of an undiagnosed ureteral injury requiring readmission and repair: – 1.72 times cost if repaired at time of injury – 2.29 times cost if no injury Schimpf MO, et al. BJOG, 2008. Universal stenting? • 12 year prospective randomized trial of >3,000 patients undergoing major Gyn surgery: – Universal stenting: 19 ureteral injuries – No stenting: 17 ureteral injuries • Decision analysis: – At a ureteral injury rate of 3.2%, universal stenting becomes minimally cost-saving. Chou MT, et al. Urogynecol J Pel, 2009. Universal stenting • The cost savings depends upon the injury rate Minimal benefit at common levels • Does not prevent injuries • May aid in recognition Limited data to support • Selective use may help identify the course of the ureter. Prophylactic stenting Prudent if extensive devascularization suspected: • Ureterolysis • Thermal injury Indocyanine green • Can be injected into the ureter • Fluoresces in response to near-infrared laser • Utilized in a variety of specialties: – Optho: retinal angiography – CV: Cardiac function testing – General surgery: intraoperative tissue viability Role of Urologists • 13,010 OB/Gyn procedures 98 consultation requests 29 for preoperative ureteral stents 69 cases of suspected injury • 32 bladder injuries 28 Dx’ed by operating OB/Gyn 23 to the dome, 9 to the posterior wall** • 11 ureteral injuries 1 Dx’ed by operating OB/Gyn Tx’ed with stenting, repair, and reimplantation** Hammad FT, et al. Int Urogynecol J, 2010. Intraoperative diagnosis Postoperative diagnosis Symptoms of Urologic Injury Cystotomy or ureteral defect Ureteral obstruction Fistula formation Intraureteral or intravesicle mesh Profuse drain output Flank or abdominal pain Urinary incontinence Hematuria Profuse wound leakage Anuria Watery vaginal discharge Dysuria Ileus Recurrent urinary tract infection Fever De novo urinary urgency Peritonitis Urge incontinence Hematuria Pelvic pain Cystography • Cystogram: – Plain film with instillation of radiocontrast – Information on integrity and contour • Voiding cystogram – Provides real-time information as the patient voids. – May demonstrate extravasation or ureteral reflux • CT cystogram – Addition of radiocontrast in the bladder prior to performance of a CT. Cystography Urography/pyelography • Intravenous pyelography (IVP) – Plain film x-rays following IV contrast administration. – Can identify stricture or obstruction. – Provides information on functionality. • Retrograde pyelography – Performed under fluoroscopy with cystoscopy – Contrast media is injected into the ureters • CT IVP • MRI IVP Pyelography Ultrasonography • Non-specific • Can visualize: – Hydronephrosis – Ureteral jetting – Free fluid/ascites • Identifies need for additional imaging. Choice of postoperative imaging High suspicion Bladder injury Cystogram or CT cystogram Urinary tract injury suspected Renal, pelvic, and bladder ultrasound ultrasound Ureteral injury or unknown location CT IVP or retrograde pyelogram Low suspicion Hydronephrosis and/or absent ureteral jets Ascites and/or fluid collection Suspect obstruction Suspect leak (bladder and/or ureteral) CT IVP or retrograde pyelogram CT IVP +/- CT cystogram Cystoscopy with retrograde pyelogram if non-diagnostic Diagnosis of a fistula • Suspected based on urinary pattern alterations: – Total urinary incontinence vesicovaginal fistula – Normal voiding with vaginal leakage ureterovaginal fistula • Confirmed with in-office testing: – Oral phenazopyridine prior to the study – Instillation of dilute indigo carmine or methylene blue into the bladder – Tampon placed in the vagina • Localized with imaging: – Cystoscopy vesicovaginal – IVP ureterovaginal – MRI Small or in close approximation to trigone Management: Bladder injuries • Dome – <2 mm: no repair, no prolonged drainage – >2 mm, <1 cm: drainage for up to 7 days – 1-2 cm: single layer absorbable suture – >2 cm: double layer absorbable suture • Foley drainage for 5-14 days, depending upon extent. – Multiple small cystotomies: • May be connected • Repaired as a single cystotomy. Management: Bladder injuries • Trigone: – May occur with injury to the ureters and urethra • Integrity of these structures must be assessed – Exposure may be difficult – Should involve someone with advanced urologic training. Role of cystography • Repair of simple defect: may not need cystogram prior to removing Foley. • Repair of complex defect: should obtain cystogram prior to removing Foley. • Time to bladder healing varies – If treating a 3-9 mm defect with drainage alone, perform cystogram prior to removing Foley. Management: Ureteral injuries • Kinking: – Remove suture to relieve kinking and obstruction • Ligation and crush: – Can cause devascularization – Remove stitch and assess viability – Stent for minor damage – Resect + anastomose or reimplant for major damage Stents and drains • Role of stents: – Promote healing – Prevent extravasation – Prevent stricturing • Role of drains – Keep anastomosis dry – Inform when leaking Management: Ureteral injuries • Laceration: – <1/2 diameter of ureter Repair over a stent Interrupted dissolvable sutures Drain placement – >1/2 diameter of ureter Treat like a transection Management: Ureteral injuries • Transection – Goals of repair: • Adequate debridement • Tension-free • Watertight – Repair by location: • Distal 1/3: Reimplantation +/- psoas hitch – Anastomosis acceptable if injury accessible • Mid 1/3: Anastomosis or reimplantation + boari flap • Proximal 1/3: Anastomosis or reimplantation + boari flap Management: Ureteral injuries • Thermal: – Stent for minor damage – Resect + anastomose or reimplant – Omental flap for vaginal incision or concomitant bowel injury in close proximity Ureteral repair follow-up • Foley catheter – Remove 1-2 weeks postoperatively Following cystogram confirmation of no leak • Ureteral stent – Remove 1-2 months postoperatively Followed by cystogram or IVP to assess the anastomotic site • Long-term function – Appropriate kidney function and absence of a stricture should be assessed at 3-6 months and 12 months Can be done with IVP, renal ultrasound, and serum creatinine Fistula management • Primary Tx: drainage – VVF: Foley catheter – UVF: Ureteral stent • Secondary treatment: surgical repair – VVF: incise epithelium around fistula mobilize tissue excise fistulous tract close defect in layers confirm water-tight bladder repair avoid overlapping suture lines. – UVF: incise above fistula reimplant ureter ligate distal portion of ureter near fistula. References • Adelman MR, Bardsley TR, Sharp HT. Urinary tract injuries in laparoscopic hysterectomy: a systematic review. Journal of minimally invasive gynecology. Jul-Aug 2014;21(4):558-566. • Brummer TH, Jalkanen J, Fraser J, et al. FINHYST, a prospective study of 5279 hysterectomies: complications and their risk factors. Human reproduction (Oxford, England). Jul 2011;26(7):1741-1751. • Lafay Pillet MC, Leonard F, Chopin N, et al. Incidence and risk factors of bladder injuries during laparoscopic hysterectomy indicated for benign uterine pathologies: a 14.5 years experience in a continuous series of 1501 procedures. Human reproduction (Oxford, England). Apr 2009;24(4):842-849. • Ibeanu OA, Chesson RR, Echols KT, Nieves M, Busangu F, Nolan TE. Urinary tract injury during hysterectomy based on universal cystoscopy. Obstetrics and gynecology. Jan 2009;113(1):6-10. References • Schimpf MO, Gottenger EE, Wagner JR. Universal ureteral stent placement at hysterectomy to identify ureteral injury: a decision analysis. BJOG : an international journal of obstetrics and gynaecology. Aug 2008;115(9):1151-1158. • Chou MT, Wang CJ, Lien RC. Prophylactic ureteral catheterization in gynecologic surgery: a 12-year randomized trial in a community hospital. International urogynecology journal and pelvic floor dysfunction. Jun 2009;20(6):689-693. • O'Hanlan KA. Cystosufflation to prevent bladder injury. Journal of minimally invasive gynecology. Mar-Apr 2009;16(2):195-197. • Siddighi S, Yune JJ, Hardesty J. Indocyanine green for intraoperative localization of ureter. American journal of obstetrics and gynecology. Oct 2014;211(4):436.e431-432. References • Lee Z, et al. Urology 2013; 82:729-33. • Hammad FT, AlQaiwani KM, Shirodkar SS. The role of urologists in the management of urological injuries during obstetric and gynaecologic surgery. International urogynecology journal. Oct 2010;21(10):1237-1241. • El-Tabey NA, Ali-El-Dein B, Shaaban AA, et al. Urological trauma after gynecological and obstetric surgeries. Scandinavian journal of urology and nephrology. 2006;40(3):225-231.