Clinical Assessment Ages 4-10
advertisement

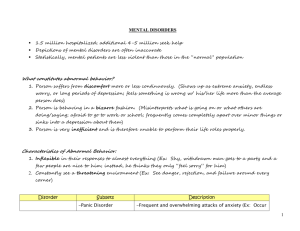
Clinical Assessment Ages 4-10 LAUSD School Mental Health Intern Training September 18, 2013 Danielle Mendez, LCSW Preparing for the First Session Purpose of the Clinical Assessment • Lays the foundation for an accurate diagnosis • Demonstrates medical necessity and the need for services. • Leads to appropriate selection of treatment plan objectives, services, and interventions • Is ongoing throughout the course of treatment Important Assessment Components: • Bio-Psycho-Social Assessment Interview(s) in which information is obtained from the client and the client’s parent/guardian (for minor clients). • Outcome Measures - SDQ • Mental Status • Other Relevant Documents or Sources* • Release of Information Risk Factors • Events that increase the likelihood of a negative outcome; can be acute or chronic Other Relevant Documents or Sources • • • • • • • • IEPs School Cumulative Records Psych Reports Previous or Current Service Providers Teachers and Other School Staff Family Members DCFS Social Workers Other Presenting Problem • Reason for referral • Current/primary symptoms/ behaviors/impairments in life functioning • Onset/duration/frequency History of Presenting Problem Symptoms/Behaviors Caregiver perception of cause Attempted interventions and responses Relevant Factors Environment (School/Home) Relationships (Loss/Separation) Traumatic Events Sexual/physical/emotional abuse Sleep Patterns Eating Patterns Hygiene Changes Prior Mental Health History Suicidality/Homicidality • # of attempts, method, access to lethal means • Interventions • When • Facility (Name or Type) • Type of intervention • Duration • Medication: dosage, response, adverse reactions • Recommendations • Response to treatment • Parent and Child • Satisfaction Substance Use/Abuse • Specify alcohol, drug type • Frequency of use • Duration • Pattern of use & last use Medical History • • • • • • Illness (Acute/Chronic) Medications Allergies Accidents Head Injuries Seizure/other neurological •Pregnancy •Sexually Transmitted Diseases •HIV •Vaccinations •Hospitalizations/Surgeries •Vision/Hearing •Dental Health Developmental History Prenatal Care Term/Months Birth Weight Age of Mother/Father/Marital Status Did mother use alcohol/cigarettes/drugs Illness/Accidents/ Stressors (family & environmental) during or after pregnancy Postpartum complications Developmental Milestones Infancy (0-3) • Motor – sit, crawl, walk • Speech; Eat; Sleep • Toilet training • Coordination • Temperament • Separation Developmental Milestones Early Years (4-6) • Social Adjustment • Separation • Sexual Behaviors • Self-Care Developmental Milestones Latency (7-11) • • • • • School adjustment Peer & adult relations/friends Interest/hobbies Impulse control Self-Care School History • • • • • • • • • Type of School Age & Grade Academic Performance Grade Retention Current/Past IEP School Changes: Attitude/Behavior Attendance/Truancy Suspension Child Abuse & Protective Services History • • • • • • • • Nature of Allegations/Abuse Age of occurrence Offender DCFS or Police Intervention Dependency Court or Criminal Court Action Child Response/Parents response to disclosure Placements and type Services and type Family History Family Composition • Siblings • Stepparents/others • Grandparents • Extended Family • Ethnicity/Culture Parent/Guardian Information • Education • Occupation • Socio-Economics • Religious Affiliation • Family History - medical, psychiatric alcohol/drug, legal/criminal Family History • • • • • Family Relationships (current and intergenerational) Quality of attachment (attunement balance & congruence) Disciplinary Style Conflict/Violence Problem Solving Mental Status Exam (MSE) • The aim of the mental status examination (MSE) is to be an objective description, not interpretation, of the child’s appearance, symptoms, behavior and functioning as manifested at the time of the examination. • A well-written MSE enables another clinician or the same clinician weeks, months or years later to have a clear picture of the patient’s mental state at the time of assessment. • The MSE is purely descriptive, includes no judgment of whether the appearance and behavior is normal or abnormal, clinically significant or non-significant. Mental Status – Cultural Considerations • There are potential problems when the MSE is applied in a cross-cultural context, when the clinician and patient are from different cultural backgrounds. For example, the patient's culture might have different norms for appearance, behavior and display of emotions. • Culturally normative spiritual and religious beliefs need to be distinguished from delusions and hallucinations without understanding may seem similar though they have different roots. • Cognitive assessment must also take the patient's language and educational background into account. Clinician's racial bias is another potential confounder. Children & Mental Status • There are particular challenges in carrying out an MSE with young children and others with limited language such as people with intellectual impairment. The examiner should explore and clarify the individual's use of words to describe mood, thought content or perceptions, as words may be used idiosyncratically with a different meaning from that assumed by the examiner. • In this group, tools such as play materials, puppets, art materials or diagrams (for instance with multiple choices of facial expressions depicting emotions) may be used to facilitate recall and explanation of experiences. The child’s stage of development should also be considered. Mental Status Components Component: Take Notice Of: May Be Used To Assess: Physical Appearance Age (actual and apparent) Age-appropriate clothes Grooming and cleanliness Differences in body structure, bruises, scars Height & Weight Physical features of alcohol or drug abuse Odor Tics, mannerisms Activity level Arousal level Coordination Unusual Motor Patterns Eye contact, quality, and movement Gait Repetitive purposeless movements Fluency Volume Rate Rhythm Articulation Language skill Stuttering Mutism Echolalia (repetition of another person’s words) Palilalia (repetition of one’s own words) Vocabulary Psychomotor Behavior Speech and Language Quality of Self-care Abuse or Neglect Medical Concerns Drug and Alcohol Use or Abuse Mood (Depression, Mania) Psychosis Neurological disorders Side effects of medication Tourette's syndrome Psychotic symptoms Autism Mania Delirium. Depression Medical condition Medical conditions Specific language disorders Autism Psychosis Mania Anxiety Depression Mental Status Components Component: Take Notice Of: May Be Used To Assess: Thought Content Overvalued ideas (a false belief that is held with conviction) Preoccupations Delusions Obsessions Phobias Quantity (i.e. poverty of thought) Thought Process Overall cognitive functioning Tempo (i.e. flight of ideas) Retarded or Inhibited thoughts Coherency of thought Perseverations Organization of thought (i.e. thought blocking, fusion, loosening of associations, tangential thinking, derailment of thought, circumstantial) Developmentally appropriate vocabulary Fund of knowledge Appropriate drawings Alertness (awareness of & response to environment) Orientation (to person, place, & time) Attention & concentration Memory (short & long term) Abstraction (the ability to categorize) Psychosis Obsessive Compulsive Disorder Personality Disorders Depression Clinical risk Anxiety Thought Disorders Mania Depression Anxiety Psychosis Personality Disorders Psychosis Anxiety Attention Deficit Intoxication Neuropsychological problems Side effects of psychiatric medications Chronic drug or alcohol use Brain damage including tumors Other brain disorders Mental Status Components Component: Take Notice Of: May Be Used To Assess: Mood Anxiety Depression Mania Ability to describe their mood state Affect Client's description of his/her mood Clinician’s observation of client mood: neutral, euthymic (reasonably positive mood), dysphoric (unhappiness), euphoric (elated mood), angry, anxious or apathetic (indifference or suppression of emotion). Emotion conveyed by the person's nonverbal behavior Appropriateness, intensity, range, reactivity and mobility Appropriateness to the current situation Congruency with their thought content Range and Reactivity of Affect Depression PTSD Psychosis Mania Personality Disorder Suicidal thoughts or behavior Self-harming behavior Thoughts or plans of harming others Risk-taking behavior Anxiety Depression Impulse control disorders Personality disorders Psychosis Mania Drug or alcohol abuse Eye contact Ability to cooperate and engage with assessment Behavior towards parents and siblings Cooperation, guardedness, hostility The quality of information obtained during the assessment. Examination of risk Attitude/Rapport Mental Status Components Component: Judgment Take Notice Of: May Be Used To Assess: Acknowledgement of problems Capacity to judge hypothetical situations Attitude towards receiving help Compliance with treatment Capacity to make sound, reasoned and responsible decisions Impulsiveness Planning ability Impaired judgment is not specific to any diagnosis but may be a prominent feature of disorders affecting the frontal lobe of the brain. If a person's judgment is impaired due to mental illness, there might be implications for the person's safety or the safety of others Recognition that one has a mental illness Compliance with treatment Ability to re-label unusual mental events (such as delusions and hallucinations) as pathological Adaptive capacity Assets Motivation for treatment Psychosis Dementia Client’s readiness for treatment Strengths to build upon in treatment Insight Strengths Suggested Questions for the MSE with Children What do you enjoy most? Why? What is your favorite movie/t.v. program? Tell me about it. What would you like for your birthday? If you had three wishes, what would you wish for? Why? What’s the nicest/worst thing that’s ever happened to you? What would you like to be when you grow up? Why do you think your mother/father/parents/grandma brought you to see me? Suggested Questions for the MSE with Children Do you have any friends? Who is your best friend? His/her name? What do you do together? How long have you been friends? Do you ever feel lonely? When? What do you do? What rules do you have in your house? What happens when you break a rule? Do you usually get blamed for things? What are your brothers and sisters like? Do you get along with them? Suggested Questions for the MSE with Children What things do you like best about school? What are the worst/hardest things? How do you get along with your teacher? Do you get into fights at school? Often? What makes you mad? What makes you sad? How is your mood most of the time (Happy, Sad, Mad, Scared)? Have you ever felt so bad you wished you could disappear? Die? Have you ever tried to hurt yourself? Maggie’s Story • “True Story” from a LA County Agency • 7 years old, female, African American • Presents with Depressive Sxs (irritability, daily crying outbursts, suicidal ideation, lack of interest in play), Anxiety Sxs (separation fears, cannot sleep alone, worries about family members and future), and Disruptive Behavior (“attitude”, noncompliance with adult commands, aggressive behavior towards sibs) • History of trauma and recent assault by male classmate who touched her in private parts Role Play the MSE • Get together with your elbow partner and take turns interviewing each other, and gathering information for the MSE, using the following “student” as the client. • You have 10 minutes to do this exercise. I’ll have you switch at the midpoint. • Have Fun! Thank You!