OST IN SOUTH ASIA Operationalisation & supply chain management
advertisement

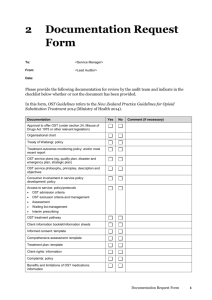
OST IN SOUTH ASIA Operational issues & supply chain management Contents of the presentation • OST programme in SA region - Current scenario • Scaling up OST in SA region • Supply chain management Contents of the presentation • OST programme in SA region - Current scenario • Scaling up OST in SA region • Supply chain management OST in South Asia Region COUNTRIES WITH OST • Bangladesh – Methadone • India – Methadone, Buprenorphine • Maldives – Methadone • Nepal – Methadone, Buprenorphine COUNTRIES WITHOUT OST • Bhutan • Pakistan • Sri Lanka Existing OST models in SA region • Different modalities of implementation – Setting (Hospital / NGO / Hospital – NGO) – Medications used (Methadone / Buprenorphine) – Activities/areas of OST implementation • Linking clients to OST centre (outreach services) • Assessment and dispensing (Clinic services) • Psychosocial services Bangladesh OST Programme • Initiated in July 2010 in partnership with Ministry of Home through icddr,b • Methadone as OST medicine • One centre in Dhaka – Client load ~ 150 OST clinic • Government hospital based clinic at the Drug treatment centre run by the Deptt of Narcotics Control, MoH • Outreach, psychosocial and clinic services provided within one single setting • Human resource: one medical doctor, 2 nurses, one counsellor, 8 outreach workers, one co-ordinator, 2 guards India OST programme • OST integrated in National AIDS Control Programme – Phase III • Three models operational – Buprenorphine • NGO based: 52 sites • Government –NGO collaboration: 15 sites – Methadone • Government hospital based: 5 sites piloted by UNODC NGO OST clinic • Run through NGOs implementing Harm reduction intervention programmes • Clinic in the Drop-in-Centre located in the vicinity of the IDU hotspots • Client load: 50 – 200 • Human resource: Doctor, 2 nurses, one counsellor, 2 outreach workers GO - NGO OST Government hospital • OST clinic located in Government hospital • Client load: 50 – 200 • Human resource: one doctor, 2 nurses, one counsellor, one data manager NGO • Outreach and follow up services provided by NGOs implementing Harm Reduction TI programmes • Human resource: One outreach worker, one programme manager MMT clinic • Run through Government De-addiction Centres, run by Ministry of Health • Referral of clients by NGOs working in the city/town • Client load: 50 – 100 • Human resource: one Doctor (part time), 2 nurses, one counsellor Nepal OST Programme – Re-initiated in the year 2007, as an emergency response – Pilots in partnership with Ministry of Home – OST medicine: Methadone, ? Buprenorphine – Currently operational through 3 units Government hospital • OST clinic located in Government hospital • Client load: 100 – 150 • Human resource: one doctor, 3 nurses, one counsellor, one data manager, 3 Guards NGO – SSU • Outreach, follow up and counselling services provided by Social Support Unit (SSU) managed by NGOs • Human resource: 5 – 7 staff Maldives • Initiated in the year 2009 • Partnership with nodal drug agency with the Ministry of Health • OST medicine: Methadone • One centre operational in Male` Government hospital • OST clinic located in Government premises • Client load: 70 • Human resource: one doctor, 2 nurses, 3 counsellors NGOs • Outreach, follow up and part-counselling services provided by 3 NGOs • Human resource: 3 – 5 staff Contents of the presentation • OST programme in SA region - Current scenario • Scaling up OST in SA region • Supply chain management Scale-up: Considerations • Setting the target – Universal access to HIV prevention services – 40% of IDUs to be covered with OST (Target setting guidelines, UNODC, UNAIDS, WHO, 2008) • However…. – Current coverage is < 3% in any country of SA region – Different countries are in different stages of IDU-HIV epidemic – Coverage is largely limited to IDUs, and not to opioid dependent drug users • Following the epidemic – Estimate IDU from major districts/provinces – Shortlist provinces with significant IDU estimates – Identify provinces without OST services – Categorize provinces based on IDU estimates (high, medium and low priority) • Prioritize provinces with moderate-high IDU-HIV prevalence • Choosing OST centres – Select models, medications based on in-country & regional experience – Shortlist potential centres – Conduct feasibility assessments • Accessibility to the clients • Infrastructure • Safety measures for stock-keeping • Training and capacity building – Sensitisation meetings for policy makers (one day) – Trainings • Induction trainings for core staff (5 days) • Exposure visits/study tours • Refresher trainings (3 days) – Develop in-country capacities – capacity building institutions • Staff selection – Defining roles & responsibilities • Establish Quality assurance mechanism – Develop tools for standardisation of operation (Standard operating procedures, operational guidelines) – Regular monitoring and evaluation of the programme – Success determined by registration and retention of clients into the programme – Factors influencing quality • • • • Dose of medication Duration of treatment Staff attitude Satisfaction of clients • Costing – Current costing: range from 30000 USD – 180,000 USD Start up cost • Sensitisation meeting • Training programmes • Feasibility assessment • Refurbishment of centres Implementation cost • Human resource • Medical doctor • Two nurses • One counsellor • Two outreach staff • One data manager • Accountant • Other support staff • Running cost - travel, communication Procurement cost • Medication • Buprenorphine: 37,000 USD • Methadone: 8,000 USD • Others: • Dispensers, water, etc. Contents of the presentation • OST programme in SA region - Current scenario • Scaling up OST in SA region • Supply chain management International regulatory framework • Different mechanism for narcotics / psychotropics – Methadone • Covered under the 1961 convention • Prior quota and annual consumption reporting required – Buprenorphine • Covered under the 1971 convention • Annual quota not required to be allocated • Annual reporting for Buprenorphine (optional) • Essential medicine list – WHO – Methadone and buprenorphine in the list Laws / policies of countries • Drawn in accordance to the conventions • Most of the countries support the use of narcotics / psychotropics for medicine and scientific purpose – India: use of opioids for OST (de-addiction) mentioned under NDPS act – Nepal: harm reduction and OST endorsed in the National Drug policy Supply chain mechanism Procurement Replenishment of stocks Supply Stock management Procurement procedures 1. Determining the medicine required – Methadone: syrup in 5 or 10 mg/ml strengths – Buprenorphine tablets: 8 mg, 2 mg, 0.4 mg, 0.2 mg 2. Determining the quantity – No. of patients X no. of days X average dose per patient per day 3. Request for QUOTA • Required only for Methadone • Nodal Ministry requests INCB for a quota for Methadone [Department of Narcotics Control (Bangladesh), Ministry of Home Affairs (Nepal), Central Bureau of Narcotics (India)] • Procuring agency – Each country has a nodal agency for procurement of goods and supplies • Maldives State Trading Organization • Nepal ‘Sajha’ trust – Negotiate rates with procuring agency (management cost) • Invitation for bids – Invite International Competitive bids • Bidding agency – Must have a WHO-GMP certificate or equivalent certificate – For export, supplier would need “Certificate of Pharmaceutical Product”(COPP) as recommended by WHO • Manufacturers / Distributors – Evidence of its technical, financial and production capability • Finalise vendor – Technical and financial qualification Negotiate Rates Establishing a supply chain mechanism SCENARIO A SCENARIO B Vendor Vendor Central stock Clinic Clinic Patient Patient Stock management Licenses from relevant authorities for storage and transport Central stocks Storage area of central stock Responsible officer for central stock Safe keeping: secure system Flow of stocks from central to OST clinic Chain of custody Clinic stocks Storage area Secure system Staff-in-charge? Record maintenance for stock management Central stock register Clinic stock register • Inventory of the stock to be maintained • Signed by the officer supplying the stock to clinic • Inventory of the stock to be maintained • Signed by the officer receiving the stock in clinic Dispensing register Daily stock register • Total quantity of methadone dispensed in the clinic in the given day • Information on the daily stock transaction being made Securing sustained supply: considerations Clear understanding of the various Ministries/departments dealing with quota, licensing and procurement Ensure clear commitment from the ministries – licensing, narcotics control / home Ensure procurement is made well in-advance Prepare a standard supply chain protocol / guideline Securing sustained supply: considerations Stock replenishment Stock projection Rotate stocks with eye on expiry dates Establish a strong supply chain mechanism Identify officers responsible in-charge of the stock at every point Maintain records strictly Check at regular intervals Conclusion • Opioid dependence is a chronic medical condition and requires long term therapy • Different modalities followed in different countries for operationalising MMT • Goal and objective of OST in each country – Treatment of opioid dependence – Prevention of HIV among opioid users, especially injecting drug users • Urgent need to scale up OST in South Asia region Conclusion • Advocacy for inclusion of narcotics / psychotropics in the national essential medicine list – Removal of import duties • Use of computer based software for stock management (copy right issues, monopoly of pvt sector !) • Robust supply chain an important part of scale up plan for OST THANK YOU