Travel and Tropical Medicine
Travel and Tropical Medicine
Roger Thomas, MD, Ph.D, CCFP,
MRCGP
OUTLINE: 6 KEY TASKS
1.
Past medical history, medications, vaccinations, planned travel, unplanned excursions and sports
2.
Update childhood vaccinations (MMR, polio, tetanus)
3.
Print off CDC data: ask patient read and underline
4.
Ask their understanding of risks
5.
Vaccinations and medications needed for trip
6.
Specific situations: (a) Mountain sickness (slide 10)
(b) Vaccines in pregnancy (14-18)
(c) Malaria: life cycle 19-20; prevention 21-23; chemoprophylaxis 24-31; treatment 32; clinical 33-40
(d) Traveller’s diarrhea: prevention; diagnosis; treatment
42-58
(e) Cholera 59; (f) Ebola 61; (g) Yellow Fever 62-65; (h)
Typhoid 66 (g) Dengue 66-69 (h) Schistosomiasis 70-1
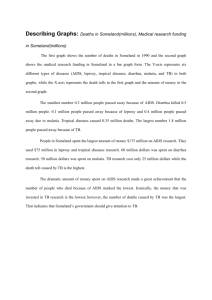
Global, regional, and national incidence and mortality for
HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study
2013. Lancet 2014
HIV
• 18 million new HIV infections (95% uncertainty interval
17 to 21 million)
• 292 million prevalent cases (281 to 317)
• 13 million HIV deaths (13 to 15)
• Due to interventions including PMTCT and ART, 191 million life-years (166 to 215 million) saved, 703%
(654% to 761%) in developing countries
• 101 countries (74 of which are developing) still have increasing HIV incidence
Global disease burden 2013
TB (HIV-negative)
• incidence 71 million (69 million to 73 million)
• prevalence 112 million (108 million to 116 million)
• deaths 13 million (12 million to 14 million).
• Annualised rates of change (ARC) for incidence, prevalence, and death negative after 2000.
• TB in HIV-negative individuals disproportionately occurs in men and boys 640% of cases (636 to 643) and 647% of deaths (608 to 703).
Global disease burden 2013
Malaria
• Cases rapidly increased 1990 to peak 232 million (143 to 387 million) in 2003
• 12 million deaths (11 to 14 million) 2004
• Since 2004, child deaths from malaria in sub-Saharan Africa decreased by 315%
(157% to 441%).
• Outside of Africa, malaria mortality steadily decreased since 1990.
Mortality from travel in developing world
• 50% is cardiovascular (older travelers with pre-existing cardiac condition), but rates are not increased by travel
• In younger travelers injuries are main cause of death: accidental death rate in
15-44 year olds is 2-3 times domestic rate
(MVA, scooters, drowning)
Traffic accidents worldwide
• 1.7 million deaths, major cause of death in males 15-45 (mostly urban pedestrians in developing countries)
• Of 309 Canadian travellers who died abroad,
25% accidents (mostly MVA)
• 1 death/million km in USA, 23 Sri Lanka, 44
Turkey; also high rates Egypt, Kenya, India, S.
Korea, Morocco
• 30 million injuries; in Ghana <10% pedestrian injuries reported
• Do not drive at night, rural areas; motorbike or bike
Let’s begin with a 60 year old going to Peru
• PMH: HTN, echocardiogram < 40% ejection fraction
• What are his/her travel plans? (3 months at agricultural research stations in
Amazonas and Madre de Dios regions, then archaelogical dig at high altitude)
• Review CDC website cdc.gov
• For the 6 basic planning tasks (slide 2) identify risks and prescribe
60 year old visiting Peru: Plan
• Update childhood vaccinations
• Check for egg allergy if plan MMR, influenza,
Yellow Fever vaccines
• GI risk: cholera? typhoid? Bacterial diarrhea?
Hepatitis? (Twinrix) Helminths?
• Yellow Fever?
• Malaria risks?
• High altitude sickness risks? (he/she is going to
Cuzco 3,500 meters rapidly by plane, no slow ascent; risks begin above 2,400 meters)
• PE from air travel to Peru (5/million?)
Acute Mountain Sickness, HACE, HAPE
• Acute Mountain Sickness: 22% adults ascending to 7000-9000 feet; 42% to 10,000;
75% to 15,000
• High Altitude Cerebral Edema: brain edema and increased intracranial pressure > Ataxia, confusion, disorientation, irrationality, lethargy, severe nausea and vomiting. Time to coma < 12 hours.
• High Altitude Pulmonary Edema: hypoxia causes increased PA pressure and fluid leaks, and a low hypoxic ventilatory response permits extreme hypoxemia, especially when sleeping
60 year old visiting Peru: CDC lists these risks
• At the country level CDC usually lists all risks and you need to be cautious and use other sources to assess relative risk
• Also you need to know if risks for travelers differ from locals with prolonged exposure
1. Dengue fever (avoid daytime bites from Aedes aegyptii ) Northern coastal and lowland urban areas. Peru not listed as dengue epidemic area
2. Malaria in certain regions
3. Yellow Fever. CDC recommends vaccination.
60 year old visiting Peru: CDC lists these risks
4. Filariasis (daytime bites from urban Culex fatigans and rural Anopheles mosquitoes transmitting Wucheria bancroftii) However, need chronic exposure to develop disease.
5. American trypanosomiasis (Reduviid (assassin) bug feces on skin transmitting American trypanosomiasis =
Chagas’ disease). However, need chronic exposure to develop disease. No cases in returning travelers
6. Bartonellosis (Oroya fever) on western slopes of Andes up to 3000 m. Very rare
7. Louseborne typhus in mountainous areas of Peru. Very rare.
Prevention of Acute Mountain Sickness
Kayser B. High Altitude Medicine and Biology 2012;13(2)
Acetazolamide N RCTs Relative risk 95%CI
250 mg/day
500 mg/day
750 mg/day
5
14
6
0.55
0.50
0.45
0.42, 0.74
0.40, 0.63
0.34, 0.61
Acetazolamide NNT to prevent AMS if climbing (AMS rate in controls 34%)
250 mg/day
500 mg/day
750 mg/day
6.5
5.9
5.3
NNT to prevent AMS if transport then climbing (AMS rate in controls 61%)
3.7
3.3
3.0
28 year old veterinarian, visiting Malawi,
South Africa, advising for WHO
• PMH: LMP 6 weeks ago, rising ΒHcG titres, planning to be in Africa during 1 st and 2 nd trimesters
• Risks to pregnancy?
• Malaria risks?
• GI risks?
• Rabies risks?
Vaccines in pregnancy
• All classes of maternal IgG transported across placenta, mostly in 3 rd trimester
• maternal IgG has half life of 3-4 weeks in infant, waning after 6-12 months of life.
• Strong evidence of benefits of vaccines
Canadian Immunization Guide
(2013) Recommended in pregnancy
Influenza inactivated vaccine
► High priority as increased risk of influenzarelated morbidity & adverse neonatal outcomes.
► No adverse events after H1N1 vaccine in
100,000 pregnant women in Canada and
500,000 in Europe.
►Pregnant women have 4 x hospitalisation rate for influenza compared to non-pregnant due to increased CVS volume, HR and O2 consumption).
► Avoid live vaccines, e.g. nasal
Canadian Immunization Guide (2013)
Recommended in pregnancy
Hepatitis B
► Test all pregnant women for HBsAg
► If no markers of Hep B infection and at high risk of Hep B during pregnancy, give complete series
Canadian Immunization Guide (2013) May be indicated in in pregnancy
• Hepatitis A, if travel to endemic area, as can cause severe disease in pregnancy.
No RCTs in pregnancy. No theoretical reason to suspect increased risk.
• Td. No increased adverse events
• Tdap. (acellular pertussis) If have not received as adult, give post-partum
• IPV (inactivated polio). May give if at increased risk of wild polio virus. Limited data.
Canadian Immunization Guide (2013) May be indicated in in pregnancy
• Pneumococcal. Review says is safe. Give if at high risk of invasive pneumococcal disease. To improve antibody response can given Pneu-C-13 vaccine then Pneu-P-23 8 weeks later. Cochrane review found insufficient evidence for protection of infant as an indication for maternal vaccination
• Meningococcal. Not studied in pregnancy.
Consider if high risk.
• Rabies. If exposed, give post-exposure prophylaxis
• Cholera & Japanese encephalitis vaccines not studied in pregnancy. Consider inactivated parenteral typhoid vaccine in high risk situations
Your 28 year old patient going to Malaŵi
• Assess risks using the 6 tasks on slide 2
• Provide vaccination advice
Malaria life cycle
• Hepatic stage: Sporozoites enter liver cells. Each
P. falciparum sporozoite asexually reproduces
30,000 merozoites; each P. vivax 10,000
• Erythrocytic stage: Hepatocytes burst and release merozoites into blood stream. Ring form matures and asexually reproduces 6-32 merozoites, which then invade other RBCs
• After 2 weeks some merozoites develop into gametocytes. If female mosquito bites a human and ingests them the gametocytes develop in her gut and 10 days later sporozoites can be injected into another human, the obligate host.
Malaria
• Incubation: for Plasmodium falciparum: hepatic stage (5-7 days) from bite to symptoms 8-25 (avg
12 days); erythrocytic stage (2 days)
• Partial immunity from long-term residence is against erythrocytic stages and diminishes within
6-12 months of leaving endemic area
• Clinical presentation: (clinical diagnosis is inaccurate as malaria is a great imitator; must do thick and thin films)
• Prodrome of tiredness, malaise and aching in the back, joints and abdomen, anorexia and nausea and vomiting. Tender splenomegaly. Conjunctivae suffused. Patient febrile for 2-3 hours before paroxysm.
Prevention of malaria
• Bednets & clothes impregnated with pyrethroids.
• Cochrane review by Gamble 2007 found for 4
RCTs of treated nets vs. no nets relative risks:
RR 95%CI
► placental malaria 0.79 0.66 to 0.90
► low birth weight 0.77 0.61 to 0.98
►m iscarriages/stillbirths 0.67 0.47 to 0.97
• Avoid going out at night, wear long sleeves and long trousers (80% of bites on ankles)
• Compliance with medication
Bednets (average use 42%) + chemoprevention, Uganda, 0-24 month olds
Bigira P. et al. Protective Efficacy and Safety of Three Antimalarial Regimens for the Prevention of Malaria in Young Ugandan Children: A
Randomized Controlled Trial. PLoS Med 11(8): e1001689. doi:10.1371/journal.pmed.1001689.
Intervention No of episodes of malaria per infant per year
Control 6.95
monthly sulfadoxine-pyrimethamine 6.73
5.21
Daily trimethoprimsulfamethoxazole monthly dihydroartemisininpiperaquine ( Protective efficacy 58% (95%
CI 45%–67%; p = 0.001
)
3.02
Malaria prevention: Domestic spraying
13 heterogeneous studies
•
Relative risk for reducing malaria prevalence
0.38 (95% CI 0.31 to 0.46)
•
More effective if:
► high initial prevalence
► multiple rounds of spraying
► DDT
► regions with a combination of Plasmodium falciparum and P. vivax malaria.
Kim D, et al. Reduction of malaria prevalence by indoor residual spraying: a meta-regression analysis.
Am J Trop Medicine Hyg 2012;87(1):117-24.
Chemoprophylaxis of malaria
• Causal prophylaxis: atovaquone and primaquine act on exo-erythrocytic cycle in liver
• Schizonticides: atovaquone, mefloquine, chloroquine, doxycycline, proguanil act on intra-erythrocytic parasites
• Terminal prophyaxis: Primaquine acts on latent hypnozoites in liver to prevent relapses in
P.Ovale and P. vivax
Chemoprophylaxis
Medication Adult dose Regimen Begin before exposure
End after exposure
1 day 7 days Atovaquoneproguanil
250/100mg Daily
Mefloquine 250mg Weekly
Doxycycline 100mg Daily
Primaquine * 30mg (base) Daily
*G6PD testing mandatory
1-3 weeks
1-2 days
1 day
4 weeks
4 weeks
3-7 days
Chemoprophylaxis of malaria: Mefloquine
62.5 mg weekly children 3 months – 5 years
125 mg weekly 6-8 years
187.5 mg 9-14 years
• 50% resistance Thai-Cambodian and Thai-
Burmese borders
• Questionnaires about adverse events:
1:6000 British soldiers, 1:10,000 European and 1:20,000 Canadian travellers
Mefloquine
• Side-effects: Headache, dizziness, confusion, vertigo, seizures, peripheral neuropathy, insomnia, dreams, anxiety, psychosis
• Only drug approved for 2 nd & 3 rd trimesters of pregnancy in chloroquineresistant areas. Limited data suggest safe for 1st trimester
• Do not prescribe for persons with major psychiatric disorders even if currently stable
Chemoprophylaxis of malaria:
Doxycycline
• Do not use children < 8 years and pregnant or lactating women
• 95% effective against
P. falciparum
• Adverse effects; abdominal pain, nausea, vomiting, diarrhea, photosensitivity (~
20%?), vaginal candidiasis (2.8%)
• Advantages: preventive for leptospirosis, rickettsial disases and traveler’s diarrhea
Chemoprophylaxis of malaria: Doxycycline
Atovaquone-Proguanil (Malarone)
• Acts on both liver and erythrocyte stages
• Efficacy 95-100%
• Adverse effects: Lowest withdrawal rate
(2%) for adverse effects compared to mefloquine and doxycyline
• Can be used in children > 5 kg
• Do not use if creatinine clearance
<30mL/min
Chemoprophylaxis of malaria: Primaquine
• Intended for radical cure of P. vivax
• Efficacy against
P. falciparum
Kenya 85%,
Irian Jaya (NE Indonesoia) 94.5%,
Colombian soldiers 94%
• Must test for G6PD deficiency; otherwise ˂
2% adverse effects
Pyrimethamine-dapsone
(Malaquine)
• PO 1 tablet = 12.5 mg pyrimethamine +
100 mg dapsone
¼ tablet weekly children 1-5 years
1/2 tablet weekly children 6-11 years
1 tablet weekly children >11 years and adults
Plasmodium falciparum malaria Treatment:
Artemisinin combination therapy
•
Recommended 1 st line therapy worldwide but decreased artemisinin susceptibility (slower parasite clearance time) reported in SE Asia.
•
27 clinical trials vs. comparators 1999-2009, intention-totreat analysis
•
15,017 (77% children < 6 years of age) patients treated for uncomplicated P. falciparum malaria, 44 sites in sub-
Saharan Africa
•
Average parasite load before treatment = 27,125/muL
Results:
•
Persistent parasitaemia Day 2 8.6%, 1.5% Day 3
•
Parasite clearance 31 hours (p=0.001 all comparisons)
Zwang J, et al. Plasmodium falciparum clearance in clinical studies of artesunate-amodiaquine and comparator treatments in sub-Saharan Africa, 1999-2009.
Malaria Journal 2014;13:114.
Malaria
• “Cold stage” of rigors (15-60 minutes):
► sudden feeling of cold and apprehension
► pulse rapid and low volume
► mild shivering turns into violent teeth chattering and shaking of the whole body.
Patients try to cover themselves with bedclothes
► core temperature is high but peripheral vasoconstriction with skin cold and goosepimpled
Malaria
• “Hot stage” up to 104F (2-6 hours): (“Ague attack” resembles the “endotoxin reactions” of lobar pneumonia or pyelonephritis)
► restless, unbearably hot, throws off all the bedclothes, excited
► severe throbbing headache, palpitations, tachypnea, postural syncope
► may vomit
► may become confused, convulse
► skin dry flushed and burning
► splenomegaly may be detected first the first time in this stage
• “sweating stage” (2-4 hours): temperature returns to normal and patient sleeps
WHO criteria for Severe malaria
Identify patients with severe malaria for special treatment with one or more of:
• Cerebral malaria
• Respiratory distress
• Severe normocytic anemia
• Renal failure
• Hyperparasitemia
• Pulmonary edema
• Hypoglycemia
• Circulatory collapse
• Spontaneous bleeding
• Generalised convulsions
Cerebral malaria (encephalitis)
• impairment of consciousness or generalised convulsion followed by coma
• high fever can cause irritability, obtundation, psychosis, and febrile convulsions (children) so urgently treat impairment of consciousness
• may thrash or lie immobile with eyes open or have dysconjugate gaze
Cerebral malaria (encephalitis)
• brainstem signs:
► doll’s eyes (in children)
► may be decorticate (flexion of elbows and wrists, supination of the arm) suggests severe bilateral damage to the midbrain
► may be decerebrate (extension of wrists and elbows with pronation of the arms suggests damage to the midbrain or the caudal diencephalon)
Cerebral malaria (encephalitis)
• children may have subtle convulsions
(nystagmoid eye movements, salivation, shallow irregular respirations, clonic movements of an eyebrow, finger, toe or mouth)
• with excellent care mortality is 15-20%; death within hours for children
• respiratory distress (compensation for metabolic acidosis), laboured breathing, intercostal recession, nasal flaring, accessory muscles of respiration)
Malarial Anemia (defined as < 5 g/dl):
• children with severe anemia usually have acidosis (deep Kussmaul breathing);
• malarial anemia kills as many children as cerebral malaria (mortality = 5-15%; mortality from acidosis = 24%; mortality from severe anemia + acidosis = 35%)
• also common in pregnant women
Jaundice and hypoglycemia in malaria
• Jaundice
1/3 of adults; associated with cerebral malaria, acute pulmonary edema
• Hypoglycemia
Anxiety, breathlessness, lightheadedness, tachycardia, impairment of consciousness, seizures, abnormal posturing can be misinterpreted as due only to the malaria
• Pregnant women:
► cell-mediated immunity is altered to favour survival of the fetus (more so in primigravidae), the placenta is heavily parasitized (the parasites adhere to chondriotin sulphate on the syncytiotrophoblast) The peripheral blood film may show no parasites
► risk is greatest for primigravidae in areas of unstable malaria
Provide advice to your 28 year old patient and her two children aged 2 and 4 going to
Malaŵi
• How to reduce the risk of malaria
• The symptoms of malaria
• Prescribe to reduce the risk of malaria
Large family going to a tropical country for wedding. They are worried about getting traveler’s diarrhea
• Advise on risks, precautions and treatment
• Risk of travellers’ diarrhea = 40% in high risk countries of Latin America, Africa and
S. Asia (unchanged over past 50 years)
Diarrhea in children in Asia and Africa (GEMS study, unpublished data first 2 years)
EPEC = : E coli enteropathogenic; ETEC = E coli enterotoxigenic.
Erlich P et al. Infections intestinales aiguës: vaccins actuels et futurs. Presse Med 2013;42:93-101.
Age 0-11 months 12-23 months
1 st Rotavirus Rotavirus/Shigella
2 nd Cryptosporidium
3 rd EPEC
Cryptosporidium/
Rotavirus
ETEC
4rd ETEC/Campylobacter jejuni
Shigella/Vibrio cholerae
5th Shigella Norovirus/Entamoeba histolytica
Norovirus
24-59 months
Shigella
Rotavirus
ETEC/Vibrio cholerae
Vibrio Cholerae/ campylobacter jejuni
Handwashing worldwide
Freeman MC. Hygiene and health: systematic review of handwashing practice worldwide and update on health. Trop Med Int Health 2013 19(8):906-916
• 42 studies; 19% of world population wash hands with soap and water after touching excreta
Studies
All studies
Excluding unblinded studies
RR diarrheal disease after handwashing
0.60
0.77
95%CI
0.53, 0.68
0.32, 1.86
TRAVELERS’ DIARRHEA: PREVENTION
1.
Hand washing: 30 seconds with soap
2.
Boil, cook or peel, eat when piping hot.
Avoid salads, ice cubes, food vendors, cans cooled in water, shellfish, undercooked seafood
► However, most travelers commit a food indiscretion within the first 72 hours due to being tempted by the sight of snacks, pre-paid buffets and the unavailability of hot food
► Studies of US naval ships abroad showed the more indiscretions ashore (salads, ice in drinks, food vendors … ) the more were on sick parade the next day with diarrhea.
TRAVELERS’ DIARRHEA: PREVENTION
3. Take a micropore filter. pass through a 1 micropore filter, so needs subsequent halogenation
Cryptosporidium can
4. Chlorine is less effective in acid or alkaline or cool water, so lengthen contact time (2 hours for Giardia, 10 minutes for bacteria).
Resistance to halogenation increases from bacteria, viruses, protozoan cysts, bacterial spores to parasitic ova and larvae
5. Potassium Permanganate to wash fruit and veg
6. Kettle to boil water (boiling for 1 minute kills even Cryptosporidium)
TRAVELERS’ DIARRHEA: PREVENTION
7. Pepto-bismol: 2 tablets qid reduces risk by 65%
(children > 3 years: 1 tablet qid)
► Indications: Prophylactic Pepto-bismol for a
short trip: Consider if immunocompromised, HIV+, severe inflammatory bowel disease, renal failure, poorly controlled insulin dependent diabetes. Or of you are a conference speaker or a musical performer who must be well at a specific time.
► Contraindications:
(a) 2 tablets have the salicylate content of one
325 mg aspirin, so contraindicated if allergy to aspirin, bleeding disorder, taking warfarin, history of GI bleed.
(b) If taking doxycycline: Pepto-bismol inhibits absorption of doxycycline (an important anti-malarial).
TRAVELERS’ DIARRHEA: PREVENTION
8. Dukoral cholera vaccine: 3 RCTs show provides no cross protection against ETEC.
9. Antibiotics: considering side-effects, best to use antibiotics for treatment in the case of diarrhea rather than prophylaxis
10. Rotavirus vaccines:
•
Rotarix (contains G1 serotype and P8), two doses at 2 and 4 months, 80% to 96 % effective in industrialised countries, 50% to 70% in developing countries
•
Rotateq (contains G1, G2, G3, G4 serotypes and P) three doses at 2, 4, and 6 months. 98% effective in in industrialised countries, 51% to 64 % in Asia and Africa.
Erlich P et al. Infections intestinales aiguës : vaccins actuels et futurs. Presse Med 2013;42:93-
101.
Inactivated cholera vaccine: Dukoral
Erlich P et al. Infections intestinales aiguës : vaccins actuels et futurs. Presse Med
2013;42:93-101.
• 67% effective against O1, not effective against O139 and other vibrios
• whole cell V. Cholerae O1 Inawa and
Ogaba strains + recombinant B subunit of cholera toxin
• 2 doses 1-6 weeks apart, lasts 2 years (for children 2-5 years 3 doses, lasts months)
Typhoid vaccines
Typhoid O live attenuated (oral)
(Vivotif (Berna)
Typhoid I
(Typhim Vi,
Typherix)
Route Dosing
Oral 1 Capsule days 1,3,5,7 in 4 oz warm water. 1 hour before or 2 hours after meal. Swallow not chew. Population of antibodysecreting cells peaks between 7 to
10 days after first dose. Each dose replicates 3-5 times then lyses over 48 hours. Maximum interval between doses must be <
72 hours and all capsules taken within 10 days.
IM 1
Minimum age
3 years
5 years
Vaccines for rotavirus, cholera, ETEC, shigella
DAS JK. Vaccines for the prevention of diarrhea due to cholera, shigella, ETEC and rotavirus. BMC Public Health 2013;13 Suppl 3
• 24 studies
• Rotavirus 74% mortality reduction
• Cholera incidence 52% reduction
• Mortality reductions for cholera, ETEC & shigella in children < 5 years: insufficient evidence
Your family going to a tropical country
• Advise them how to minimise risks of diarrhea
DIAGNOSIS of TRAVELLER’s DIARRHEA
• On a 3 week trip the indiscreet traveler is most likely to get diarrhea in the first week, and will need guidance about selftreatment.
• >60% is bacterial: Most common is E.
Coli, then Shigella, Salmonella,
Campylobacter (undercooked poultry)
• Attack rate remains same in long-term travelers and expatriates for several years
5 clinical syndromes of Traveller’s Diarrhea:
1. Watery diarrhea (60%)
• Mostly enterotoxigenic E. Coli ; also Salmonella,
Campylobacter, Vibrio parahemolyticus and vulnificus (seafood) .
• Parasites: Giardia, Cryptosporidium, Cyclospora &
Isospora
• 10% viruses (norovirus, rotavirus)
• Cause usually not identified
• Symptoms last 3-5 days and range from several watery stools/day to more explosive profuse but non-bloody diarrhea. Some may have nausea, cramps, vomiting, mild fever.
5 Clinical syndromes of Traveller’s Diarrhea
2. Dysentery (15%)
• Usually Shigella . Other causes: Salmonella,
Campylobacter, Yersinia, E. Coli serotype
0157:H7, more rarely non-colera vibrios and
Aeromonas
• Symptoms: small volume stools with mucous, high fever, abdominal pain and tenderness, prostration, feeling of incomplete evacuation.
Blood seen in only 50% of patients.
• Treatment: Treat all bloody diarrhea with antibiotics; fluids to prevent dehydration.
5 Clinical syndromes of Traveller’s Diarrhea
3. Acute gastroenteritis
• Vomiting, little diarrhea
•
Staph aureus
Incubation 2-7 hours, recovery in 12-18 hours
•
C. perfringens
Incubation 8-14 hours
• Bacillus cereus produces two toxins. One toxin produces symptoms like and the other like
Staph aureus
C. perfringens
• 4. Typhoid fever
Febrile illness and systemic toxicity. May or may not have diarrhea.
5 Clinical syndromes of Traveller’s Diarrhea
5. Chronic diarrhea, lasting > 14 days (3-5%)
• Usually
Giardia
or
Campylobacter.
Also enteroaggregative
E. Coli,
Aeromonas, Plesiomonas.
In many cases tests are negative and is attributed to postinfectious lactose intolerance and
IBS.
• Symptoms: vague abdominal pain, bloating, nausea, weight loss, low grade fever.
Diagnosing the type of diarrhea
• Check out your family’s diarrhea symptoms and diagnose
Treatment of Diarrhea while Travelling
1. Oral rehydration: Severe: WHO per L purified water
• sodium chloride 3.5 g
• Potassium chloride 1.5 g
• Sodium bicardonate 2.5 g
• Glucose 20g
• CeraLyte is rice based. If not available, make your own with 1 teaspoon salt and 2 tablespoons sugar or honey in 1 L water. Continue to drink even if vomiting.
• Moderate dehydration: drink 3 L water/day, add soup
+ salty crackers, avoid dairy
• Mild: infants - continue usual breast feeding/formula/ fluids
Treatment of Diarrhea while Travelling
2. Loperamide: 2 mg. capsules: two STAT then 1 capsule for every loose stool, max 16 mg/day reduces frequency of stools and duration of illness by 80% due to anti-motility and antisecretory actions.
• Young children are more susceptible to side effects: drowsiness, vomiting and paralytic ileus.
Not approved for children < 2 years.
3. Pepto-bismol (do not exceed 16 tablets/day): reduces diarrhea by 50% because of antiperistaltic and anti-secretary effects.
Treatment of Diarrhea while Travelling
• Need calories to repair gut cells so eat
• Steamed or baked fish, chicken, vegetables, toast, bananas applesauce, soup, soft drinks, dilute fruit juice, saltine crackers. Avoid dairy.
Treatment of Diarrhea while Travelling
• 4. Antibiotics: If copious or bloody stools, or fever.
► ciprofloxacin 750 mg once or 500 mg bid. If unwell continue for a total of three days.
HOWEVER: Resistance: 90% in Thailand, 50% Nepal,
40% Egypt
► Alternatives: levofloxacin 500 mg once or 500 mg daily x 3 days azithromycin 1000 mg once or 500 mg daily for 3 days (also effective against Shigella, Salmonella, E.
Coli, Campylobacter and typhoid fever. In Thailand more effective against ciprofloxacin.
Giardia and cannot get medical help.
Do not use with alcohol.
Campylobacter than
► metronidazole 250 mg tid x 5-7 days if you consider you may have
Treatment of Diarrhea while Travelling
• Reseve antibiotics for invasive enterocolitis with fever and dysentery, profuse diarrhea with more than three liquid stools within
12 hours. Duration of antibiotherapy 1 to
5 days.
• Treat pregnant women with ciprofloxacin, best alternative is azithromycin.
• Consider whether the rapid diarrhea is limiting antibiotic absorption.
•
Marchou B. Diarrhées du voyageur: épidémiologie, prévention et conduite à tenir. Presse Med.
2013; 42:76 –81.
Problems with fluoroquinolones
•
High resistance to fluoroquinolones in MRSA, P. aeruginosa, anaerobes, and pathogens isolated from
ICUs
•
Increasing resistance in community-acquired E.coli and
N. gonorrhea .
•
10-30% of community acquired respiratory tract infections (CARTIs), H. influenzae and S. pneumoniae harbour 1 st step mutations in quinolone resistance determining region. These mutants pass susceptibility testing unnoticed and are primed to acquire high-level fluoroquinolone resistance rapidly, especially in elderly and immunocompromised patients
•
Dalhoff A. Global Fluoroquinolone Resistance Epidemiology and Implications for
Clinical Use. Interdisciplinary Perspectives on Infectious Diseases 2012; Article ID
976273, 37 pages doi:10.1155/2012/976273
Problems with fluoroquinolones
•
1/3 to 2/3 of Enterobacteriaceae producing extended spectrum β -lactamases (ESBL) are also fluoroquinolone resistant, and others are primed to acquire high-level resistance during treatment.
•
Fluoroquinolones select for methicillin resistance in staphylococci, limiting use in skin infections
•
Co-selection of fluoroquinolone resistance by β lactams or aminoglycosides, and vice versa β -lactam- or aminoglycoside resistance by fluoroquinolones demonstrates that chemically unrelated drug classes select for drug resistant mutants and even multidrug resistant strains
Antiemetics for diarrhea
DAS JK The effect of antiemetics in childhood gastroenteritis. BMC Public Health 2013
Suppl 3
• 750,000 children < 5 die annually from gastroenteritis
Medication RR vomiting 95%CI
Rectal dimenhydrinate 0.60
0.44, 0.82
IV ondansetron
Oral ondansetron
IV metoclopramide
Total
0.50
0.35
0.80
0.46
0.24, 1.04
0.26, 0.46
0.50, 1.28
0.35, 0.61
Please treat your family’s diarrhea
• Discuss with your family their options and prescribe
Ebola
Schieffelin JS, et al. Clinical Illness and Outcomes in Patients with Ebola in Sierra Leone. NEJM
October 29, 2014DOI: 10.1056/NEJMoa1411680
•
10,100 cases reported in Guinea, Sierra Leone, Liberia, Senegal,
Nigeria, and Mali to October 25, 2014
•
Kenema Government Hospital, Sierra Leone: 213 patients symptoms of Lassa hemorrhagic fever or Ebola (106 Ebola)
•
Incubation: 6-12 days, symptoms to hospitalisation 6 days
•
Symptoms: fever (89%), headache (80%), weakness (66%), dizziness (60%), diarrhea (51%), abdominal pain (40%), sore throat
(34%), vomiting (34%), conjunctivitis (31%)
•
Rx: Fluids, 55% antimalarials, 93% antibacterials (ceftriaxone)
•
Prognostic factors associated with death: > 45 years, 38 °C, weakness, dizziness, diarrhea on presentation
•
Death: 33% if < 100,000 Ebola copies/ml of serum; 94% if >10 million copies/ml (P=0.003)
Yellow Fever
•
Marked underreporting of cases
•
45 endemic countries in Africa and Latin America (900 million)
•
< 550 million doses of yellow fever vaccine given worldwide. Planned vaccination of additional 174 million in Africa and Latin America 2011-2020 estimated will avoid 34,849 deaths
Brighton Collaboration definitions of serious adverse events after yellow fever vaccination:
•
Viscerotropic disease: “Multiple organ system dysfunction following vaccination, with spectrum from relatively mild multi-system disease to severe multiple system organ failure and death involving hypotension, hemorrhage, and acute renal and respiratory failure.”
Yellow Fever Vaccine is very safe
•
Encephalitis: “demonstration of acute inflammation of central nervous system parenchyma ( ± meninges) by histopathology.”
•
Anaphylaxis: “an acute hypersensitivity reaction with multi-organ-system involvement that can present as, or rapidly progress to, a severe lifethreatening reaction.” 1
• Published cases which meet Brighton
Collaboration criteria: neurologic criteria (1 death);
42 Viscerotropic Disease criteria (24 deaths) (includes 2 with both viscerotropic and neurologic criteria); 33
Anaphylaxis; 2 Wild Virus
• Published cases with insufficient detail to be
assessed with Brighton Collaboration criteria: 108 additional neurological cases, 58 viscerotropic cases
Yellow Fever
•
Unvaccinated traveler: the risk of disease during endemic periods = 1/267; death = 1/1,333 in an endemic African country (levels 10 times lower in South America)
•
Thomas RE , Lorenzetti D, Spragins W, Jackson D, Williamson T. A systematic review of yellow fever vaccineassociated serious adverse events.
World Health Organization. 1 December 2010
•
•
Thomas RE , et al. Active and passive surveillance of yellow fever vaccine 17D or 17DD-associated serious adverse events: Systematic review. Vaccine. 2011; 29(28):4544-4555.
•
•
Thomas RE , et al. Reporting Rates of Yellow Fever Vaccine 17D or 17DD-Associated Serious Adverse Events in
Pharmacovigilance Data Bases: Systematic Review. Current Drug Safety 2011;6(3): 145-154.
•
•
Thomas RE , et al. The Safety of Yellow Fever Vaccine 17D or 17DD in Children, Pregnant Women, HIV+
Individuals, and Older Persons: Systematic Review. J. Trop. Med. Hyg. 2012;86(2):359
–372. doi:10.4269/ajtmh.2012.11-0525.
•
•
Thomas RE, et al.Mortality and Morbidity Among Military Personnel and Civilians During the 1930s and World
War II From Transmission of Hepatitis During Yellow Fever Vaccination: Systematic Review. Am J Pub Health.
2013;103(3):e16-29. doi:10.2105/AJPH.2012. 301158)
Dengue
• Flavivirus with 4 serotypes DEN-1, DEN-2, DEN-
3, DEN-4. Infection confers long-term immunity only to that serotype
• Transmitted by Aedes aegyptii and Aedes albopticus , worldwide in tropics & subtropics
• 2.5 billion at risk
• 100 million/year. Most common Asia (esp
Thailand). Also Caribbean, Pacific islands,
Americas, 19,000 deaths/year
• No vaccine or medications available
Dengue Control
•
Due to impure water supply many houses in developing countries have open water containers.
•
Mosquitoes like to breed in water containers in or near houses
•
Integrated vector management most effective to reduce number of immature parasites per water container (relative effectiveness 0.12 (95% CI
0.02 to 0.62) [lower numbers show more effective]
•
Best to provide pure piped water
•
Erlanger TE, et al. Effect of dengue vector control interventions on entomological parameters in developing countries: a systematic review and meta-analysis. Medical and Veterinary Entomology (2008) 22, 203
–221
•
No evidence peridomestic spraying effective.
Esu E, et al.
Effectiveness of peridomestic space spraying with insecticide on dengue transmission; systematic review. Tropical
Medicine & International Health 2010;15(5):619-31.
Dengue Hemorrhagic fever (DHF) and shock syndrome (DSS)
•
250,000/year
•
DHF grades 1 and 2 = plasma leakage
•
DSS grades 3 and 4 = life-threatening shock (mortality
50x no shock)
•
Sudden onset high fever (5-7 days), headache, fatigue, severe myalgia, arthralgias, 50% maculopapular rash
•
Platelets < 100,000/mm 3
•
Capillary leakage: ascites, pleural effusion. US demonstrates 10x more cases than clinical exam
• Tourniquet test for capillary fragility: ≥ 20 petechiae/inch 2 after Bp cuff deflated
•
Mortality 10-20% but 0.2% in experienced hospitals;
Decreased mortality in Thailand over past 40 years
Dengue Shock Syndrome
DSS more likely if:
• serotype 2 in Thailand
• younger (children, immature immune system)
• female gender (differences in seeking care?)
• neurological signs
• nausea/vomiting, abdominal pain, gastrointestinal bleeding, hepatomegaly, increased ALT or AST
•
Increased hemoconcentration, ascites, pleural effusion,
• hypoalbuminemia, hypoproteinemia,, thrombocytopenia, coagulation dysregulation
• secondary infection
•
Huy NT, et al. Factors Associated with Dengue Shock Syndrome A Systematic Review and Meta-Analysis. PLoS
Negl Trop Dis 7(9): e2412. doi:10.1371/journal.pntd.0002412.
Dengue diagnosis
• immunochromatographic test (ICT) manufactured by Panbio. (Results in < 60 minutes)
• Sensitivity 0.45 to 1.0
• Specificity 0.57 to 1.0
• Diagnostic odds ratio 4.5 to 1287
• Positive likelihood ratio 2.3 to 59
• Negative likelihood ratio 0.01 to 0.56
•
Blacksell SD, et al. A systematic review and meta-analysis of the diagnostic accuracy of rapid immunochromatographic assays for the detection of dengue virus IgM antibodies during acute infection. Trans
Royal Soc Trop Med Hyg 2006;100(8):775-84.
Schistosoma haematobium (trematode)
• Africa and Egypt
• A human urinates eggs into fresh water, snails ingest eggs, replicate in snail, released into fresh water as cercariae, which then penetrate human skin (swimmer’s itch)
• Cercariae change to schistomules and migrate to lungs, causing Katayama syndrome 2-8 weeks after exposure
► high fever, cough, SOB, wheezing, headache, splenomegaly, urticarial rash
• Flukes then migrate to genitourinary venules and cause granulomas and calcification
S. mansoni and S. japonicum
• S. mansoni Africa and Brazil; S. japonicum
Asia (Laos)
• Humans excrete eggs in stool, and another human ingests them by mouth
• Final destination of schistosmules is mesenteric venules, causing granulomas and calcification
Resources
• www.cdc.gov
go to travelers, then destinations (best on line source)
• Canadian Immunization Guide , 8 th edition 2013. www.phac-aspc.gc.ca
• or www.naci.gc.ca
• Public Health Agency of Canada http://www.travelhealth.gc.ca
Includes official EBM statements from CATMAT (Committee to Advise on Tropical
Medicine and Travel), which are a bit wordy
• World Health Organisation www.who.int/ith
• Schwartz E. Tropical Diseases in Travelers.
Oxford: Wiley-Blackwell, 2009.
(good for specific diseases).
• Rose SR, Keystone JS. International Travel Health Guide.
(Philadelphia:
Mosby. (For patients, updated annually, chapter on each country, patients can buy this).
• Jong EC, McMullen R. (Eds.) The Travel & Tropical Medicine Manual . (4 TH ed.) Philadelphia: W.B. Saunders, 2008 (best short book).
• Keystone JS (ed.). Travel Medicine (2nd ed). Mosby Elsevier, 2011. Also online
• JeffreyHC, Leach RM. Atlas of Medical Helminthology and Protozoology .
Edinburgh & New York: Churchill Livingstone. (Outstanding, comprehensive, colour plates).