Schizophrenia
advertisement

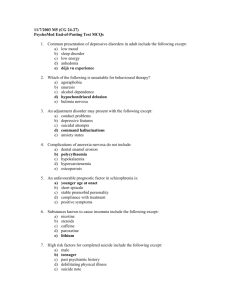
Schizophrenia History of Schizophrenia Diagnosis Emil Kraepelin (1856-1926): dementia praecox Eugen Bleuler (1857-1939): schizophrenia The Broadened U.S. Concept – Increased frequency of diagnosis – Process-reactive dimension Other U.S. diagnostic practices – Diagnose schizophrenia whenever delusions or hallucinations were present – Patients having a personality disorder were also diagnosed as schizophrenic DSM-IV Diagnosis Schizophrenia – Symptoms > 6 months Schizophreniform disorder – Symptoms 1 month - 6 months Brief psychotic disorder – Symptoms 1 day - 1 month Prevalence of Schizophrenia 1-2% of U.S. population 2 million diagnosed in U.S. Primary diagnosis in 40% state/county hospital admissions Low SES 3-8x higher prevalence Prevalence of Schizophrenia Median age at diagnosis = mid-20’s Men = Women prevalence – Men earlier diagnosis Worse premorbid history Worse prognosis Prognosis of Schizophrenia 10% continuous hospitalization < 30% recovery = symptom-free for 5 years 60% continued problems in living/episodic periods Schizophrenia Characteristic Symptoms: Two or more of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated): – delusions – hallucinations – disorganized speech (e.g., frequent derailment or incoherence) – grossly disorganized or catatonic behavior – negative symptoms, i.e., affective flattening, alogia, or avolition Social/occupational dysfunction Continuous signs for 6 months, at least 1 month of symptoms The DSM-IV Diagnosis DSM narrowed the range of individuals who could be diagnosed with schizophrenia in two ways: Explicit and detailed criteria Excluding other disorders – – – – Schizoaffective disorder Schizophreniform disorder Brief psychotic disorder Delusional disorder Course of Schizophrenia Prodromal phase Active phase Residual phase Symptom Distinction Positive symptoms – Deviant behaviors present Negative symptoms – Normal behaviors absent – Poor premorbid history – Poorer prognosis – Spouses less satisfied Positive Symptoms of Schizophrenia Disorganized Speech (thought disorder): problems in the organization of ideas and in speaking so that a listener can understand Delusions: Beliefs contrary to reality, firmly held in spite of evidence to the contrary (themes: control, grandeur, persecution) Hallucinations: sensory experiences in the absence of any stimulation from the environment Negative Symptoms of Schizophrenia Avolition: or apathy; a lack of energy and a seeming absence of interest in routine activities Alogia: a negative thought disorder: – poverty of speech – poverty of content Anhedonia: inability to experience pleasure Flat or Blunted Affect: virtually no stimulus can elicit an emotional response Asociality: severe impairments in social relationships Subtypes of Schizophrenia Paranoid – Delusions/Hallucinations have single theme = Persecution/Grandiosity – No thought disorder – Better prognosis Subtypes of Schizophrenia Catatonic – Hallmark = motor behavior Catatonic stupor Catatonic excitement Subtypes of Schizophrenia Disorganized (Hebephrenic) – Grossly disorganized cognition, affect, behavior – Poor prognosis Subtypes of Schizophrenia Undifferentiated – Does not meet criteria for other subtypes Diagnosis in First Episode (Lieberman et al., 1992) 1% Catatonic 3% Disorganized 19% Paranoid 54% Undifferentiated Etiology of Schizophrenia Summary of Family and Twin Studies Relation to Proband Spouse Grandchildren Nieces/nephews Children Siblings DZ twins MZ twins Percentage Schizophrenic 1.00 2.84 2.65 9.35 7.30 12.08 44.30 Biochemical Factors in Schizophrenia Problems with biochemical research Dopamine Activity – Effects of phenothiazines – Amphetamine psychosis Problems with Dopamine Hypothesis – HVA not found in greater amounts in schizophrenics – Phenothiazines rapidly block dopamine receptors, but effect on symptoms is slow – Excess or oversensitive dopamine receptors The Brain and Schizophrenia Autopsy studies indicate structural problems in the limbic areas and the prefrontal cortex CT scan and MRI studies reveal enlarged ventricles, suggesting deterioration or atrophy of brain tissue. PET scans suggest atrophy in the prefrontal areas. The Brain and Schizophrenia Evidence supports the hypothesis that a viral infection occurring during the mid trimester of fetal development may cause this brain damage It has been suggested that this early brain injury remains silent until the prefrontal cortex matures, typically in adolescence. Psychological Stress and Schizophrenia Social Class - the highest rates of schizophrenia are found in central city areas inhabited by people in having the lowest SES – Sociogenic hypothesis – Social-selection theory Family and Schizophrenia – Schizophrenogenic mother – Expressed emotion – High Risk Studies Treatment of Schizophrenia Treatments for Schizophrenia Insulin coma, prefrontal lobotomy, and ECT no longer used. Neuroleptics - anti-psychotic medications which are the most effective treatment for the positive symptoms of schizophrenia. Family Therapy - aimed at reducing the expressed emotion which predicts relapse Behavioral Therapy - social skills training has been found to improve social adjustment Treatment Today Outpatient and Inpatient Treatment – 80-90% hospital discharge rate – 40-50% readmission rate = revolving door $33 billion direct/indirect costs 2.5% of total health care expenditures Predictors of Good Outcome Good premorbid adjustment Acute onset Notable stressful life events Positive family environment More positive than negative symptoms More affective (vs. flat) symptoms Medication Atypical neuroleptics – Clozaril, Risperdal – Block 65% dopamine receptors, but more selective to frontal and temporal nerve tracts – Also increase serotonin Effectiveness of Medications Effective for positive symptoms – Atypical also effective for negative symptoms Decrease time in hospital Decrease relapse – 19% vs. 55% placebo 10-15% patients not helped by medication Side Effects of Medications Autonomic effects – Dry mouth – Drowsiness – Blurred vision Side Effects of Medications Extrapyramidal Effects – Tardive Dyskinesia - face, mouth, jaw movement 15% long-term regimens some not reversible can affect respiration