Presentation title - Person-Centred Care Resource Centre
advertisement

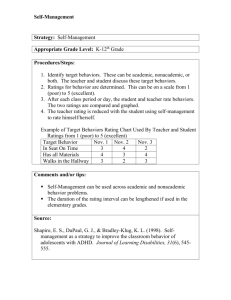
Introduction to Co-Creating Health Preparatory Workshop Welcome and Introductions • • • • Tutors All in group Name and area of work House keeping; -Manage self -All teach, all learn -Toilets -Fire alarm & exits -Refreshments -Mobile phones Aims Preparatory Workshop During this workshop you will have the opportunity to; • • • • • • • Understand the contextual background regarding the challenges for today’s healthcare economy with regard to Long Term Conditions (LTCs) Explore your knowledge, beliefs and understanding of Self Management (SM) and Self Management Support (SMS) Raise your awareness of the evidence base to support this approach Consider what you already do that works well to support SM Find out how to signpost people living with a long term condition to the parallel skills training programme for patients Understand the support tools available to help you change processes Start to develop your team’s action plan for SMS Pre-training questionnaire • • Please complete the pre training questionnaire (or other chosen version) and return to the facilitator. This questionnaire will be repeated at the end of the last workshop and will enable you to assess your development and will contribute to the programme evaluation • Thank you The Challenge – Long term Conditions (LTC’s) • • • • • • • • 15.4 million people in UK living with at least one LTC People with LTCs are far higher users of health and social care Accounts for; approx 69% primary and acute care budget in England Includes; 50% General Practitioner consultations, 65% of out-patient appointments and 70% of inpatient bed days Aging population and rising numbers At current rate of growth, expenditure on LTCs would increase by 94% by 2022 (with minimal real potential increase in NHS budget) Increasing pressure to improve quality and cost Our healthcare system is not currently configured to cope with the increased demand Meeting the Challenge • • No decision about me without me Equity and excellence: Liberating the NHS: The 2010 NHS white paper • • • 82% people living with a LTC want more support to self care Half those identified with LTC unaware of treatment options & no care plan GP Patient Survey 2008/9 - 61% surveyed felt discussion of care plan would result in better care The Co-Creating Health Programme; improve quality of healthcare services, increase personalisation and reduce costs • • http://www.dh.gov.uk Reflective exercise • • • • • • • • Exploring your philosophy – What do you think? Work in groups of two or three Discuss statements on the handout/next slide Score how much you agree with them on a scale of 0-10 (0=strongly disagree, 10=strongly agree) Each group start with a different statement Move onto the other statements Come back as a large group Discuss and debrief Statements • • • • The person with a long term condition is in charge of their own life and managing their condition(s) The person with a long term condition is the main decision-maker in terms of how they live with and manage their condition(s) The person with a long term condition is more likely to act upon the decisions they make themselves rather than those made for them by a professional The person with a long term condition and the health care professional are equals and experts The Year of Care Consultation Skills and Philosophy Toolkit © Year of Care v7 08/07/10 http://www.diabetes.nhs.uk/year_of_care Why Self-Management Support? Life with a long term condition: the person’s perspective Interactions with the service: planned or unplanned NB : People may also be accessing a wide variety of other support e.g. from within their communities What is Self-Management? What is SM? (Interactive discussion) • • • Self-management, by definition, is led, owned and done by people themselves The NHS cannot do self management to people, however it can create an environment where people feel supported and have increased confidence to self-manage This is not just about a change in service provision, but a cultural change, allowing people with long term conditions to be partners in their care, supporting them to decide what is important to them, what support they need, when they need it and how it should be available What is Self-Management Support? What is SMS? (Interactive discussion) • “Self-management support is what health services do in order to aid and encourage people living with long term-conditions to make daily decisions that improve health-related behaviours and clinical outcomes. It can be viewed in two ways: as a portfolio of techniques and tools; and as a fundamental transformation of the patient-caregiver relationship into a collaborative partnership” Tom Bodenheimer CHF 2005 • Personal Care Planning (is a process that) empowers individuals, promotes independence and helps people to be more involved in decisions about their care. It centres on listening to individuals, finding out what matters to them and finding out what support they need. • They are verbs not nouns! People who optimally self manage are; • • • • • • Optimistic Determined Contextually informed (health information that ‘makes sense to me’) Confident Problem solvers, decision makers People who inhabit rich social networks • Chicken and egg – however; All of these are amenable to change – often with simple interventions Active support works best There is a continuum. ─ There are many ways to support self management. ─ Some approaches are passive and focus on improving technical knowledge. ─ Other ways are more active and focus on changing confidence and behaviours. Research shows that more active support focused on confidence and behaviour works best to improve outcomes. 13 Self management works Research shows that supporting self management can improve: •self confidence / self efficacy •self management behaviours •quality of life •clinical outcomes •patterns of healthcare use A review of almost 600 studies found that when people are supported to look after themselves, they feel better, enjoy life more and have fewer emergency visits to GPs and hospitals. There is a lot of evidence from systematic reviews and randomised trials and much of the research is good quality. 14 Diabetes had at least one check up in the last 12 months and discussed ideas about the best way to manage their diabetes agreed a plan to manage their condition over the next 12 months discussed their goals in caring for their diabetes From ‘Managing Diabetes’ Healthcare Commission: 2007 Self management of warfarin and INR. Cochrane review Heneghan et al April 2010 1. 2. 3. Clinician management of warfarin and INR Self monitoring of INR and clinician advice re: warfarin dose Self management of INR and warfarin Compared to groups 1 and 2, group 3 have • same risk of bleeding • 50% fewer thrombotic episodes • 36% lower mortality Patient contacts by care setting Data is provided for 19 patients for whom a care planning approach has been implemented. Data includes patients with data is available for 12months prior to care planning and for 12 subsequent months. Costs: The unit costs of health and social care are derived by the Personal GP appointment £35 Social Services Resource Unit (PSSRU) annually. These costs are Outpatient attendance £126 applied to the activity levels for each type of contacts to estimate the A&E attendances £110 Acute admissions £1,317 financial impact of care planning. Over a 12-month period, care planning for the 19 patients in this study has reduced the total number of health care contacts from 529 to 246. The associated change in costs is a reduction from £47,346 to £17,860. Patient contact activity Patient contact costs (£) 400 350 300 250 200 150 100 50 practice visits out patient visits A&E attendences Acute admissions 20,000 18,000 16,000 14,000 12,000 10,000 8,000 6,000 4,000 2,000 practice visits out patient visits A&E attendences Acute admissions Co-creating Health: What are we trying to achieve? Our aim is to support people with long term conditions to develop the knowledge, skills and confidence to manage their own health and healthcare (to become activated). Co-creating Health supports people with long term conditions on their journey of activation Compared with people at low levels of activation, people at high levels of activation tend to live a higher quality of life, have better clinical outcomes and make more informed decisions about accessing medical services. 18 Levels of activation 19 The CCH Integrated Model 20 Health behaviour modeling Biological Biological Emotions / Thoughts Social / Behavioural 21 An Integrated Approach Service Improvement Programme Focus Patient Practitioner Development Programme Role change From passive patient to self-management Activation and partnership: confidence and skills Clinician/work force Self-management Programme Who From expert who cares to enabler who supports selfmanagement Building clinicians’ skills and addressing attitudes Service/processes Programme From cliniciancentred services to services that have self-management support as their organising principle Embedding the 3 enablers into everyday practice by building them into systems and care pathways 22 The Three Enablers Becoming an active partner Agenda setting – Identifying issues and problems – Preparing in advance – Agreeing a joint agenda – Exploring ambivalence, decisional balance Making change Goal setting & action planning – Small and achievable goals – Builds confidence and momentum Maintaining change Goal follow-up – Proactive – instigated by the system – Soon – mutually agreed and ideally within 14 days – Encouragement and reinforcement 23 Practitioner Development Programme Three x 3 hour skills development workshops Time interval between for practice Adult learning methods Co-facilitation lay and clinical tutor equal partnership Pre course reading Interactive exercises Large and small group discussion Based on three enablers – agenda setting, goal setting and follow up Experiential role play with simulated patient Goal setting and action planning between sessions Clinical communication skills, motivational interviewing, CBT approach Mapped to KSF & Appraisal/revalidation Evaluation Ongoing support & continued development Continuous improvement measurement tools PDP skills list • • • • • • • • • • • • • • Reflection/Empathy Explore agenda - something else - priority & expectation - clarify boundaries Explore beliefs self management Explore importance Explore confidence Support autonomy & choice Explore ambivalence Invite goals Ask before advise Problem solving Action planning Follow up Self management programme for Patients (SMP) • • • • • • • • Skills development programme Co-facilitation lay and clinical tutor equal partnership Combination of education, interactive learning and role play Based on three enablers – agenda setting, goal setting and follow up Each session follows up goals set for the week and sets new goals for the following week Seven 3 hour workshops at weekly intervals Follow up support, but aims to build effective peer support. Skills descriptor list SMP Skills list • • • • • • • • • • • Goal setting and action planning Problem solving Follow up Pacing and balancing life Communication – with family, friends and effectively with clinicians Agenda Setting Making choices, deals and decisions. Relaxation & mindfulness Managing setbacks Handling and challenging difficult emotions Planning to stay well Self Management Programme outcomes Produces statistically significant changes in: • positive engagement with life • constructive attitude/approach towards condition • more positive emotional well being • using self-management skills and techniques Person living with a long-term condition “I used to go to the doctor only when they summoned me, and then say ‘What are you going to do to fix my problem?’. But now I’m saying like, ‘I’m not sure these particular painkillers are working the way we hoped, can we try something else? What could I do myself? ’ “ 28 Self management programme signpost process and information leaflet • • • • Describe your local signposting process with examples of relevant documentation The lay co-facilitator can share their experience of the SMP together with any key messages Describe local data for total numbers, completed and outcomes Update this information regularly Does CCH improve diabetes control? Results from The Whittington Hospital, 2010 30 Patient Activation and Self Efficacy Outcome Measure Score 80 Pre SMP 70 6 Months Post SMP 60 50 40 30 20 10 0 PAM PSEQ Results Pre and Post SMP from NBT and CHFT, August 2010 Examples of improvement ─ A Cochrane review of 36 trials found that self monitoring and agenda setting reduced hospitalisations, A&E visits, unscheduled visits to the doctor and days off work or school for people with asthma (Gibson et al 2004). ─ A US trial found that personalised goal setting for older women with heart conditions reduced days in hospital and overall healthcare costs (Wheeler et al 2003). ─ A trial found that telephone support may improve self care behaviour, glycaemic control, and symptoms among vulnerable people with diabetes (Piette et al 2000). ─ US researchers found that motivational interviewing helped improve self efficacy, patient activation, lifestyle change and perceived health status (Linden et al 2010). ─ A large meta analysis found that individual education and group sessions improved symptoms for people with high blood pressure (Boulware et al 2001). 32 Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? Understanding the problem. Knowing what you’re trying to do - clear and desirable aims and objectives Measuring processes and outcomes What have others done? Langley G, Nolan K, Nolan T, Norman C, Provost L, (1996), The improvement guide: a practical approach to enhancing organisational performance, Jossey Bass Publishers, San Francisco Act Plan Study Do What hunches do we have? What can we learn as we go along? Outcome Secondary Drivers Organisational Changes Patient / Clinician Engagement Pre Visit Changes The 3 Enablers During Visit Changes Patient Confident in Self Management Ideas for Change Agenda Setting Goal Setting Goal Follow Up Post Visit Changes 34 Appendix 2 Self Management Questionnaire To help us to continually improve our services we would be grateful if you would kindly answer the following 6 questions. HAVE YOU ATTENDED A SELF-MANAGEMENT PROGRAMME? In your consultation today: YES/ NO (please circle) (please circle) YES/ N0 1. Did you Discuss what was most important to You in managing your own health? 2. Did you Get support to set a short-term goal for yourself? YES/ N0 3. Did you Arrange to discuss your progress on your short-term goal? YES/ N0 4. How supported did you feel in managing your health? 10 9 8 7 6 5 4 3 2 1 0 Totally Not at all supported supported “I am confident that I can manage my health condition” 10 9 8 7 6 5 4 3 2 1 0 Strongly Strongly agree disagree Evaluation & measuring success • • • • • Practitioner longitudinal questionnaire Workshop evaluation Patient feedback questionnaire – The self management questionnaire, CARE measure Measurement tools for continuous service improvement (PDSA) Referral rates to SMP You may also wish to consider measuring; • • Qualitative data capture Health economic data such as length of stay, reduced emergency admissions, increased referral and completion rates for disease specific programmes such as pulmonary rehabilitation and diabetes programmes Examples of Activating interventions •Patient held record •Negotiated agenda setting •Patient access to record •Information sharing •Results sharing •Supported goal setting •Agenda setting sheets •Supported problem solving •Access to information •Follow up on goals •Self management programmes •Peer support groups •‘Buddy system’ Implementing activating intervention(s); • Which activating intervention can you develop in your team or practice that will impact activation and confidence for people living with a long term condition(s)? • Agree one which you will work on before the next session • Nominate an improvement lead who will co-ordinate goal setting and action planning for this • All contribute and all support Activating intervention- goal setting and action planning • Work in groups of three • On a scale of 0-10 consider how important it is that you/your team support your chosen activation intervention? (0=no importance 10=maximal importance • Set a SMART goal and develop your action plan to progress implementation of your chosen activating intervention between now and the next session. • On a scale of 0-10 how confident are you that you/your team can do this? (0=no confidence 10=maximal confidence) • Explore what things would need to happen to increase this confidence? Next steps • Three skills development workshops – List dates and venues • Start to use the ‘Self Management Questionnaire’ with people that you see who are living with a long term condition. • Agree action plan for activating intervention activity between now and next workshop. • Consider how you will embed signposting to Self Management Programme or how you will find out what programmes are available locally. • If there are no local programmes start considering how can you deliver Self Management skills training for your local population?