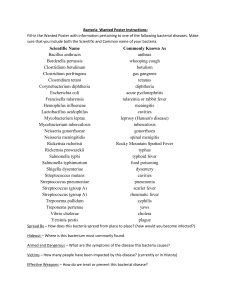
Gram Positive Bacteria
advertisement

Bacterial Diseases Victor Politi,M.D., FACP, Medical Director, SVCMC School of Allied Health Professions, Physician Assistant Program Introduction Bacteria consist of only a single cell Bacteria fall into a category of life called the Prokaryotes There are thousands of species of bacteria, but all of them are basically one of three different shapes. Classification of Bacteria Until recently classification has done on the basis of such traits as: shape bacilli: rod-shaped cocci: spherical spirilla: curved walls ability to form spores method of energy production (glycolysis for anerobes, cellular respiration for aerobes nutritional requirements reaction to the Gram stain. Classification of Bacteria The Gram stain is named after the 19th century Danish bacteriologist who developed it. The bacterial cells are first stained with a purple dye called crystal violet. Then the preparation is treated with alcohol or acetone. This washes the stain out of gram-negative cells. To see them now requires the use of a counterstain of a different color (e.g., the pink of safranin). Bacteria that are not decolorized by the alcohol/acetone wash are gram-positive Gram Positive Bacteria I-Gram Positive Cocci A-Streptococcus (e.g. streptococcus Pneumoniae) B-Staphylococcus (e.g. Staph. aureus) C-Enterococcus (Previously Group D Strep.) II-Gram Positive Rods A-Corynebacteria: Corynebacterium diphtheria B-Listeria monocytogenes C-Bacillus anthracis (Anthrax) D-Erysipelothrix rhusiopathiae III-Gram Positive Branching Organisms A-Actinomycetes Gram Positive Cocci I-Beta-hemolytic Streptococcus (Lancefield Groups) Group A Streptococcus (Streptococcus Pyogenes) Group B Streptococcua (Streptococcus agalactiae) Group C Streptococcus Group G Streptococcus II-Alpha-hemolytic Streptococcus Streptococcus Pneumoniae (Pneumococcus) - Viridans streptococcus (bacterial endocarditis) III-Non-hemolytic Streptococcus Streptococcus faecalis (Group D) Certain members of Groups B, C, D, H, and O Strep throat is caused by group A Streptococcus bacteria. These bacteria are spread through direct contact with mucus from the nose or throat of persons who are infected, or through contact with infected wounds or sores on the skin Group B Streptococcus (Streptococcus agalactiae) Epidemiology Most common US cause of neonatal sepsis and meningitis Incidence Overall: 2 to 4 per 1000 live births Invasive: 1.8 per 1000 live births Primarily occurs in newborns Very rare after 5 months of age Group B Streptococcus (Streptococcus agalactiae) Pathophysiology Group B Beta-hemolytic streptococcus infection Perinatal transmission Delivery via a birth canal colonized with GBS Incidence of U.S. vaginal GBS colonization: 15-20% Onset of infection (Mean onset 20 hours of life) Early onset neonatal disease (<6 days of life in 80%) Sepsis Pneumonia Late onset neonatal disease of sepsis or mengitis Group B Streptococcus (Streptococcus agalactiae) Labs: Maternal Screening GBS Culture Management Sepsis (treat for 10-14 days) Meningitis (treat for 14-21 days) Pencillin G 200,000 units/kg/day divided q4-6 hours Penicillin G 400,000 units/kg/day divided q2-4 hours Prevention Perinatal Group B Streptococcus Prophylaxis Prognosis Mortality 10-40% Streptococcus Pneumoniae (Pneumococcus) Epidemiology Most common cause of community acquired pneumonia Classic Symptoms Shaking rigors Fever Purulent sputum Rust colored Pleuritic chest pain Dyspnea Chest splinting Alpha-hemolytic Streptococcus Lab CBC Gram stain Positive in only 33% of cases Sputum culture Gram positive encapsulated organisms Elongated lancet shaped diplococci Blood Culture WBC elevated with left shift Positive in only 40% of pneumococcal pneumonias Radiology Chest X-ray Lobar consolidation (often lower lobe) patchy infiltrates Management Increasing Pencillin Resistance Penicillin Sensitive Ampicilin IV or Amoxicillin PO Erythomycin Azithromycin Clarithromycin Penicillin G IV Doxycycline Oral second generation cephalosporin Parenteral third generation cephalosporin Management High-Level Penicillin Resistance Broad spectrum Fluoroquinolone Levofloxacin Gatifloxacin Grepafloxacin Moxifloxacin Sparfloxacin Parenteral third generation Cephalosporin High dose Ampicillin Vancomycin IV with or without Rifampin Gram Positive Cocci Organisms -Staphylococcus aureus -Staphylococcus epidermidis Pus smear (wound) Staphylococcus aureus Enterococcus I-Characteristics Gram Positive Cocci Previously defined as Group D Streptococcus II-Organisms Enterococcus faecalis Enterococcus faecium Gram Positive Rods Corynebacterium Epidemiology Rare in United States due to Immunization (DTP, DTaP) However 20% of adults may be inadequate immune status Ongoing epidemic in the former USSR Etiology Corynebacterium Diphtheriae Corynebacterium Symptoms sore throat dysphagia Weakness Malaise Corynebacterium Signs Toxic appearance fever Tachycardia (out of proportion to fever) Pharyngeal erythema Gray-white tenacious exudate or "membrane" Occurs at tonsillar pillars and posterior pharynx Leaves focal hemorrhagic raw surface when removed Cervical lymphadenopathy Differential Dx Vincent's Angina (trench mouth) Pharyngitis Labs Also shows pseudomembrane formation CBC Leukocytosis Throat culture (+ for corynebacterium org.) Management Diphtheria antitoxin Erythromycin 20-25 mg/kg q12 hours IV for 7-14 days Prevention DTP/DTaP vaccination Listeria monocytogenes Bacillus anthracis (Anthrax) Etiology Transmission Contact with hides of infected animals Cattle Sheep Camels Antelopes Ingestion of contaminated meat Inhalation of spores Bacillus anthracis Infective aerosol dose: 8,000-50,000 spores Spores may remain viable in soil for >40 years No transmission person to person Bacillus anthracis (Anthrax) Symptoms and Signs: Cutaneous ("Malignant Pustule") Inoculation at site of broken skin Painless pruritic pustules develop at inoculation site Begins as erythematous papule on exposed skin Vesiculates and then ulcerates within 1-2 days Surrounded by a ring of non-tender Brawny edema Black eschar may form Bacillus anthracis (Anthrax) Bacillus anthracis (Anthrax) Symptoms and Signs: Inhalation Anthrax Malaise Regional lymphadenopathy Two phases Initial Phase Viral upper respiratory symptoms rhinorrhea pharyngitis Later Phase dyspnea and hemoptysis during dissemination Symptoms and Signs: Acute GI type symptoms Hematemesis Severe diarrhea Differential Diagnosis Cutaneous Anthrax Spider bite Ecthyma gangrenosum Ulceroglandular tularemia Plague Staph. Or strep. cellulitis Inhalational Anthrax Community acquired pneumonia (late phase anthrax) Mycoplasma pneumonia (early phase anthrax) Influenza (early phase anthrax) Legionnaires' Disease Psittacosis tularemia Q fever Viral pneumonia Histoplasmosis Coccidiodomycosis Bacillus anthracis (Anthrax) Labs Rapid ELISA test now available Cultures Gram stain - blood or vesicular fluid from lesion Gram positive bacilli CBC Blood culture (high sensitivity) Cultures of Vomitus or feces (Intestinal Anthrax) CSF culture (Inhalational Anthrax) Nasal Swab (Epidemiologic tool to identify outbreak) Sputum culture (Inhalational Anthrax) Vesicular fluid (Cutaneous Anthrax) Neutrophilic leukocytosis in severe cases Radiology: Chest x-ray - Widened Mediastinum (hemorrhagic mediastinitis Management: Antibiotics Antibiotic course: 60 days Empiric Treatment Cipro Adults: 400 mg IV q12 hours Children: 20-30 mg/kg/day IV divided q12 hours Levofloxacin Adults: 500 mg IV q24 hours Specific Treatment for confirmed anthrax Adults Pencillin G 4 MU IV q4 hours or Doxycycline 200 mg IV, then 100 mg IV q12 hours Children > age 12 same as adults Children < age 12 Penicillin G 50,000 U/kg IV q6 hours Postexposure prophylaxis Concurrently begin vaccination Continue antibiotics for 60 days Ciprofloxacin Amoxicillin Adults: 500 mg PO bid Children: 20-30 mg/kg/day divided bid up to 1g/day Adults: 500 mg PO tid Children: 40 mg/kg up to 500 mg PO tid Doxycycline Adults: 100 mg PO bid Children over age 8: 5 mg/kg/day divided q12 hours Anthrax Course Incubation: 4-6 days Duration of illness: 3-5 days Prognosis Inhalation Anthrax (inhaled spores) Cutaneous Anthrax (skin contact) Untreated: 95% mortality Treated: 80% mortality Untreated: 20% mortality Treated: Rare mortality Intestinal Anthrax (ingested contaminated meat) Prevention Anthrax Vaccine 93% effective Initial: 0, 2, and 4 weeks Next: 6, 12, 18 months and then annually Postexposure Prophylaxis as above Empiric prophylaxis for any suspected exposure Best prognosis with antibiotics prior to symptoms Gram Negative Gram Negative Rods Anaerobes Bacteroidaceae (e.g. Bacteroides fragilis) Facultative Anaerobes (enteric/nonenteric) Enterobacteriaceae (e.g. Escherichia coli) Vibrionaceae (e.g. Vibrio Cholerae) Pasturella,Brucella,Yersinia Aerobes Pseudomonadaceae (e.g. Pseudomonas aeruginosa) Facultative Anaerobes Enterobacteriaceae (e.g. E. coli) Vibrionaceae (e.g. Vibrio Cholerae) Salmonella,Shigella,Klebsiella,Proteus GI pathogens !!!!! non-enteric Pasturella,Brucella,Yersinia Francisella,Hemophilus,Bordetella Enterobacteriaceae Characteristics Facultative Anaerobic Gram negative rods EKP Gram negative bacteria Escherichia coli Klebsiella Proteus Vibrionaceae Characteristics Facultative Anaerobic gram negative rods Vibrio Cholerae Vibrio parahaemolyticus Genus: Aeromonas (motile with single polar flagellum) Vibrionaceae Genus: Campylobacter (motile with single polar flagellum) Campylobacter jejuni Genus: Helicobacter (motile with multiple flagella) Helicobacter Pylori Pasteurellaceae Characteristics Facultative Anaerobic gram negative rods Genus: Pasteurella Pasteurella multocida Pasteurellaceae Genus: Haemophilus (coccobacilli) Haemophilus Influenzae Haemophilus aegyptius Haemophilus ducrei Gram Negative Rod Aerobes Pseudomonadaceae (e.g. Pseudomonas aeruginosa) Brucella Legionellaceae Pseudomonadaceae Characteristics Aerobic Gram Negative Rod Family: Pseudomonadaceae Pseudomonas aeruginosa Pseudomonas mallei (Glanders) Gram Negative Rod Aerobic Family: Legionellaceae Legionella pneumophila Legionellaceae Pathophysiology Aerobic, intracellular, Gram negative rod Virulent organism More severe disease than other atypical pneumonia Transmission Waterborne Transmission Optimal conditions for growth Temperature: 89 to 113 F water Stagnant water Freshwater or moist soil near ponds Air conditioning Condensers Cooling towers Respiratory therapy equipment Showers or water faucets Whirlpools Incubation Two to ten days Legionellaceae Symptoms Prodrome for 12-48 hours Malaise Myalgia HA Symptoms for 2-3 days Fever to 40.5 C persists for 8-10 days GI symptoms- 20-40% of cases Nausea/vomiting Diarrhea Later Symptoms: Cough Minimal to no sputum production Slightly blood tinged sputum Signs Severe respiratory distress Confusion Disorientation Legionella pneumophila Complications Respiratory failure (20-40% of cases) Extrapulmonary complications Myocarditis/pericarditis Prosthetic valve endocarditis Glmoerulonephritis Pancreatitis Peritonitis Legionella pneumophila Radiology: chest x-ray Small pleural effusions Unilateral parenchymal infiltrates Round, fluffy opacities Spread contiguously to other lobes Progresses to dense consolidation Progresses to bilateral infiltrates Legionella pneumophila Labs CBC Erythrocyte Sedimentation Rate leukocytosis leukopenia Elevated markedly LFTs increased Sputum Exam Fluorescent antibody studies of sputum Legionella can not be seen on gram stain Legionella pneumophila Diagnosis Legionella urine antigen testing High sensitivity/ serogroup 1 Sputum Culture - to ID other serogroups Serogroup 1 (LP1) causes most U.S. cases Urine antigen and sputum culture all cases Legionella Serologies Legionella fourfold titer rise to >= 1:128 or Legionella titer >= 1:256 Legionella pneumophila Management (Antibiotic course for 21 days) Azithromycin IV Levofloxacin IV Trovafloxacin IV Erythromycin IV Add Rifampin in immunocompromised or severe disease Course Response to antibiotics may not be seen for 4-5 days Up to 15% mortality in some studies Brucellosis Epidemiology US Incidence <100 cases per year (0.34/100,000) Etiology Brucella abortus Brucella suis Brucella melitensis Brucellosis Pathophysiology Facultative intracellular parasite Releases endotoxin when dies Infective dose: 10-100 organisms Incubation: 5-60 days Brucellosis Transmission Infected animal products Tissue from Sheep in U.S. Unpasteurized milk Vaccine exposure No transmission person to person Enters via mucus membranes, broken skin, or inhalation Brucellosis Risk Factors Veterinarians Farm workers Meat processing plants Travel or residence in endemic region Mediterranean India North Africa, East Africa Central Asia, South Asia Brucellosis Symptoms Intermittent fevers Undulating fever Temperature peaks in evening to 101-104 Arthralgia (90%) Weakness Lassitude Weight loss Headache Sweating Chills Brucellosis Course Weeks to months Prognosis Case Fatality <5% treated Gram Negative Cocci Aerobes Moraxella(Branhamella catarrhalis) Acinetobacter Neisseria Neisseriaceae Neisseria meningitidis Neisseria gonorroeae Neisseria gonorrhoeae Epidemiology Incidence: 500-700,000 cases per year Much less common than chlamydia Decreasing except in inner city, drug abuse (crack) Highly contagious: 50% transmission Chlamydia coexists in 45-50% of patients with gonorrhea Pathophysiology Incubation: 2-7 days Neisseria gonorrhoeae Symptoms and Signs: General Urinary Symptoms Copious urethral discharge Urinary frequency Urinary urgency Dysuria Green, yellow, or sanguinous discharge Meatus and anterior urethra inflammation Neisseria gonorrhoeae Conjunctivitis Direct inoculation Copious exudate Beefy Conjunctiva Serious complications Pharyngitis Corneal ulceration or opacification Visual loss Globe perforation Rarely the only site of infection Usually asymptomatic Acute Diarrhea Neisseria gonorrhoeae Symptoms and Signs: Women Mucopurulent Cervicitis Often asymptomatic Vaginal d/c or spotting Bartholin’s Gland inflammation Skene's gland inflammation Neisseria gonorrhoeae Symptoms and Signs: Men (often asymptomatic) Epidiymitis under age 35 years Proctitis Receptive anal intercourse or vaginal secretions Mild anal irritation or itching Neisseria gonorrhoeae Symptoms and Signs: Disseminated Infection More common in pregnancy Dermatitis Rash over trunk, extremities, palms and soles Necrotic pustule on red base over distal extremity May become hemorrhagic Usually less than 20 total lesions Tenosynovitis Gonococcal arthritis Endocarditis risk Neisseria gonorrhoeae Complications PID Systemic Gonorrhea Chronic Arthritis Neonatal Gonorrhea Gonorrheal conjunctivitis Preterm labor Neisseria gonorrhoeae Labs Gram stain: Urethral /cervical smear Numerous WBCs Gram negative biscuit-shaped diplococci Gonorrhea culture and Sensitivity Antigen Testing (e.g. Gonozyme) False positive Gram stain (saprophytic Neisseria) Indicated in symptomatic men Inaccurate in other populations DNA probe testing Rapid: 30 minutes Sensitivity: 85-100% Specificity: 99-100% Neisseria gonorrhoeae Management: Drug Resistance Tetracycline resistance: 17-23% Penicillin resistance 15-19% Emerging Fluroquinolone resistance No resistance to 3rd generation cephalosporins Ceftriaxone (Rocephin) Cefixime (Suprax) Azithromycin requiring higher dosages for some GC References Moraxella catarrhalis Diagnosis Represents less than 5% of all pneumonias More common in COPD Lobar consolidation is rare Moraxella catarrhalis Labs Gram stain Kidney bean shaped gram negative diplococci Radiology Chest xray patchy bronchopulmonary infiltrate Moraxella catarrhalis Management: Antibiotic Amoxicillin-clavulanate (Augmentin) Second generation Cephalosporin (e.g. Cefuroxime) 3rd generation Cephalosporin (e.g. Cefotaxime) Erythromycin Azithromycin (Zithromax) Clarithromycin (Biaxin) Trimethoprim Sulfamethoxazole (Bactrim or Septra) Doxycycline Gram Negative Obligate Intracellular Parasites Rickettsia Ehrlichia Coxiella Rochalimaea (not obligate intracellular) Rickettsia Genus: Rickettsia Typhus Group Spotted Fever Group Rickettsia prowazekii (epidemic typhus,louse) Rickettsia mooseri Rickettsia rickettsii (rmsf,tick) Scrub Typhus Group Rickettsia tsutsugamushi (scrub typhus,) Rickettsia rickettsii Pathophysiology Transmission: Tick bite Infects blood vessel walls Endothelial cells Smooth muscle cells Rickettsia rickettsii is causative organism Small pleomorphic organism Obligate intracellular parasite Rocky Mountain Spotted Fever Epidemiology Bimodal age distribution Ages 5 to 9 years old Age over 60 years old Endemic area North America Atlantic coast states Midwest Central America South America Rocky Mountain Spotted Fever Symptoms (follows seven day incubation) Fever HA Myalgias Malaise vomiting Rocky Mountain Spotted Fever Signs: Rash (occurs in 90% of patients) Onset in first week of illness Characteristics Distribution Initial: Blanching Macules 1 to 4 mm in diameter Later: Macules transition to Petechiae Onset: Wrists and Ankles Later: Trunk, Palms and Soles Labs Rocky Mountain Spotted Fever Labs CBC Liver transaminases increased AST /ALT Serum sodium -Hyponatremia Cerebrospinal Fluid WBC normal or slightly decreased Thrombocytopenia CSF pleocytosis w/monocytic predominance Rickettsia Serology Positive 7 to 10 days after symptom onset Used for confirmation, not for diagnosis Rocky Mountain Spotted Fever Management Antibiotic Course Minimum course: 5 to 7 days Continue antibiotics until afebrile for 2 days Antibiotics Doxycycline or Tetracycline or Chloramphenicol Rocky Mountain Spotted Fever Complications Encephalitis Noncardiac pulmonary edema ARDS Cardiac arrhythmia Coagulopathy GI bleeding Skin Necrosis Rocky Mountain Spotted Fever Prognosis Untreated: 25% Mortality within 8 to 15 days Treated: 5% Mortality Ehrlichia Ehrlichia sennetsu Ehrlichia canis Coxiella Coxiella burnetii – Q fever, no arthropod vector cattle,sheep, goats, inhallation of dust with dried feces urine or milk Rochalimaea (not obligate intracellular) Rochalimaea quintana (trench fever seen in military settings) Chlamydia Eye Diseases Trachoma Inclusion conjunctivitis Genitourinary Disease Lymphogranulmoa venereum Urethritis cervicitis Salpingitis Respiratory Other Chlamydia psittaci (Human psittacosis) Chlamydia pneumonia in newborns Bird borne zoonosis Respiratory illness or typhoidal illness Chlamydia pneumoniae pneumonia Chlamydia trachomatis Epidemiology: Very Prevalent Asymptomatic teenage female test positive: 5-10% Sexually active persons: 10% Chlamydia 6 to 10 times more common than Gonorrhea Incidence: 3-5 million cases/year Chlamydia Trachomatis (obligate intracellular organism) Cause Complications Chlamydia Trachomatis (obligate intracellular organism) PID Infertility Preterm labor Perinatal transmission to newborn Chlamydia conjunctivitis Neonatal pneumonia Chlamydia Trachomatis (obligate intracellular organism) Symptoms: Women Vaginal d/c dysuria Pelvic pain Untreated infections may persist for months Usually asymptomatic Urethritis Dysuria-Sterile pyuria Syndrome Persistent dysuria and pyuria Negative urine culture Chlamydia Trachomatis (obligate intracellular organism) Symptoms: Men Urethritis Often symptomatic Associated Conditions: Reiter’s Syndrome in Men Arthritis Conjunctivitis Urethritis Chlamydia Trachomatis (obligate intracellular organism) Management First Choice Refer all sexual contacts for treatment Azithromycin 1 gram PO for 1 dose Doxycycline 100 mg PO bid for 7 days Alternatives Ofloxacin 300 mg PO bid for 7 days Erythromycin 500 mg PO qid for 7 days Erythromycin Ethylsuccinate (EES) Dose: 800 mg PO qid for 7 days Amoxicillin 500 mg PO tid for 7 days Clindamycin 450 mg PO qid for 14 days Chlamydia Trachomatis (obligate intracellular organism) Pregnancy Azithromycin 1 gram PO as single dose Erythromycin OR EES as above for 7 days Amoxicillin 500 PO tid x7 days (Only 50% effective) Neonates (conjunctivitis or pneumonia) Erythromycin for 14 days Questions ??????