Tracheostomy, Lung Cancer, Pneumonia
advertisement

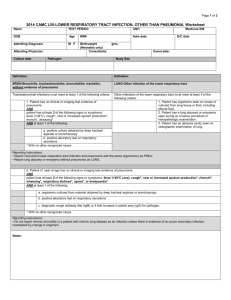
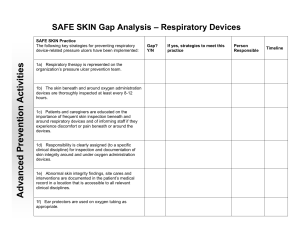
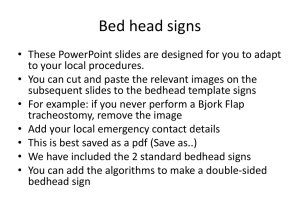
Respiratory System, Tracheostomy, Lung Cancer, Pneumonia, Tuberculosis (TB) Zoya Minasyan RN, MSN-Edu Structures and Functions of Respiratory System Fig. 26-1. Structures of the respiratory tract. A, Pulmonary functional unit. B, Ciliated mucous membrane. Structures and Functions of Respiratory System Fig. 26-5. A small portion of the respiratory membrane greatly magnified. An extremely thin interstitial layer of tissue separates the endothelial cell and basement membrane on the capillary side from the epithelial cell and surfactant layer on the alveolar side of the respiratory membrane. The total thickness of the respiratory membrane is less than 1⁄5000 of an inch. Structures and Functions of Respiratory System Physiology of Respiration Ventilation Compliance Diffusion Oxygen-hemoglobin dissociation curve Mixed venous blood gases Oximetry Structures and Functions of Respiratory System Arterial blood gases Table 26-1. Normal Arterial and Venous Blood Gas Values *. Structures and Functions of Respiratory System Table 26-3. Critical Values for Pao2 and Spo2 *. Structures and Functions of Respiratory System Control of Respiration Chemoreceptors Mechanical receptors Assessment of Respiratory System Assessment of Respiratory System Fig. 26-8. Sequence for examination of the chest. A, Anterior sequence. B, Lateral sequence. C, Posterior sequence. For palpation, place the palms of the hands in the position designated as “1” on the right and left sides of the chest. Compare the intensity of vibrations. Continue for all positions in each sequence. For percussion, tap the chest at each designated position, moving downward from side to side. Compare percussion sounds at all positions. For auscultation, place the stethoscope at each position and listen to at least one complete inspiratory and expiratory cycle. Keep in mind that, with a female patient, the breast tissue will modify the completeness of the anterior examination. Assessment of Respiratory System Fig. 26-9. Diagram of percussion areas and sounds in the anterior side of the chest. Assessment of Respiratory System Fig. 26-10. Diagram of percussion areas and sounds in the posterior side of the chest. Percussion proceeds from the lung apices to the lung bases, comparing sounds in opposite areas of the chest. Assessment of Respiratory System Fig. 26-11. Normal auscultatory sounds. Assessment of Respiratory System Table 26-8. Normal Physical Assessment of the Respiratory System. Diagnostic Studies of Respiratory System Sputum Studies Skin Tests Endoscopic Examinations Bronchoscopy Diagnostic Studies of Respiratory System Fig. 26-12. Fiberoptic bronchoscope. A, The transbronchoscopic balloon-tipped catheter and the flexible fiberoptic bronchoscope. B, The catheter is introduced into a small airway and the balloon inflated with 1.5 to 2 mL of air to occlude the airway. Bronchoalveolar lavage is performed by injecting and withdrawing 30-mL aliquots of sterile saline solution, gently aspirating after each instillation. Specimens are sent to the laboratory for analysis. Sinusitis Head and Neck Cancer Tracheostomy • • • Definition: • Surgical incision into the trachea to establish an airway • Stoma that results from tracheotomy Indications – Bypass upper airway obstruction – Facilitate removal of secretions – Long-term mechanical ventilation – Permit oral intake and speech in patient who requires long-term mechanical ventilation Advantages – Less risk of long-term damage to airway – Increased comfort – Patient can eat. – Increased mobility because tube is more secure Parts of a Tracheostomy Tube Types of tracheostomy tubes. A, Parts of a tracheostomy tube. B, Tracheostomy tube inserted in airway with inflated cuff. C, Fenestrated tracheostomy tube with cuff, inner cannula, decannulation plug, and pilot balloon. D, Tracheostomy tube with foam cuff and obturator (one cuff is deflated on tracheostomy tube). Tracheostomy Care • Explain purpose before procedure. • Inform patient and family of inability to speak while inflated cuff is used. • During insertion, obturator is placed inside outer cannula, with rounded tip protruding from end to ease insertion. • After insertion, obturator must be immediately removed to allow airflow. – Keep obturator near bedside in case of decannulation. – Suctioning the airway to remove secretions – Cleaning around stoma – Changing ties – Providing inner cannula care • Some tubes have a removable inner cannula for easier cleaning. Suctioning Tracheostomy Suctioning tracheostomy with closed system suction catheter. Tracheostomy Care • Tube with inflated cuff is used for risk of aspiration or in mechanical ventilation. – Inflate cuff with minimum volume required to create an airway seal. – Inflate cuff with air to form seal. • Excessive cuff pressure can – Compress tracheal capillaries – Limit blood flow – Predispose to tracheal necrosis Tracheostomy Care • Deflation – To remove secretions accumulating above the cuff – Patient should cough up secretions before deflation to avoid aspiration. – Suction mouth and tube. – Patient should cough and be suctioned again. – Assess patient’s ability to protect airway from aspiration. – Remain with patient when cuff is initially deflated, unless patient can protect against aspiration and breathe without respiratory distress. Tracheostomy Care • Tube of equal or smaller size kept at bedside for emergency reinsertion • Accidental dislodging – Immediately replace tube. – Insert obturator into replacement tube. – If insertion is successful, obturator is removed immediately for airflow through the tube. • If tube cannot be replaced – Assess level of respiratory distress – Severe distress may progress to respiratory arrest – Cover stoma with sterile dressing and ventilate with bag-mask until help arrives – The nurse should take care not to dislodge the tracheostomy tube during the first 5 to 7 days when the stoma is not mature (healed). Tracheostomy Care • Initially should receive humidified air. • Tube should be changed monthly. • Patient can be taught to change tube using clean technique at home. • When a tracheostomy has been in place for several months, the healed tract will be well formed. Changing Tracheostomy Tube at Home When a tracheostomy has been in place for several months, the tract will be well formed. The patient can then be taught to change the tube using a clean technique at home. Swallowing Dysfunction • Inflated cuff – Interferes with normal function of muscles used to swallow – Evaluate risk of aspiration when cuff deflated • Techniques to promote speech – Spontaneously breathing patient may deflate cuff, allowing exhaled air to flow over vocal cords. Speaking Tracheostomy Tubes A, Fenestrated tracheostomy tube with cuff deflated, inner cannula removed, and tracheostomy tube capped to allow air to pass over the vocal cords. B, Speaking tracheostomy tube. One tube is used for cuff inflation. The second tube is connected to a source of compressed air or oxygen. When the port on the second tube is occluded, air flows up over the vocal cords, allowing speech with an inflated cuff. Speech • Tracheostomy tubes and valves have been designed to facilitate speech. • Fenestrated tube has opening on surface of outer cannula to permit airflow over vocal cords to allow – Spontaneous breathing through larynx – Speech – Secretion expectoration with tube in place • Fenestrated tube – Requires frequent suctioning – Ability to swallow is determined before use. – Frequently assess for signs of respiratory distress on first use. Passy-Muir Speaking Tracheostomy Valve The valve is placed over the hub of the tracheostomy tube after the cuff is deflated. Multiple options are available and can be used for ventilated and nonventilated patients. The valve contains a one-way valve that allows air to enter the lungs during inspiration and redirects air upward over the vocal cords into the mouth during expiration. Lung Cancer • • • Most important risk factor in 80% to 90% of all lung cancers is smoking. – Contains 60 carcinogens that interfere with cell development • Total number of cigarettes smoked • Age of smoking onset • Depth of inhalation • Tar and nicotine content • Use of unfiltered cigarettes Causes a change in bronchial epithelium Other carcinogens pose risk for developing lung cancer. – Polycyclic aromatic hydrocarbons – Arsenic – Air pollution Etiology • Environmental tobacco smoke (ETS) inhaled by nonsmokers poses 35% increased risk of developing lung cancer. • Children are more vulnerable to ETS than adults. Lung Cancer Lung cancer (peripheral adenocarcinoma). The tumor shows prominent black pigmentation, scar. Lung Carcinoma The gray-white tumor tissue is infiltrating the lung. Histologically this tumor was identified as a squamous cell carcinoma. Pathophysiology • • Lung cancers metastasize by – Direct extension – Blood circulation – Lymph system Common sites for metastatic growth – Liver – Brain – Bones – Scalene lymph nodes – Adrenal glands Clinical Manifestations • • • • • • Pneumonitis Persistent cough with sputum (most common) Hemoptysis Chest pain Dyspnea Later manifestations – Anorexia – Fatigue – Nausea/vomiting – Hoarse voice – Unilateral paralysis of diaphragm – Dysphagia – Superior vena cava obstruction Diagnostic Studies • • • • Chest x-ray CT scan Magnetic resonance imaging (MRI) Diagnosis identified by malignant cells Diagnostic Studies • Sputum specimens obtained for cytologic studies – Fiberoptic bronchoscope – Video-assisted thoracoscopy (VATS) – Pulmonary angiography • Chemotherapy • Radiation therapy – Used as curative therapy, palliative therapy, or adjuvant therapy – Primary therapy for those unable to tolerate surgery – Some cancer cells are more radiosensitive than others. – Stereotactic radiotherapy Nursing Management Nursing Diagnoses • • • • Ineffective airway clearance Anxiety Acute pain Imbalanced nutrition: Less than body requirements • Ineffective health maintenance • Ineffective breathing pattern Nursing Management: Nursing Implementation • • • Health promotion – Avoid smoking. – Promote smoking cessation programs. – Support education and smoking policies. Acute intervention – Offer support during diagnostic evaluation. – Monitor for side effects. – Provide comfort. – Teach methods to reduce pain. Educate indications for hospitalization. Ambulatory and home care – Follow up carefully for manifestations of metastasis. – Educate patient on signs and symptoms of hemoptysis, dysphagia, chest pain, and hoarseness. – May need information about hospice – http://www.cdc.gov/tobacco/quit_smoking/cessation /index.htm Pneumonia • Acute inflammation of lung caused by microbial organism • Discovery of sulfa drugs and penicillin decreased morbidity and mortality rates. • Likely to result when defense mechanisms become overwhelmed • ↓ Cough and epiglottal reflexes may allow aspiration • Mucociliary mechanism impaired by – Pollution – Cigarette smoking – Upper respiratory infections – Tracheal intubation – Aging Etiology • Three ways organisms reach lungs: – Aspiration from nasopharynx or oropharynx – Inhalation of microbes such as Mycoplasma pneumoniae – Hematogenous spread from primary infection elsewhere in body Types of Pneumonia • Community-acquired pneumonia – Lower respiratory infection of lung – Onset in community or during first 2 days of hospitalization – Highest incidence in midwinter – Smoking- important risk factor Types of Pneumonia • Organisms implicated – Streptococcus pneumoniae – Haemophilus influenzae – Legionella – Mycoplasma – Chlamydia Types of Pneumonia • HAP: Hospital-acquired pneumonia. • VAP: Ventilator-associated pneumonia. • HCAP: Health care–associated pneumonia: newonset pneumonia in a patient who • was hospitalized in an acute care hospital for ≥2 days within 90 days of the infection; • resided in a long-term care facility; • received recent intravenous antibiotic therapy, chemotherapy, or wound care within the past 30 days of the current infection; or • attended a hospital or hemodialysis clinic. Types of Pneumonia • Risk factors for HAP – Immunosuppressive therapy – General debility – Endotracheal intubation • Treatment is based on – Known risk factors – Severity of illness Types of Pneumonia • Aspiration pneumonia – Occurring from abnormal entry of secretions into lower airway – Usually with history of loss of consciousness • Gag and cough reflexes suppressed – Forms of aspiration pneumonia • Mechanical obstruction • Chemical injury • Bacterial infection Types of Pneumonia • Opportunistic pneumonia – Patients at risk • Severe protein-calorie malnutrition • Immune deficiencies • Chemotherapy/radiation recipients • Long-term corticosteroid therapy • Causes of opportunistic pneumonia – Bacterial and viral causative agents – Pneumocystis jiroveci (PCP) – Cytomegalovirus – Fungi Types of Pneumonia • Clinical manifestations of PCP (Pneumocystis jiroveci) – Fever – Tachypnea – Tachycardia – Dyspnea – Nonproductive cough – Hypoxemia Pathophysiology • • • Stage 1: Congestion from outpouring of fluid to alveoli – Organisms multiply. – Infection spreads. – Interferes with lung function Stage 2: – Red hepatization • Massive dilation of capillaries • Alveoli fill with organisms, neutrophils, RBCs, and fibrin. • Causes lungs to appear red and granular, similar to liver – Gray hepatization – ↓ Blood flow – Leukocyte and fibrin consolidate in affected part of lung. Resolution – Resolution and healing if no complications – Exudate lysed and processed by macrophages – Tissue restored Pathophysiologic Course of Pneumococcal Pneumonia Clinical Manifestations • CAP symptoms(care associated Pneumonia) – Sudden onset of fever – Shaking chills – Shortness of breath – Cough productive of purulent sputum – Pleuritic chest pain Clinical Manifestations • Physical examination findings – Dullness to percussion – ↑ Fremitusa (vibration or tremor, resulting from a physical action such as speaking or coughing, felt by hand and used to assess whether the chest is affected by disease) – Bronchial breath sounds – Crackles – Related to infection with S. pneumoniae and H. influenzae. • Initial manifestations are highly variable in viral pneumonia. – Primary pneumonia can be caused by influenza viral infection. – Can be a complication of systemic viral disease Complications • Pleurisy (inflammation of the membrane pleura surrounding the lungs, usually involving painful breathing, coughing, and the buildup of fluid in the pleural cavity) • Pleural effusion (a thin transparent membrane that lines the chest wall and doubles back to cover the lungs, thereby forming a continuous sac enclosing the narrow pleural cavity. The inner faces of the cavity are lubricated by fluid to ease breathing) movements. • Usually is sterile and reabsorbed in 1 to 2 weeks or requires a thoracentesis (surgical procedure in which a needle is inserted through the chest wall in order to withdraw fluid, blood, or air) • Atelectasis – Usually clears with cough and deep breathing • Bacteremia – Bacterial infection in the blood Complications • Lung abscess – Seen when caused by S. aureus and gram-negative pneumonias • Pericarditis – Spread of microorganism to heart • Meningitis – Patient who is disoriented, confused, or somnolent should have lumbar puncture. • Endocarditis – Microorganisms attack endocardium and heart valves. Diagnostic Tests • • • • • • • • History Physical examination Chest x-ray Gram stain of sputum Sputum culture and sensitivity Pulse oximetry or ABGs CBC, differential, chemistries Blood cultures Collaborative Care • • • • • • • Antibiotic therapy Oxygen for hypoxemia Analgesics for chest pain Antipyretics Fluid intake at least 3 L per day Caloric intake at least 1500 per day, IV Pneumococcal vaccine – Indicated for those at risk • Chronic illness such as heart and lung disease, diabetes mellitus • Recovering from severe illness • 65 or older • In long-term care facility Nursing Assessment • History – Lung cancer – COPD – Diabetes mellitus – Debilitating disease – Malnutrition – AIDS – Use of antibiotics, corticosteroids, chemotherapy, immunosuppressants – Recent abdominal or thoracic surgery – Smoking – Alcoholism – Respiratory infections – Prolonged bed rest – Dyspnea – Nasal congestion – Pain with breathing – Sore throat • Muscle ache • • • • • • • • • • • • • Fever Restlessness Tachypnea Asymmetric chest movements Use of accessory muscles Crackles Green or yellow sputum Tachycardia Changes in mental status Leukocytosis Abnormal ABGs Pleural effusion Pneumothorax on x-ray Nursing Diagnoses • • • • Ineffective breathing pattern Ineffective airway clearance Acute pain Imbalanced nutrition: Less than body requirements • Activity intolerance Planning • • • • • Clear breath sounds Normal breathing patterns No signs of hypoxia Normal chest x-ray No complications related to pneumonia Nursing Implementation • Teach nutrition, hygiene, rest, regular exercise to maintain natural resistance. • Prompt treatment of URIs • Strict asepsis • Encourage those at risk to obtain influenza and pneumococcal vaccinations. • Reposition patient every 2 hours. • Elevate head of bed 30 to 45 degrees for patients with feeding tube. • Assist patients at risk for aspiration with eating, drinking, and taking medications. • Assist immobile patients with turning and deep breathing. • Emphasize need to take course of medication(s). • Teach drug–drug interactions. Evaluation • • • • • • • • Dyspnea not present SpO2 ≥ 95 Free of adventitious breath sounds Clear sputum from airway Reports pain control Verbalizes causal factors Adequate fluid and caloric intake Performs activities of daily living Tuberculosis (TB) • Infectious disease caused by Mycobacterium tuberculosis TB Involves • • • • Lungs Larynx Kidneys Meninges Bones Adrenal glands Lymph nodes Etiology and Pathophysiology • Spread via airborne droplets when infected person – Coughs – Speaks – Sneezes – Sings – Transmission requires close, frequent, or prolonged exposure. Etiology and Pathophysiology • Spread – Inhaled bacilli pass down bronchial system and implant themselves on bronchioles or alveoli. – Multiply with no initial resistance – Replicates slowly and spreads via the lymphatic system • If cellular immune system is activated – Tissue granuloma forms – The bacteria are contained, preventing replication and spread of disease Etiology and Pathophysiology • Favorable environments for growth: – Upper lobes of lungs – Kidneys – Epiphyses of bone – Cerebral cortex – Adrenal glands Clinical Manifestations Fatigue Malaise Anorexia Weight loss Low-grade fevers Night sweat Clinical Manifestations • Cough becomes frequent. – Hemoptysis is not common and is usually associated with advanced disease. – Acute symptoms (generalized flu symptoms) • High fever • Chills • Pleuritic pain • Productive cough Complications • Miliary TB – Large numbers of organisms invade the bloodstream and spread to all organs. • Acute or chronic symptoms • Pleural effusion – Caused by bacteria in pleural space – Inflammatory reaction with plural exudates of protein-rich fluid • TB pneumonia – Large amounts of bacilli discharging from granulomas into lung or lymph nodes • Other organ involvement – CNS—Meninges – Bone and joint tissue – Kidneys Diagnostic Studies • Skin testing – Intradermal administration of tuberculin • Induration at injection site indicates exposure. • Sensitivity remains for life, and individual should not be tested again. – Response ↓ in immune compromised patients • Reactions ≥5 mm considered positive • Two-step testing recommended for health care workers getting repeated testing and those with decreased response to allergens. Skin testing • The test is administered by injecting 0.1 mL of PPD (Purified protein derivative) intradermally on the dorsal surface of the forearm. • The test is read by inspection and palpation 48 to 72 hours later for the presence or absence of induration. • The indurated area (if present) is measured and recorded in millimeters with 0 for no induration. • The reaction occurs 2 to 12 weeks after initial exposure to the organisms. Diagnostic Studies • Chest x-ray – Cannot make diagnosis solely on x-ray – Upper lobe infiltrates, cavitary infiltrates, and lymph node involvement suggest TB. • Bacteriologic studies – Stained sputum smears examined for acid-fast bacilli – Required for diagnosis – On different days, three consecutive sputum samples – Could also be collected from • Gastric washings • CSF • Fluid from an abscess or effusion Diagnostic Studies • QuantiFERON-TB (QFT) – Rapid blood test (few hours) – Does not replace cultures Sputum Cultures – On different days, three consecutive sputum samples – Could also be collected from » Gastric washings » CSF » Fluid from an abscess or effusion Collaborative Care • Hospitalization not necessary for most patients • Drug therapy used to prevent or treat active disease Drug Therapy • Active disease – Four drugs are used in initial phase for maximum effectiveness. • Treatment is aggressive to combat resistant strains of TB. •In most circumstances, the treatment regimen for patients with previously untreated TB consists of a 2-month initial phase with four-drug therapy (INH isonicotinylhydrazine, rifampin [Rifadin], pyrazinamide [PZA], and ethambutol). •If drug susceptibility test results indicate that bacteria are susceptible to all drugs, ethambutol may be discontinued. Drug Therapy • Directly observed therapy (DOT) – Noncompliance is major factor in multidrug resistance and treatment failures. – Requires watching patient swallow drugs Drug Therapy • Active disease – Patients should be taught about side effects and when to seek medical attention. – Liver function should be monitored. • Latent TB infection – Usually treated with INH for 6 to 9 months – HIV patients should take INH for 9 months. • Vaccine – Bacille Calmette-Guérin (BCG) vaccine to prevent TB is currently in use in many parts of the world. – In United States, not recommended – Can result in positive PPD (Purified protein derivative) reaction Nursing Assessment • Assess for – Productive cough – Night sweats – Afternoon temperature elevation – Weight loss – Pleuritic chest pain – Crackles over apices of lungs Nursing Diagnoses • Ineffective breathing pattern • Imbalanced nutrition: Less than body requirements • Noncompliance • Ineffective health maintenance • Activity intolerance Planning • Goals – Comply with therapeutic regimen. – Have no recurrence of disease. – Have normal pulmonary function. – Take appropriate measures to prevent spread of disease. Nursing Implementation Selective screening programs in high-risk groups to detect TB Identify contacts of patient with TB. • Acute intervention – Airborne isolation – Appropriate drug therapy – Immediate medical workup Nursing Implementation • Teach patient – Cover nose and mouth with tissue when coughing, sneezing, or producing sputum – Hand washing after handling sputum-soiled tissues • Ambulatory and home care – Ensure that patient can adhere to treatment. – Teach symptoms of recurrence. Evaluation • Expected outcomes – Complete resolution of disease – Normal pulmonary function – Absence of any complications – No transmission of TB