Chemoprevention of Cancer
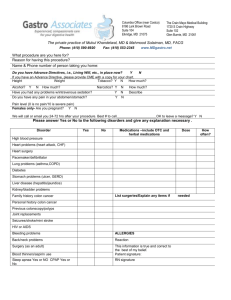
advertisement

Colon Cancer Chemoprevention UWCCC Chemoprevention Program And Mayo Clinic Chemoprevention Program Spirit of Eagles September 6, 2007 Howard Bailey, MD and Paul Limburg, MD, MPH Colon Cancer Chemoprevention Need/Rationale 150,000 expected to be diagnosed with colorectal cancer in 2007 >50,000 expected to die from colorectal cancer in 2007 Estimated new Cancer Cases for 2007 Jemal et al. CA Cancer J Clin 2007 Estimated Cancer Deaths for 2007 Jemal et al. CA Cancer J Clin 2007 Annual Age-adjusted Cancer Incidence Rates Jemal et al. CA Cancer J Clin 2007 Annual Age-adjusted Death Rate Males Jemal et al. CA Cancer J Clin 2007 Annual Age-adjusted Death Rate Females Jemal et al. CA Cancer J Clin 2007 Incidence of Selected Cancers by Race/Ethnicity Jemal et al. CA Cancer J Clin 2007 Death Rates for Cancers by Race/Ethnicity Jemal et al. CA Cancer J Clin 2007 Colo-rectal Cancer Incidence JNCI Stat Bite, 2006 Colon Cancer • Above data implies while colorectal cancer remains a significant health issue, it appears to be lessening including for American Indians/Alaska Natives. • Cancer mortality, in general, is less in American Indians/Alaska Natives than general population 165 compared to 201 per 100,000; however mortality rates for Alaska Natives and Northern Plains Tribes is higher, especially for colorectal, lung, liver, stomach, gall bladder and kidney cancers. Mortality Rates Selected IHS sites Slattery, J Cancer Educ 2005 Colon Cancer in Indian Country • Harwell et al. (Am J Prev Med 30:493, 2006) – Age adjusted 6-yr cancer incidence rates in Montana, 1991-96 and 1997-2002 – All cancers incidence rates higher in American Indians than whites – Colon cancer incidence twice as high in American Indian males as white males Colon Cancer Prevention • For the US population it remains important despite decreasing incidence and mortality • This appears especially true for Northern Plains Tribes and Alaska Natives • Many ways to accomplish this through lifestyle, screening, etc.. • Will focus on the potential of chemoprevention of colon cancer Chemoprevention of Cancer The study of carcinogenesis has led to the current dogma that human carcinogenesis is a multi-year process Example – normal colonic mucosa to hyperplastic polyps to adenomatous polyps to carcinoma may take 10-30 years Thus providing an opportunity to intervene prior to accumulated mutations or phenotypic changes Candidate Agents • COX-2 inhibitors, selective or nonselective • Diet and Nutraceuticals • Antioxidants/Vitamins • Statins • Difluoromethylornithine (DFMO) • Others Selective COX-2 Inhibitors • Celecoxib: FDA approved for adenomatous polyp prevention for individuals with Familial Adenomatous Polyposis – These data and retrospective data have led to extensive study of COX-2 inhibitors for sporadic adenomas as well Selective COX-2 Inhibitors FAP Trial (phase IIb) • Phenotypic expression of APC mutation (n=81) • 3 arms; duration = 6 mo. - celecoxib 100 mg bid - celecoxib 400 mg bid placebo bid • Change in polyp burden Steinbach, et al. - N Engl J Med 2000;342:1946-52; Images from E. Hawk, NCI Subject #5120 41 Polyps at Baseline Images courtesy of Dr. E. Hawk, NCI 21 Polyps at Follow-Up Change in Polyp Number % Change from Baseline 80 60 40 20 0 -20 - 4.5 - 11.9 -28.0%* -40 -60 -80 Placebo 100 mg BID 400 mg BID (N=30) (N=15) (N=32) * p< 0.05; Steinbach, et al. - N Engl J Med 2000;342:1946-52 Sporadic Adenomas Phase III Trials APC Trial • Sporadic CRN (n=2,035) • 91 participating sites • Celecoxib 200 mg bid or 400 mg bid vs. placebo • Rec. adenomas at 3 years AdvancedAdenomas Adenomas Recurrent Placebo bid *p<0.0001 vs. placebo; Bertagnolli – NEJM 2006;355:873-84 Celecoxib200 mg bid Celecoxib400 mg bid Phase III Trials PreSAP Trial (n=1,561) • 107 participating sites • Celecoxib 400 mg qd vs. placebo • Rec. adenomas at 3 years RR=0.64 (0.56-0.75); any RR=0.49 (0.33-0.73); adv. APPROVe Trial (n=2,587) • 108 participating sites • Rofecoxib 25 mg qd vs. placebo • Rec. adenomas at 3 years RR=0.76 (0.69-0.83); any RR=0.70 (0.57-0.73); N Engl J Med 2006;355:885-95 and Gastroenterol 2006; epub adv. Cardiovascular Toxicity Celecoxib • APC Trial • N=2,035 subjects • Follow-up = 2.8-3.1 years • CV deaths (%): Rofecoxib • APPROVe Trial • N=2,586 subjects • Follow-up = 3,327 pt-years • CV Adverse events (%): –Placebo (1%); RR=1.0 –200 mg BID (2.3%); RR=2.3 –400 mg BID (3.4%); RR=3.4 www.theoaklandpress.com; www.washingtonpost.com; 4/7/05 12/18/04 N Engl J Med. 2005;352:1071-80 and 1092-102 –Placebo (2%); RR=1.0 –25 mg QD (3.6%); RR=1.9 Celecoxib and Colon Cancer Prevention • Psaty and Potter (NEJM 355:950, 2006) – Reviewed APC and PreSAP trials and concluded the following – Celecoxib decreases adenoma formation – Celecoxib increases the risk of cardiovascular adverse events – The potential increase in CV event/mortality outweighs the projected decrease in colon cancer incidence Non-selective COX-2 inhibitors • Retrospective data supporting potential preventive effects • Cardiovascular issues appear less, but remain • Aspirin Sandler et al. NEJM 348:883, 2003 635 subjects with previous colo-rectal CA randomized to ASA 325 mg/d or placebo 1 or more adenomas in 27% of placebo vs 17% ASA Calcium Polyp Prevention Study Extended Follow-Up • Self-reported surveys (n=822) • Mean = 7 yrs postintervention • Histologic confirmation for adenomas • 37% lower risk < 5 yrs Grau, et al. – J Natl Cancer Inst 2007;99:129-36 Calcium + Vitamin D Women’s Health Initiative • Postmenopausal women (n=36,282) • 1000 mg elemental calcium + 400 IU vit. D3 vs. placebo • Mean duration = 7.0 yrs • Incident CRC (sec. endpoint) • HR=1.1; 95% CI=0.9-1.3 0.010 0.006 0.002 0.000 0 1 2 3 4 5 6 7 8 = calcium + vitamin D = placebo Wactawski-Wende, et al. – N Engl J Med 2006;354:684-96 Nutraceutical Trials Agent(s) N Fiber, Fat 201 Fiber, Fat, BC* 424 Fiber 1,429 Fiber, Fat, F&V† 2,079 Vitamins C, E 200 Vitamins C, E 864 Vitamin E 29,133 Selenium 598 Antioxidants + Calcium 93 Calcium 930 *Beta carotene; †Fruits & vegetables Endpoint Risk Estimate Rec. adenoma 1.2 (0.6-2.2) Rec. adenoma 1.2 (0.8-2.0) Rec. adenoma 0.9 (0.7-1.1) Rec. adenoma 1.0 (0.9-1.1) Rec. adenoma 0.9 (0.5-1.5) Rec. adenoma 1.1 (0.9-1.3) Inc. cancer 0.8 (0.6-1.1) Prev. adenoma 0.7 (0.4-1.1) Rec. adenoma 0.3 (0.1-0.8) Rec. adenoma 0.8 (0.7-1.0) Meta-analysis of Antioxidants for GI Cancer Prevention Bjelakovic et al. Lancet 364:1219, 2004 Meta-analysis of Antioxidants for GI Cancer Prevention Overall Mortality Bjelakovic et al. Lancet 364:1219, 2004 Statins and Colon Cancer • Lipid lowering agents have been associated with decreased incidence of various cancers • Dale et al (JAMA 295:74, 2006) performed metaanalysis of randomized through 2005 and observed no effect on cancer incidence or death rate • Poynter et al. (NEJM 352:2184, 2005) case control study in Israel of approx 2000 colon cancer patients vs 2000 controls; statin use of >5 yrs was associated with a 50% risk reduction Difluoromethylornithine (DFMO) • DFMO is a specific polyamine inhibitor approved for treatment of African Sleeping sickness • Phase 2 and 3 studies in other tissue sites have observed safety and tolerability; longer duration studies are pending including in preventing colonic polyps Chemoprevention of Colon Cancer • Promising results with COX-2 inhibitors have been severely compromised by other organ toxicity • Dietary measures or nutrient-based supplements have mainly been negative, potential exceptions include calcium ± vitamin D and selenium • We continue to explore other options for the chemoprevention of colon cancer Chemoprevention of Colon Cancer • Future directions – Earlier markers of risk • Protein signatures • Aberrant crypt formation within colon • Genomic signatures – Less invasive measures of ongoing chemopreventive effectiveness • Finding the equivalent of checking your cholesterol level for risk of heart disease Chemoprevention of Colon Cancer • Future directions cont. – Combinations; low dose non-selective COX-2 inhibitors + other agents • DFMO + sulindac • Green tea + non-selective COX-2 – Test interventions as more health maintenance rather than just trying to prevent a specific cancer • Studies like the Women’s Health Initiative Colon Cancer Prevention • Currently there are more established/costeffective measures to reduce the burden of colo-rectal cancer; • Chemoprevention of colon cancer currently is not an established approach. • For many reasons pursuing non-invasive interventions for colon cancer risk reduction is important. Examples by Target Organ Kelloff, et al. - Cancer Epidemiol Biomarkers & Prev 2000;9:127-37 Clinical Trials Phase II Trial(s) 25-75 50-300 1-12 6-36 pK, dose, SEB mod. safety Phase III Trials 300+ 36-60 cancer inc. Cost Subjects (N) Duration (months) Primary Endpoints Phase I Trial Risk Candidate Agent Chemoprevention Targets General • Proliferation • Apoptosis • Circulating growth factors • Immunosurveillance • Metastasis Specific • Tumor necrosis factor • Nuclear factor-kappa B • Activator protein-1 • STAT proteins • Cyclooxygenase-2 • Lipoxygenases Colorectal Cancer Potential Cohorts • Prior neoplasia • Inflamm. bowel disease Case Distribution 75% - Crohn’s disease - ulcerative colitis • FAP • HNPCC • Family hx. NOS 4% Sporadic Familial NOS HNPCC 15% FAP Other Syndromes IBD Chemoprevention Agents/Issues with Micronutrients CARET, ATBC, and NPC Results Concerning negative results Micronutrients assumed not to be harmful Replacement doses vs supraphysiologic (prooxidant effects?) Regular dietary consumption vs supplementation Smokers and gender differences in metabolism