Hormonal Control of Urine Production
advertisement

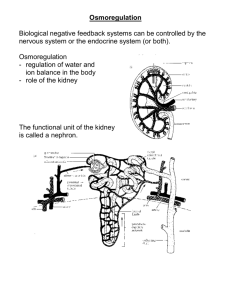
Hormonal Control of Urine Production Long- Term Regulation of Blood Pressure and body fluid volume, concentration, and composition! 1 How can we alter osmolality? • How can you make a fluid more concentrated? – Solute – Solvent- this changes volume • How can you make a fluid more dilute? – Solute – Solvent- this changes volume 2 Hormonal regulation of Osmolarity (And Blood Volume/Pressure) • ADH-water control • Angiotensin II- solute and water control • Aldosterone- solute and water control • Atrial Natriuretic Peptide (ANP—a.k.a atriopeptin) 3 ADH • Made in hypothalamus and released from posterior pituitary • Increases water permeability of principal cells and collecting ducts • Increases activity of Na+K+-2Cl- transporter • Increases urea permeability of inner medullary duct 4 Collecting Duct- tapping into the water reserve How much water is left to reabsorb? Tubular Cells Tubular Lumen H20 (depends on ADH) Aquaporin-3 H20 Aquaporins ADH cAMP V2 receptor Vesicle Aquaporin-2 H20 More water reabsorbed= concentrated, scant urine Less water reabsorbed= less concentrated, 5 copious urine Copyright © 2006 by Elsevier, Inc. Stimuli for ADH Secretion and Thirst • Increased osmolarity • Decreased blood volume – (cardiopulmonary reflexes) • Decreased blood pressure – (arterial baroreceptors) • Other stimuli: – – – – – – – dryness of mouth nausea Fever Burns excessive sweating vomiting, or diarrhea severe blood loss 6 Factors that decrease ADH and Thirst • • Decreased osmolarity Increased blood volume (cardiopulmonary reflexes) • Increased blood pressure (arterial baroreceptors) • Other factors: – alcohol (inhibits ADH!!!) – Gastric distention (inhibits thirst) A decrease in ADH means copious amounts of urine of dilute concentration Urea 7 Regulation of Sodium and water Balance: Angio II & Aldosterone • The renin-angiotensin mechanism triggers the release of aldosterone • This is mediated by the juxtaglomerular apparatus, which releases renin in response to: – Sympathetic nervous system stimulation – Decreased filtrate osmolality – Decreased stretch (due to decreased blood pressure) • Renin catalyzes (ultimately) the Macula production of angiotensin II, which prompts aldosterone release Sympathetic nerve fiber densa Juxtaglomerular cells 8 Renin-Angiotensin- System Made by Liver renin ACE in lungs 9 Angiotensin II Increases Na+ and Water Reabsorption • Stimulates aldosterone release • Directly increases Na+ reabsorption (proximal, loop, and in principal cells of late distal convoluted tubules) • Constricts efferent arterioles – Helps to maintain GFR and decreases peritubular capillary hydrostatic pressure – more reabsorption Ang II Ang II Na+ Na+ ATP Interstitial Fluid K+ H+ Na+ HCO3- Ang II Tubular Lumen 10 • Regulation of Sodium/ Potassium Balance: Aldosterone Hyperkalemia and hypokalemia can: – Disrupt electrical conduction in the heart – Lead to sudden death • Increased K+ in the ECF (hyperkalemia) around the adrenal cortex causes: – Release of aldosterone leads to K+ secretion • Potassium controls its own ECF concentration via feedback regulation of aldosterone release 11 Late Distal Convoluted Tubule Principal Cells Na + Na + K+ Tubular Lumen ATP K+ Cl - Aldosterone When aldosterone levels are high, all remaining Na+ is actively reabsorbed (last 8%) Aldosterone stimulates potassium ion secretion by principal cells For each Na+ reabsorbed, a K+ is secreted 12 Copyright © 2006 by Elsevier, Inc. Low K+ diet only Alkalosis! Normal or high K+ diet acidosis 13 Conn’s • Hyperaldosteronism • Hypernatremia • Hypokalemia (low potassium) • Hypertension Cushing’s • Hyperadrenalism-too much aldosterone and glucocorticoids • Hypernatremia • hypokalemia • Hypertension • Increased glucocorticoid production, resulting in excess blood sugar levels (resembling Diabetes Mellitus) • Increased androgen production, resulting in more masculinizing signs 14 Addison’s Disease • Primary adrenal insufficiency –not enough aldosterone and glucocorticoids • Hypoaldosteronism • Low blood pressure • Low sodium (hyponatremia) • High potassium (hyperkalemia) • Mild acidosis • Decreased glucocorticoid hormones, low blood sugar 15 Inhibitors of Aldosterone and Sodium Reabsorption • Atrial natriuretic peptide (ANP) • Increased Na+ concentration •(osmolality) ACE inhibitors (captopril, benazipril, etc) • Ang II antagonists (losartan, etc.) • decrease aldosterone • directly inhibit Na+ reabsorption of “reserve” • decrease efferent arteriolar resistance Natriuresis and Diuresis + Blood Pressure 16 Atrial Stretch Reflexes and ANP • Located in the atria of the heart. • Released due to increased ECF volume (stretch receptors in atria detect increased chronic venous return) • ANP – Vasodilation of afferent arterioles – Vasoconstriction of efferent arterioles – Increased GFR! – directly inhibits Na+ reabsorption – inhibits renin release (and hence, angio II production) and aldosterone formation – Reduces ADH release – helps to minimize blood volume expansion through potent diuretic and natriuretic effects 17 We must separate solute from solvent! Where will this occur in the nephron? Formation of a Concentrated Urineantidiuresis • Continue electrolyte reabsorption • Increase water reabsorption • Maximal urine concentration = 1200 - 1400 mOsm / L (specific gravity ~ 1.030) Formation of a Dilute Urine-diuresis • Continue electrolyte reabsorption • Decrease water reabsorption • Minimal urine concentration = 50 - 70 mOsm / L (specific gravity ~ 1.003) 18 Obligatory Water loss-Just how concentrated can the urine get? • The minimum urine volume in which the excreted solute can be dissolved and excreted. • Obligatory water loss reflects the fact that: – Kidneys excrete 600-1400 mOsm of solutes to maintain blood homeostasis – Urine solutes must be flushed out of the body in water Example: If the max. urine osmolarity was 1200 mOsm/L, and a minimum of 600 mOsm of solute must be excreted each day to maintain electrolyte balance, the obligatory urine volume is: 600 mOsm/d 1200 mOsm/L = 0.5 L/day 19 Water, water everywhere Nor any drop to drink (Coleridge’s: The Rime of the ancient Mariner) • Depending on the location, seawater varies from 2000-2400mOsm (8x that of plasma!) • You are dehydrated from being at sea-you drink 1L of seawater (2400mOsmoles!) • Your blood plasma now has a higher osmolality. • Maximum you can concentrate your urine ~1200mOsm-don’t forget the 600mOsmoles you MUST excrete for the day! • 3000/1200= 2.5L (that’s 1. 5L more than what you drank!) • Hey, Bear, should you really be drinking that urine? • 1200 + 600= 1800/1200= 1.5L! That’s 0.5 L more than what he drank! 20 Steps in production of a HYPER-osmotic urine • How does the kidney make a urine more concentrated than blood? • What determines how concentrated the urine will be? ADH! 21 Figure 28-8; Guyton and Hall thirst Osmoreceptor– antidiuretic hormone (ADH)-Thirst feedback mechanism for regulating extracellular fluid osmolarity Osmolality Plasma volume /Scant urine and HIGH urine osmolarity 22 With ADH around we create a scant, concentrated urine TAL- more solute reabsorption Principal cells of LDCT and collecting duct insert AQP2 More urea reabsorption of medullary duct 23 Syndrome of inappropriate ADH (SIADH) • Circulating levels of ADH are inappropriately HIGH • Head injury or tumors (lung) • Urine hyperosmotic • Plasma osmolarity decreased • Demeclocycline inhibits ADH activity in kidney 24 Production of a Hypo-osmotic urine Low levels of ADH PCT not affected: 67% of solute and water reabsorbed TAL- water not reabsorbed anyway EDT- solute reabsorption continues (diluting) LDT and collecting ducts- DO NOT express AQP2 gene (no water permeability) 25 Diabetes Insipidus-”bland urine of high flow” • Too little ADH • • • • • • Polydypsia (high thirst) Polyuria (high urine output) Urine osmolality? Plasma osmolality? 1) Central Diabetes Insipidus – head injury – Results from decreased production of ADH by the CNS – CD, therefore, has poor permeability to water and leads to diuresis – dDAVP- 1-deamino-8-D-arginine vasopressin 2) Nephrogenic Diabetes Insipidus – Deals with problem of nephron to sense ADH and malfunctioning ADH receptors in the Collecting Duct – CD, therefore, has poor permeability to water – Give thiazide diuretics 26 Let’s go through the hormones again, but with respect to solute maintenance • Sodium salts most abundant in ECF: – Account for 90-95% of all solutes in the ECF • Sodium is the only cation exerting significant osmotic pressure • Changes in plasma sodium levels affect: – Plasma volume, blood pressure – ICF and interstitial fluid volumes • Renal acid-base control mechanisms are coupled to sodium ion transport— review how! 27 REGULATION OF Na+ BALANCE • Sympathetic nerve activity- more Na+ reabsorption by PCT • R-A-A system: more sodium reabsorption • Atriopeptin (ANP: Atrial natriuretic peptide)- increases GFR and decreased Na+ reabsorption • Starling forces in peritubular capillaries 28 29 30 SNS can directly stimulate Na+ reabsorption in tubule cells, too! 31 Figure 26.9 32 Protein UP HCT N.C. Protein down HCT N.C. 33 TYPE EXAMPLE ECF ICF OSMOLARITY HCT PROTEIN ISO CONTRACTION DIARRHEA; BURN DOWN N.C. N.C. UP UP HYPER CONTRACTION SWEATING; DIABETES INSIPIDUS; dehydration DOWN DOWN UP N.C. UP HYPO CONTRACTION ADRENAL INSUFFICIENCY Abuse of diuretics DOWN UP DOWN UP UP ISO EXPANSION INFUSION OF ISOOSMOTIC NACL UP N.C. N.C. DOWN DOWN HYPER EXPANSION HIGH NACL INTAKE Conns ; Cushings UP DOWN UP DOWN DOWN HYPO EXPANSION SIADH UP UP DOWN N.C. DOWN Which rows are hypernatremia? Which rows show hyponatremia? 34 Hypertension • Primary- unknown cause. Treat the symptoms-diuretics, ace inhibitors, calcium channel blockers • Secondary- some other physiological event triggers the hypertension – Goldblatt: renin released inappropriately. Leads to cascade and ultimately increased blood pressure and hypertrophied heart muscle (CHF). • Anything that leads to decreased RBF/ low GFR will lead to renin release. • Anorexia, blockage in renal artery, etc. 35 DIURESIS-more water flow • Decreasing the amount of solutes reabsorbed in the tubules increases the water in the tubule and thus more urine output • diabetes mellitus (sweet urine of high flow): unreabsorbed glucose in tubules causes diuresis and water loss – Lack of insulin or failure of insulin to work (hyperglycemia) – High tubular loads and Tm for glucose is maxed – Polyuria – Glucosuria and ketonuria – Polydipsia (high thirst) • Many types of diuretics to cause changes in water reabsorption by altering solute reabsorption 36 OSMOTIC DIURETIC• • • • • • Mannitol- simple sugar, derived from mannose. Is small and freely filtered into kidney tubules and not harmful to pt. Given IV verses eaten To make it osmotic diuretic, it must not be reabsorbed. It must then stay in tubule lumen. (OBLIGATORY WATER LOSS!) Water stays in tubule to keep concentration at 300 mOsmolal. Water and mannitol is then excreted. Mannitol makes pt excrete more water. 37 Diuretics- thick ascending loop of Henle • Furosemide, aka “ Lasix” • Inhibits the Na+K+CLtransporters so the medullary interstitial gradient no longer exists • Water remains in the lumen • Very potent • Affects K+ balance, so risk of hypokalemia (which can affect RMP of excitable cells & cause hyperpolarization. 38 Diuretics- Early Distal CT • Thiazides • Inhibit Na/Cl transporters- no salt reabsorption. • Water stays in lumen 39 Diuretics- late DCT (aldosterone inhibitors) • Spironolactone • Decreases numbers of Na/K pumps on basolateral membranes so that NaCl reabsorption is blocked. • Results in more salt excreted (& water follows salt out so more water is also excreted) • Pro’s: prevents loss of K+ (potassium sparing diuretic). • Often used in conjunction with Loop diuretic • Con’s: can lead to hyperkalemia and Antiandrogen effect!! Female athletes use it to mask steroid use! Men have gynecomastia. 40 Diuretics- late DCT (sodium inhibitors) • Amiloride • Blocks Na+ channels on luminal membranes so that less Na+ is able to enter the tubule from the lumen in the first place. • Also potassium sparing— used with loop diuretic • Therefore, more is excreted and water follows 41