General Emergent Management of Patients with Acute Ischemic Stroke
advertisement

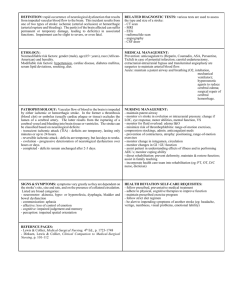
General Emergent Management of Patients with Stroke, Including Blood Pressure Management Objectives • Review initial evaluation of the patient with an AIS – history, physical exam, diagnostics, imaging • Discuss acute supportive care – stroke vital signs: ABCC’s, hypertension, glucose, temperature, seizure management • Understand that emergent management requires simultaneous evaluation and intervention Goals of Acute Supportive Care Assure optimal perfusion and oxygenation • Protect the C-spine • Secure the airway • Support oxygenation and ventilation • Assure appropriate circulation The History • • • • • • Age - approximately 65 yr Sudden onset focal neurologic deficit Specific vascular territory Seizure at onset of Sx: 5% Headache at onset: 10-30% Fall or trauma at onset Time of Symptom Onset • Most difficult portion of the history • Start when patient “was last seen normal” • Work forward in time (TV guide) • Patients that awake with symptoms onset = time of sleep • Confirm with family, friends, care taker • EMS - bring family along in ambulance Past Medical History • Medications: – diuretic, antihypertensive, antithrombotic • Risk Factors: hypertension smoking diabetes African-American TIA previous stroke atrial fibrillation carotid artery disease Physical Exam • Vital signs are vital, – but occasionally inaccurate • C-Spine tenderness, pain • BP in both arms, symmetry of pulses • Signs of trauma, associated injuries • Neurologic deficit characteristic vascular distribution Stroke Scales • Severity – NIH stroke scale 0-42, 0 = normal valid, reproducible, assists in patient selection, facilitates communication • Functional Scales – m-Rankin – Barthel index normal – Glasgow outcome 0-5, 0 = normal 100, 100 = 0-5, 5= normal • in NINDS t-PA stroke trial, 0 = normal Stroke Scales • NIH stroke scale 0-42 0-5 mild/minor in most patients 5-15 moderate 15-20 moderately severe > 20 very severe underestimates volume of infarct in nondominant (R) hemispheric strokes Diagnostic Testing • Laboratory studies – CBC, differential, platelets – electrolyte profile, glucose (finger stick) – INR, aPTT – Troponin • EKG • CXR Non-contrast CT of the Head • Initial imaging study of choice • Readily available • Very sensitive for blood in the acute phase – blood - 50-85 Hounsfield Units – bone- 120 (70-200) Hounsfield Units • Not sensitive for acute ischemic stroke – nearly 100% sensitive by 7 days • Posterior fossa structures - bone artifact Non-contrast CT of the Head • May shows early signs of ischemia in the 1st 3 hours – loss of gray/white matter distinction – hypodensity – mass effect, edema – hyperdense middle cerebral artery sign • Re-evaluate the time of symptom onset, if early signs of ischemia are present ECT 2 hours 24 hours Other Imaging Modalities • MRI – standard – DWI/PWI • Xenon CT • Perfusion CT • CT Angiography Differential Diagnosis • Deciphered by history, PE, diagnostics • DDx: TIA seizure trauma mass lesions vascular disorders infections (endocarditis) complex migraine metabolic abnormalities Stroke Vital Signs Airway Breathing Circulation C-spine Glucose Temperature Airway Management Upper airway patency • Maintain C-Spine precautions • Asses level of consciousness • Inspect for loose dentures, foreign bodies • Suction secretions • Assess gag reflex, tongue control Oxygenation and Ventilation • Respiratory rate and depth • Signs of fatigue - Paradoxical respirations • Breath sounds - (CHF, pneumonia, COPD) • Supplemental O2 with O2 sat > 95% • Support with Basic airway techniques • Ventilatory support as required Basic airway techniques • Foreign body removal • Suction with rigid suction device • Positioning – jaw thrust – chin lift • Nasal airway • Bag valve mask Advanced Airway Management • Rapid sequence intubation, orotracheal – sedation and paralysis prevent increase in ICP • Most common indications – inability to maintain airway – depressed level of consciousness – need for hyperventilation to manage ICP • Treat the underlying cause of respiratory distress: CHF, MI, etc. Monitoring of oxygenation • Pulse oximetry – indicator of oxygenation not ventilation – falsely high in CO poisoning – falsely low in PVOD, hypotension, peripheral vasoconstriction • ABG – pCO2 allows eval of ventilation – obtain from compressible site • Supernormal oxygenation – not of proven benefit Circulation • Goal: maintain cerebral perfusion • Optimize cardiovascular status • Monitor and reevaluate Circulation • Evaluate cardiac history and status • Cardiac output – preload – afterload – contractility – stroke volume Circulation • Monitor vital signs Q 15 min in acute phase – pulse (palpate in all 4 extremities) – heart rate – rhythm – blood pressure (both arms) – central venous pressure ECG • Cardiac Arrhythmia: 5% -30% • Acute MI: 1%-2% • ECG abnormalities – more common with hemorrhagic infarct – T-Wave inversions – nonspecific ST and T-wave changes Vascular Access • Two peripheral IVs • Use .9NS or .45 NS unless hypotensive • Use .9NS if hypotensive • Replace blood products as indicated Autoregulation • The ability of the vasculature in the brain to maintain a constant blood flow across a wide range of blood pressures • Autoregulation - impaired or lost in the area of the infarction • Ischemic tissues are perfusion dependant • Autoregulation is shifted to higher pressure patients with a history of HTN Autoregulation of Cerebral Blood Flow Ischemic 80 Normotensive 60 Hypertensive 40 20 MAP mm Hg 25 0 20 0 15 0 10 0 50 0 0 CBF ml/100mg/min 100 Hypertension Ischemic Stroke • Loss of autoregulation • Treat judiciously if at all • Treatment guidelines - not receiving rtPA – AHA: MAP > 130 or Sys BP > 220 • MAP= [(2x DP)+SP]B3 – NSA: 220/115 Hypertension - Ischemic Stroke • Drugs - short acting, titrate • Labetalol IV: 10-20 mg increments, double dose Q 20 min, max cumulative dose 300mg • Enalapril Oral: 2.5 - 5.0 mg/day, max 40mg/day IV : 0.625-1.25 mg IV Q 6hrs, max 5.0 Q 6 hrs Hypertension -Ischemic Stroke • Nitroglycerine Paste: 1-2 inches to skin IV Drip: 5mcg/min, increase in increments of 5-10mcg every 3-5 min • Nitroprusside IV Drip: 0.3 - 10 mcg/min/kg Continuos BP monitoring check thiocyanate levels • AVOID NIFEDIPINE Hypertension Intracerebral Hemorrhage • Treat aggressively • Elevate head of bed • Use labetalol, nitroglycerine, nitroprusside or lasix • AVOID NIFEDIPINE • Keep systolic < 160 mm Hg diastolic < 100 mm Hg Hypotension • • • • More detrimental than hypertension Seek cause and treat aggressively CVP monitoring may be necessary Use .9 NS first to ensure adequate preload • Then add vasopressors if needed Hypertension: rt-PA Candidate • Exclude for persistent BP > 185/110 • Check BP q 15 min • May not aggressively lower BP to meet entry criteria • Use Labetolol or Nitropaste • Avoid Nifedipine Glucose • Worse outcome after stroke: – diabetics – acute hyperglycemia at time of infarct • Mechanism uncertain – increase in lactate in area of ischemia – gene induction, – increased number of spreading depolarizations • Insulin is a neuroprotective Glucose • Avoid any IV fluids with D5 – instruct prehospital personnel not to give D50 as part of the “coma cocktail” to acute stroke patients • Check a finger stick ASAP – treat only if low (< 50) • Use insulin to establish euglycemia Temperature • Fever worsens outcome: – for every 1°C rise in temp, risk of poor outcome doubles (Reith, Lancet 1996) • Greatest effect in the first 24 hours • Brain temp is generally higher than core • Treat aggressively with acetaminophen, ibuprofen, or both • Search for underlying cause • Hypothermia currently under investigation Seizures • Occur in 5% of acute strokes • Usually generalized tonic-clonic • Possible causes: severe strokes cortical involvement unstable tissue at risk spreading depolarizations hx of seizure disorder Seizures • Protect patient from injury during ictus • Maintain airway • Benzodiazepines: – lorazepam (1-2 mg IV) – diazepam (5-10 mg IV) • Phenytoin: – 18 mg/kg loading dose, at 25-50 mg/min infusion with cardiac monitor • No need for prophylaxis Primary treatment of AIS • • • • Supportive care Aspirin IV thrombolysis No role for antithrombotics Summary Evaluation • History with time of symptom onset • Physical exam – trauma, NIHSS score • Laboratory evaluation • Non-contrast CT head Summary Supportive Care • • • • • • • • Secure airway; basic and advanced methods Protect C-spine Assure oxygenation and ventilation Maximize perfusion, IV fluids Blood pressures (both arms), treat carefully Normalize the temperature and glucose Treat seizure if occurs Reevaluate