Slides - Rowan University
advertisement
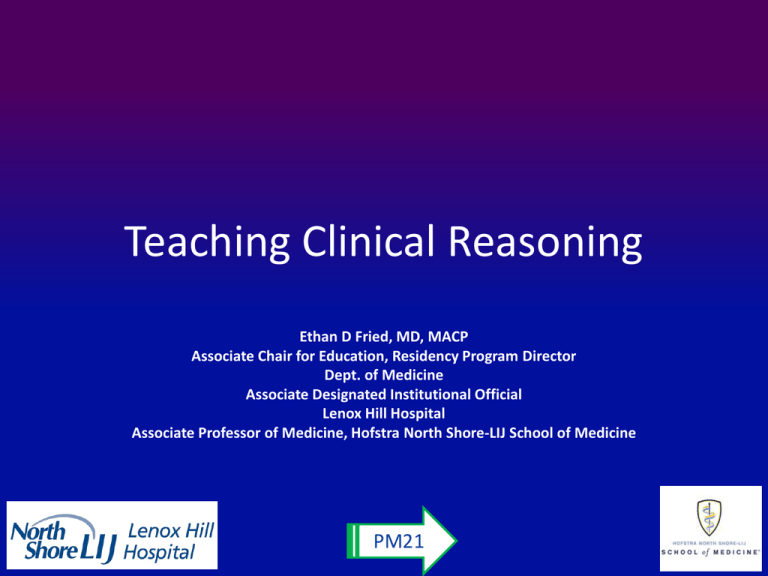
Teaching Clinical Reasoning Ethan D Fried, MD, MACP Associate Chair for Education, Residency Program Director Dept. of Medicine Associate Designated Institutional Official Lenox Hill Hospital Associate Professor of Medicine, Hofstra North Shore-LIJ School of Medicine PM21 Presentation Skills Patient Interview • • • • • • • • • • Doctor: Hello Mr. Smith. What brings you in to see me today? Patient: Hello Doctor. I have a pain in my groin. D: Oh I see. Sorry to hear that. Tell me more about it. P: It started about 2 weeks ago and it comes and goes. But each time it comes it gets worse. Last night it woke me up. D: What sort of pain is it? P: Mostly a dull pain but sometimes it’s sharp. It’s mostly in my groin but when it’s bad it comes up into my belly. D: Does it go anywhere else? P: Yes. To my lower back too when it’s really bad. D: How bad is it on a scale of 1 to 10. P: Mostly it’s a 3 or 4 but when it’s bad it’s a 10 PM21 Presentation Skills Patient Interview (2) • • • • • • • • • • D: Do you vomit? P: Not usually but once I did. D: What came up? P: Just green fluid. D: No blood? No coffee grounds? P: No D: Any fever? Chills? P: No D: Sweating at night? P: No PM21 PM21 Presentation Skills Patient Interview (3) • D: Do you have any shortness of breath? • P: No • D: Palpitations? Do you feel an uncomfortable sense of your own heart beat? • P: No • D: Cough? • P: No • D: I thought that the pain is worse when you cough. • P: Yeah. But just a regular cough. You know. Like everyone. • D: Tell me about this cough. • P: It’s nothing really. I sometimes cough in the morning. PM21 Presentation Skills Patient Interview (4) • • • • • • • • • • • • D: Do you bring anything up? P: Just phlegm. Plus a little bit of blood. D: I’m sorry. Did you say that you cough up blood every morning? P: Not every morning. But yes. I guess so. D: How long has that been happening? P: Oh boy. For a while. Maybe 6 months. D: Any fever during that time? P: No I don’t think so. D: Chills, Sweats at night? P: No D: Weight change? P: I have lost some weight. Maybe 20 pounds since the winter. PM21 PM21 Summarizing a Clinical Case* • First, you have to think about what you believe is the diagnosis. • Account for ALL of your findings (not just the ones that fit your first impression). • Re-tell the story in chronologic order (not necessarily the order that you found out the information). • Use semantic qualifiers to cue the listener as to what you are thinking. PM21 Interpretive Summary Semantic Qualifiers • Acute • Sudden • Delayed • Progressive • Constant • Unilateral • Painful • Mild • Associated with • • • • • • • • • PM21 Chronic Gradual Abrupt Waning Intermittent Bilateral Painless Severe Followed by Outline (HPI) I. What is the patient milieu? A) Age, sex B) Underlying illnesses or risk factors II. What is (are) the current problems A) Tell the clinical story* B) Use the 7 dimensions of a symptom (or PQRST, or whatever) C) By this point, the listener should have a pretty good idea of what is happening III. What is this NOT? A) Pertinent negatives PM21 6 Mechanisms of Injury – Infectious – Neoplastic – Immune/Inflammatory – Metabolic – Toxic/Traumatic – Delivery (oxygen, blood, nutrients, etc.) PM21 As quick as you can … • A bat and a ball together cost $1.10 • The bat costs $1.00 more than the ball • How much does the ball cost? PM21 Critical Thinking Quiz 1) 2) 3) 4) 5) 6) 7) Do they have a 4th of July in England? How many birthdays does the average man have? Some months have 31 days, how many have 28? Why can't a man living in the USA be buried in Canada? How many outs are there in an inning? Is it legal for a man in California to marry his widow's sister? Two women play five games of checkers. Each woman wins the same number of games. There are no ties. Explain this. 8) Divide 30 by 1/2 and add 10. What is the answer? 9) There are 3 apples and you take away 2. How many do you have? 10) If you have only one match and you walked into a room where there was an oil burner, a kerosene lamp, and a wood burning stove, what would you light first? PM21 Critical Thinking Process Overview • Overcoming bias: – Heuristics: • A) Thaddeus is an investment banker • B) Thaddeus is a Republican investment banker – Intuition: 5/yr • A) # of deaths by shark attack 2900/yr • B) # of deaths by hippo attack • Experience/Context PM21 What do we know and how do we know it? • History and Physical – – – – Failure to ask Failure to look Language barriers Poor history taking skills • Open ended questioning • “Tell me more” • “Anything else?” – Physical exam deterioration • Auscultation through clothing • Inadequate palpation skills • Failure to recognize abnormalities • Inadequate space to evaluate • Equipment inadequate or unavailable • Medical Records – Failure to obtain/find information – Propagation of inaccurate information • Other secondary sources • Failure to recognize abnormalities • Faulty reading of study/labs PM21 Affective Factors/Assumptions • Patient is behaviorally difficult • Patient is likeable • Physician is fatigued • Cognitive overload • Physician is uncomfortable admitting knowledge deficit • • • • • Rare symptoms Rare diseases Complex problem list Too many consultants “Routine” (social admission) patient • VIPs PM21 Can we draw conclusions based on current evidence? • What else do we need to know? • What other ideas should be explored? • Have we used a systematic process to recognize competing solutions? • What are best alternate diagnoses? Why don’t they win? PM21 Causes of Misdiagnosis Data Gathering Specific Presentation Context Diagnostic Error Patient Presentation Affective Factors Faulty Reasoning Organizational PM21 Ten Commandments of Clinical Reasoning 1) 2) 3) Thou shalt reflect on how you think and decide. Thou shalt not rely on your memory when making critical decisions. Thou shalt make your working environment information-friendly by using the latest wireless technology such as the Tablet PC and PDA. 4) Thou shalt consider other possibilities even though you are sure of your first diagnosis. 5) Thou shalt know Bayesian probability and the epidemiology of the diseases in your differential diagnosis. 6) Thou shalt mentally rehearse common and serious conditions that you expect to see in your specialty. 7) Thou shalt ask yourself if you are the right person to make the final decision or a specialist after considering the patient’s values and wishes. 8) Thou shalt take time to decide and not be pressured by anyone. 9) Thou shalt create accountability procedures and follow up for decisions made. 10) Thou shalt record in a relational data base software your patient’s problems and decisions for review and improvement. Leonardo L. Leonidas, MD Tufts University School of Medicine, Boston, USA PM21 Bias in Clinical Reasoning • Premature Closure – Anchoring, Representativeness restraint, Confirmation bias • Insufficient Knowledge – Availability, Ascertainment • Fatigue – Order effect, Zebra retreat, Multiple alternative • Prejudice – Psych out, Gender • Gambling – Sutton’s slip, Posterior probability PM21 Dual Process Theory PM21 Steps in Clinical Reasoning 1) Patient’s Story 2) Data Acquisition 3) Accurate “problem representation” 4) Generation of hypothesis 5) Search for and selection of an illness script 6) Diagnosis PM21 Four Basic Questions • What else could this be? • What finding does not fit with my diagnosis? • Could there be multiple processes going on at once? • Is there any other reason I need to slow down? PM21 Context + IDEALS • Context – H&P/2ndary sources/Knowledge • Identify/Frame the problem – Represent the illness as semantic qualifiers • • • • • Determine potential roots of bias Enumerate solutions systematically Assess best solutions List reasons why one solution is best Self-correct after counter propositions PM21 Avoiding Cognitive Errors • • • • Improve data collection Building illness scripts Beware of heuristics, bias, intuition Systematic problem solving – Know your biases – Acknowledge emotions • Reducing reliance on memory • Review errors PM21 Dialogue 1 • • • • • • • • • • • • • The patient is a 52 year old man. He is exhausted and sighs and yawns frequently during the interview. Doctor: Good afternoon Mr. G. What brings you to see me today? Patient: Oh, hello doctor. I’m just so tired lately. Dr.: Really, how long has this been going on? Pt: Well, let’s see. I started noticing it about 3 months ago and it has been getting worse ever since. Dr.: Are you getting enough sleep? Pt.: That’s just it Doc. It doesn’t matter how much sleep I get. I’m still tired. Dr.: I see. Tell me more about your symptoms for the last 3 months. Have you noticed any other changes? Pt.: What do you mean? Dr.: Any change in your weight? Pt.: Yes, I have lost weight. Like 10 pounds. Dr.: Is your appetite good? Pt.: Yes – I’ve been eating like a horse. PM21 • • • • • • • • • • • • • • Dr.: Hmmm. Anything else? Pt.: I don’t know. Sometimes my vision is blurry. Dr.: When does that happen Pt.: Varies. No specific time. I just notice it sometimes. Later in the day it is normal again. Dr.: OK. What else? Pt.: That’s all I can think of. Dr.: Well, let me ask you some specific questions just to make sure that we haven’t missed anything. Pt.: OK Doc. Ask me anything. Dr.: Is everything alright at home? Any unusual stresses? Pt.: Nothing that’s over the top. My daughter is finishing college. She will need a job. It’s a pretty bad economy out there. But I wouldn’t say that I am loosing any sleep over that. Dr. OK. What about just going from head to toe. Any headaches? Pt: No Dr.:We already talked about your vision. Any pain or discharge from the eyes? Pt.: No PM21 • • • • • • • • • • • • Dr.: Trouble swallowing? • Pt.: No Dr.: Trouble hearing? Pain or discharge • from the ears? • Pt.: No • Dr.: How’s your breathing? • Pt.: OK • Dr.: How far can you walk? • Pt.: Only 2 blocks without resting Dr.: Is that because of your breathing? • • Pt.: No – Just tired. • Dr.: Any cough? • Pt.: No • Dr.: When you do cough, do you bring anything up? Pt.: No Dr.: Any chest pain? Pt.: No Dr.: Any palpitations? Pt.: What is that? Dr.: The uncomfortable sensing of your own heart beat. Pt.: Oh my - no Dr.: Any trouble with your bowels? Pt.: Sometimes I feel bloated Dr.: Diarrhea? Pt.: No PM21 • • • • • • • • • • • • Dr.: Constiipation? • Pt.: No • Dr.: Nausea/Vomiting? • Pt.: No Dr.: Any blood in the stool? • Pt.: No Dr.: Does your stool ever turn black• and tarry? • Pt.: No • Dr.: How about your urination? Pt.: Tons of it. • Dr.: What do you mean? • Pt.: I go 8 – 10 times a day Dr.: That’s a lot. Each time you go, is it a full load of urine or just little spurts? Pt.: No – Full loads Dr.: Afterward do you feel empty or like you still have to go? Pt.: Empty Dr.: And is there any burning or pain with urination? Pt.: No Dr.: Any blood in the urine? Does it ever turn pink or red? Pt.: No Dr.: OK I think I have a handle on your problem. We’ll need to do some testing but I think I know what’s been happening to you. PM21 Dialogue 2 • • • • • • • • • • • • • P:Good Afternoon, doctor. D:Good afternoon. What is your problem? P:I have a stomachache. D:What do you feel? P:I have a strong pain and heartburn. D:How long have you had this pain and acidity? P:For 2 months now. It does not go way! I eat and after every meal my stomach hurts. Even at night the pain persists. D:Tell me, in the last 2 months, have you eaten any kind of heavy food, or something different? P:No. D:How strong is the pain. Lets say in a 1 to 10 scale, how would you describe the intensity of the pain? P:Between 4-5 D:Is the pain continuous or does it come and go? P:It come and goes. PM21 • • • • • • • • • • • • • • • • D:Does the pain come after meals? P:That's possible because it hurts everytime after eating. D:Is there a kind of food that affects you more? P:Greasy food. D:Greasy food affects you? P:Yes. At home we eat a lot of greasy food. D:Where in the abdomen does it hurt? Point please! Does the pain travel to your chest, shoulder, back or across your abdomen? P:It hurts in the middle. Sometimes, the pain travels across my abdomen. D:Besides the pain, you said you have heartburn? P:Yes, after a burp, I feel a kind of sour taste. D:Do you feel like this more during the day or in the evenings? P:Both. I feel the acidity during the day and at night. D:Is it worse when lying down? P:Yes, I taste the acid in my mouth? D:Besides greasy food, is there any other kind of food that irritates your stomach? Like spicy food? P:No, at home we don't eat spicy food. PM21 D:And tell me, how often do you regularly have a bowel movement? Has that changed since you have been having these problems? P:It is regular. It hasn't changed since the problem. D:Have you noticed any change in the consistency of the bowel movement? P:Yes. It is a bit softer. D:Have you noticed any change in color? P:Yes, it is greener. D:Greener, not darker? Any blood in your bowel movement or black coloring to bowel movement? P:No, not darker. I do not see any blood in my bowel movement, either. PM21 Case Records of the Massachusetts General Hospital Case 35-2015 — A 72-Year-Old Woman with Proteinuria and a Kidney Mass D. Bora Hazar, M.D., Nwamaka D. Eneanya, M.D., M.P.H., Aoife Kilcoyne, M.D., and Ivy A. Rosales, M.D. N Engl J Med Volume 373(20):1958-1967 November 12, 2015 PM21 Summary • A 72-year-old woman presented with flank pain, proteinuria, and a new kidney mass. • Magnetic resonance imaging of the kidney revealed a complex, solid mass (3 cm x 2.9 cm x 2.9 cm) in the lower pole of the right kidney. • Diagnostic tests were performed. PM21 MRI Scans. Hazar DB et al. N Engl J Med 2015;373:1958-1967 PM21 Biopsy Specimens of the Renal Mass (Hematoxylin and Eosin). Hazar DB et al. N Engl J Med 2015;373:19581967 PM21 Biopsy Specimens of the Uninvolved Kidney. Hazar DB et al. N Engl J Med 2015;373:1958-1967 PM21 Laboratory Data. Hazar DB et al. N Engl J Med 2015;373:1958-1967 PM21 Conditions and Associated Glomerular Diseases in Patients with Adult Nephrotic Proteinuria. Hazar DB et al. N Engl J Med 2015;373:19581967 PM21 Final Diagnosis • PLA2R-type membranous nephropathy. • Clear-cell renal-cell carcinoma. PM21