Training - Hamilton Health Sciences
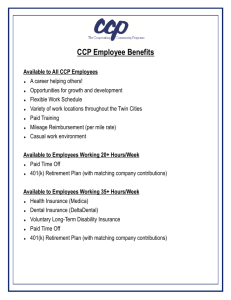
advertisement

DIFFICULT AIRWAY Review Kenneth W. Stuebing Program Manager A-EMCA, Critical Care Flight Paramedic Objectives During this presentation we will discuss: – – – – – – – – – A systematic approach to airway assessment Common terminology (talk the same language) Pediatric airway concerns Difficult airway assessment Introduce facilitated intubation Introduce Rapid Sequence Induction CONCEPTS Introduce alternate airway adjuncts Introduce an AIRWAY algorithm Practice airway procedures Kenneth W. Stuebing EMCA, CCP(F) STRESSED ? Let me paint the picture for you! – WHEN: 16:00 hrs. on Friday – WHERE: MAIN & JAMES – WHAT: 8 year old female patient who was hit by a speeding car (approximately 90 kph) – She is unconscious, responds with groans to pain, does not open eyes and withdraws from pain. She has a pulse of 50 and is breathing but you notice her skin is pale and lips are blue. She is bradycardic, hypotensive and tachypnic. You note multiple fractures and copious amounts of blood loss with paradoxical (seesaw) breathing. Her air entry is markedly diminished on the left side and crackles on the right (aspiration?). She has a blown left pupil and lateralizing signs. Kenneth W. Stuebing EMCA, CCP(F) First Things First Indications for intubation – – – – – – – LOC Obtain / Maintain / Protect Airway Oxygenation Positive Pressure Ventilation or control ventilation Drugs (NAVEL) Fatigue Access Tracheal Toilet (suction) Kenneth W. Stuebing EMCA, CCP(F) Why PAINFUL STIMULUS? MEDICAL TRAUMA PROTECT C-SPINE Kenneth W. Stuebing EMCA, CCP(F) RESPIRATORY PROCESS ALVEOLAR PRESSURE < ATMOSPHERIC MECHANICAL: ATMOSPHERIC PRESSURE > ALVEOLAR PRESSURE NATURAL: Kenneth W. Stuebing EMCA, CCP(F) SELLICK MANEUVER or CRICOID PRESSURE FINGER PRESSURE ON CRICOID CARTILAGE WHICH AIDS IN INTUBATION AND PREVENTS GASTIC DISTENTION & ASPIRATION Kenneth W. Stuebing EMCA, CCP(F) Airway Assessment Once the decision to intubate has been made a deliberate assessment process needs to be started. Is it a CRASH intubation? – Death or near death (like “NIKE” “just do it”) – Suction, stylette, lubed ETT, stethoscope, laryngoscope Is it a DIFFICULT intubation? – LEMON (DO YOU NEED TO LOAD YOUR PATIENT ?) Rapid Sequence Induction / Intubation (RSI) future? – Sedation, analgesia, neuromuscular blocking agent Kenneth W. Stuebing EMCA, CCP(F) CRASH AIRWAY VSA Pending VSA Respiratory Arrest GCS < 5 Airway compromise (blood / vomit unable to clear) Note: positioning is the number 1 airway procedure to prevent aspiration. Kenneth W. Stuebing EMCA, CCP(F) DIFFICULT AIRWAY LEMON assessment scale. – Prior to taking TOTAL control of airway – May choose to facilitate intubation (versed) – May need to LOAD patient Lidocaine Opiate Atropine Depolarizing neuromuscular blocking agent (defasiculating) Kenneth W. Stuebing EMCA, CCP(F) LEMON L - Look 1 point E - Evaluate 2 points M - Mallampati (1 - 4) 2 points O - Obstruction 2 points N - Neck 1 point 2 or more equals difficult Kenneth W. Stuebing EMCA, CCP(F) LEMON L - Look (visual assessment) 1 point (each) – – – – – Under / over bite Big teeth Facial hair No neck Barrel chest Gut feeling tough tube!!! Kenneth W. Stuebing EMCA, CCP(F) LEMON E - Evaluate 2 points – Ability to open mouth 3 fingers – Anterior Larynx 3 fingers – Superior Larynx 2 fingers Children and Asians have anterior and superior larynx. Kenneth W. Stuebing EMCA, CCP(F) LEMON M - Mallampati – – – – (1 - 4) = 0 or 2 points 1 = can see all of uvula 2 = can see most of uvula 3 = can see a part of uvula 4 = can see none of uvula - all hard palate Paramedics should lean to a 1 or 4 interpretation. Kenneth W. Stuebing EMCA, CCP(F) LEMON O - Obstruction 2 points – Tumors – Hematoma – Swelling Kenneth W. Stuebing EMCA, CCP(F) LEMON N - Neck – – – – – 1 point Immobility, unable for flex or extend neck C -spine precautions Kyphosis Osteoporosis Severe Rheumatoid Arthritis 2 or more equals difficult airway is expected Kenneth W. Stuebing EMCA, CCP(F) What if it is difficult? Concern for paralytics and heavy use of analgesics and sedatives. If patient quits breathing and you are unable to ventilate - you have broken fundamental premise of medicine “CAUSE NO HARM”. Before taking TOTAL control of a patient’s airway an accurate / defendable assessment for due diligence AND a back up must be available. Blind nasal intubation with slight sedation may be beneficial. Kenneth W. Stuebing EMCA, CCP(F) Facilitated Intubation Sedation (decrease LOC) – Versed (January 2002 with patch) concerns for hypotensive patients helps blunt sympathetic response amnesia Analgesia (stop pain) – Morphine concerns for hypotensive patients helps blunt sympathetic response – Fentanyl (synthetic opiate 100 x stronger than morphine) concerns for hypotensive patients helps blunt sympathetic response Kenneth W. Stuebing EMCA, CCP(F) Versed Madazolam HCL Classification: Sedative (anxiolytic and hypnotic) – CNS depressant (benzodiazepines, barbiturates, etc) Mode of Action: – Inhibitory action of the GABA receptors (ý~aminobutyric acid): When GABA binds to CNS receptors it increases the chloride that enters the cell. This causes a SMALL hyperpolarization and moves the postsynaptic receptor away from its action potential. (resting potential more negative) Benzodiazepines bind to specific, high affinity sites on CNS cell membranes beside GABA receptors, resulting in more frequent opening of the chloride channels. This hyperpolarizes the postsynaptic receptor even MORE then GABA alone and further inhibits neuronal firing. Benzodiazepines also interfere with the release of calcium from the sacroplasmic reticulum in the CNS inhibiting these cells further. Kenneth W. Stuebing EMCA, CCP(F) Benzodiazepines BENZODIAZEPINES: – GABA receptors are only found in the CNS – have no analgesic or anti psychotic effects – do not affect the autonomic nervous system (still BP caution) – all have exhibit varied level of these actions: Anxiolytic Muscle relaxant Sedative / hypnotic Anticonvulsant Kenneth W. Stuebing EMCA, CCP(F) Benzodiazepines BENZODIAZEPINES: – Anxiolytic at low doses they are anxiolytics, thought to selectively inhibit neuronal circuits in the brain’s limbic system. – Muscle Relaxant relax spasticity of skeletal muscle, by increasing presynaptic inhibition of the spinal cord. Kenneth W. Stuebing EMCA, CCP(F) Benzodiazepines BENZODIAZEPINES: – Sedative / hypnotic All Benzos have these properties at high doses can cause hypnosis and respiratory depression and hypotension. – Anticonvulsant Several types are used to treat epilepsy however some don’t have a long enough half life to be useful. Kenneth W. Stuebing EMCA, CCP(F) Benzodiazepines Pharmacology: – Absorption and distribution: Lipophilic benzodiazepines are rapidly & completely absorbed after PO, IV & SQ administration & distributed evenly throughout the body. – Duration of actions: Half lives of this classification of drug are VERY important for their clinical use. They are divided into 3 categories: Long acting: (Valium / Diazepam) Intermediate acting: (Lorazepam) Short acting: (Triazolam, Versed) – Metabolism & Excretion: most are metabolised in the liver and therefore caution should be used when administering to people with hepatic dysfunction eliminated in the urine. Kenneth W. Stuebing EMCA, CCP(F) Versed Madazolam HCL Adverse affects: – – – – Drowsiness and confusion Hypoventilation Tackycardia / bradycardia Hypotension Caution: – It will potentiate effects of alcohol and other CNS depressants Versed in use by January - February 2002 Dose: > or = 40 kg 0.05mg/kg (0.1 mg/kg) Kenneth W. Stuebing EMCA, CCP(F) RSI Induction / Sedation – Versed & Morphine (?) Neuromuscular blocking agent – Succinylcholine (depolarizing or fasiculating) Acetylcholine Agonist: causes systemic release of ALL acetylcholine from motor nerve endings which bind to nicotinic receptors on the neuromuscular endplates of all skeletal muscle. This causes a fasiculation (seizure) while all muscles contract or depolarize at once. Since ALL acetylcholine is released it is impossible for muscle contraction to occur until stores have been replenished. – Note: skilled practitioners can usually intubate ~ 80 - 90% of the population without too much trouble. The remaining 10 - 20 % falls under the difficult to very difficult category. Kenneth W. Stuebing EMCA, CCP(F) LOAD Lidocaine – to blunt ICP for patient with: CVA Head Injuries Opiate - Analgesia – Fentanyl concerns for hypotensive patients will also blunt ICP and reduce sympathetic response Atropine (have ready) – to stop vagal response - particularly pediatrics Defasiculating neuromuscular blocking agent - ART – used to stop fasiculation caused by Succinycholine Kenneth W. Stuebing EMCA, CCP(F) Emergency Cricothyrotomy Protocol If a patient cannot be ventilated due to life-threatening suspected upper airway obstruction, the Advanced Care Paramedic may attempt a cricothyrotomy according to the following protocol after receiving orders from the BHP. Indications: A patient that requires intubation and Unable to intubate and Unable to adequately ventilate Conditions: Patient 40 kg and 12 years old Contraindications: Suspected fractured larynx Inability to localizeKenneth the W. cricothyroid membrane Stuebing EMCA, CCP(F) Emergency Cricothyrotomy Protocol Procedure: 1. Administer 100% O2. 2. Contact the BHP for on-line medical direction to proceed with this protocol. 3. If every attempt to contact a BHP has failed, the AC Paramedic may continue with this protocol in a life-threatening situation if all other indications and conditions are met. The AC Paramedic should contact the BHP (and the Base Hospital) as soon as possible after the procedure and document the patch failure and decision to proceed. 4. Place patient on his or her back, and then extend the head and neck (provided there are no c-spine injuries). 5. Grasp the larynx with your thumb and middle finger. Locate the cricoid cartilage and the cricothyroid membrane with the index finger. Prep the area quickly. Follow the appropriate procedures following for the specific equipment used. The seldinger cricothyrotomy should be the primary method used but if the equipment is not available, the needle cricothyrotomy procedures should be followed. Kenneth W. Stuebing EMCA, CCP(F) Emergency Cricothyrotomy Protocol Seldinger (Melker) Cricothyrotomy Kit: 1. While stabilizing the thyroid cartilage make a vertical incision in the midline of the cricothyroid membrane with a scalpel. 2. Use the supplied 18g TFE catheter with the 6cc syringe attached. Insert the catheter into the airway at a 45º caudal angle looking for free air in the syringe. 3. Remove the syringe and needle leaving the catheter in place. Always maintain contact with the guidewire, never let go! 4. Advance the soft flexible end of the wire guide through the catheter and into the airway several centimeters caudally. 5. Remove the catheter leaving the wire guide in place. (STEP # 1) 6. Feed the dilator (with airway catheter in place) over the wire. Ensure that the stiff end of the wire protrudes out of the back of the dilator. 7. Advance the dilator into the airway until the flange of the 15mm airway adapter is resting against the patient's neck. 8. Remove the dilator and wire guide. Use caution to ensure that the wire guide is not lost into the trachea. 9. Secure the flange of the airway adapter to the patient. 10.Attach a BVM and attempt to ventilate the patient. Genesis or other ventilators must not be used. 11.Initiate rapid transport to the closest appropriate hospital. 12.Patch to the Base Hospital if complications arise or further orders Kenneth W. Stuebing EMCA, CCP(F) are required. Emergency Cricothyrotomy Protocol Needle Cricothyrotomy: 7. Attach a 14 gauge over-the-needle catheter to a 10 cc syringe filled with saline. Carefully insert the needle through the skin and cricothyroid membrane into the trachea while aspirating for free air. Direct the needle at a 45 degree angle caudally. 8. Aspirate with the syringe. If air is returned easily by way of seeing bubbles in the saline filled syringe, you are in the trachea. If it is difficult to aspirate with the syringe, or if you obtain blood, re-evaluate needle placement. 9. Withdraw the stylette, while gently advancing the catheter downward into position. 10.Attach an adapter to the hub of the catheter and begin ventilating with 100% O2 with a BVM. Genesis or other ventilators must not be used. 11.Secure the catheter and continue ventilation, allowing time for passive expiration 12. Initiate rapid transport to the closest appropriate hospital. 13. Patch to the Base Hospital if complications arise or further orders are required. Kenneth W. Stuebing EMCA, CCP(F) Needle Cricothyroidotomy SECOND LINE PROCEDURE that should be used if Seldinger technique is not possible. (BHP may give orders from 8 - 12 year old patient) Provides temporary oxygenation but no ventilation Note: Exhalation may be difficult through such a small diameter catheter and the paramedic should lengthen the time between breaths to allow for exhalation. The BHP may consider giving orders for a second catheter horizontally next to the first to allow for better exhalation and this should be discussed during the patch. Kenneth W. Stuebing EMCA, CCP(F) Cricothyroidotomy (Melker) Kenneth W. Stuebing EMCA, CCP(F) Cricothyroidotomy (Melker) 2 Landmark cricothyroid membrane between the thyroid and cricoid cartilages and prep area. Maintain landmark with one hand & insert the 6cc syringe with 18 guage TFE catheter and introducer needle. Advance needle on a 45° angle to the frontal plane in the midline in a caudad direction. While inserting needle draw back on syringe to verify when trachea has been found. Kenneth W. Stuebing EMCA, CCP(F) Cricothyroidotomy 3 Remove the syringe and needle leaving the catheter in place. Advance the soft, flexible end of the guidewire through the TFE catheter and into the airway several centimeters. 4 While holding on to the guidewire ensuring not to let it move carefully remove the TFE. Kenneth W. Stuebing EMCA, CCP(F) Cricothyroidotomy 6 5 While holding the guidewire make a vertical incision with the # 15 short handle scapel blade to allow dilator to be inserted. While holding on to the guidewire advance the preassembled dilator and airway catheter with the tapered end first over the guidewire. Kenneth W. Stuebing EMCA, CCP(F) Cricothyroidotomy Kenneth W. Stuebing EMCA, CCP(F) Cricothyroidotomy Kenneth W. Stuebing EMCA, CCP(F) PLAY EMERGENCY AIRWAY VIDEO! Airway Assessment Algorithm CRASH INTUABTION DEATH OR NEAR DEATH INTUBATE: Lubricated Tube Stylette Suction Stethescope Syringe YES NO SUCCESSFUL? NO YES: Confirm (see Note 1) DIFFICULT AIRWAY LEMON No CONSIDER PATCH FOR FACILITATED INTUBATION: Versed/Morphine Consider Lidocaine Yes SUCCESSFUL? NO Rapid Sequence Induction / Intubation (future consideration) REASSESS (see Note 2) No YES Versed Fentanyl Succinylcholine SUCCESSFUL? YES: Confirm (see Note 1) Consider Adjunct Devices Lighted Stylette LMA Can you ventilate the patient? NO YES Perform Cricothyrotomy Note 1: Note 2: Continue to ventilate with adjunct or BVM Confirmation includes 3 methods with 1 being end tidal CO2 confirmation Reassess continually to determineEMCA, whether theCCP(F) patient’s condition reverts to Kenneth W. Stuebing “Crash Intubation” or “Facilitated” criteria. NO Airway Assessment Algorithm CRASH INTUABTION DEATH OR NEAR DEATH INTUBATE: Lubricated Tube Stylette Suction Stethescope Syringe YES NO SUCCESSFUL? NO YES: Confirm (see Note 1) DIFFICULT AIRWAY LEMON No CONSIDER PATCH FOR FACILITATED INTUBATION: Versed/Morphine Consider Lidocaine Yes SUCCESSFUL? REASSESS (see Note 2) Consider Adjunct Devices Lighted Stylette LMA Can you ventilate the patient? NO Perform Cricothyrotomy Note 1: Note 2: YES Continue to ventilate with adjunct or BVM Confirmation by 3 methods; one must be end-tidal CO2 (when available). Reassess continually determine whether the patient’s CCP(F) condition reverts to Kennethto W. Stuebing EMCA, “Crash Intubation” or “Facilitated” criteria. NO Questions Kenneth W. Stuebing EMCA, CCP(F) Reference Material Website @ www.springnet.com/criticalcare PALS / NALS The ICU Book by Paul L. Marino Hemodynamic Monitoring by Darovic Lippicotts Pharmacology Merck Manual Hemodynamic Monitoring by Dana Oakes Handouts - Compiled Information (Sunnybrook) Kenneth W. Stuebing EMCA, CCP(F) Thank you Kenneth W. Stuebing Clinical Co-ordinator H.B.H. CCP(F), AEMCA Kenneth W. Stuebing EMCA, CCP(F)