INCIDENT REPORTS - The Moore Center

INCIDENT REPORT POLICY & PROCEDURE
Notable Events
1. Notable Events a. A Notable Event may be an occurrence that takes place during non-service/non-staffed hours;
Supervision is not provided by the agency;
Includes programs such as Independent Living, Family
Support, PCS, or IHS.
Example:
An Independent Living client steals something and is arrested by police. b. A Notable Event may be unsupported threat or accusation made by a client during service or not-service hours.
Example:
A client is screaming that someone is hitting them when no one is in the room. c. Notable Event may be an injury sustained during service hours such as a cut or bruise that may need to be monitored but does not require immediate medical attention.
Examples:
A scratch or bruise from a fall that does not immediately incapacitate/affect the client.
A cut requiring a Band-Aid.
A bruise of unknown origin.
If a cut or bruise develops into a serious injury or happens repeatedly then it must be capture in an
Incident Report and notifications must be made. d. Notable Event may be a medical concern that is noted when a client at home or in independent living goes to their PCP or a hospital for a medical concern.
Example:
One of our parents takes their child to the doctor ’s office for twisted ankle from a fall at home/in the park. e. Protocol
Do not use an Incident Report form for Notable Events.
Record in the Daily Note (DSP) or Case Note (Case
Management).
Keep a dialog with Manager/Supervisor/Case Manager.
Incident Report Policy & Procedure Handout Last Revision: 2012/05/17 IR-002
2
‘
He-M 202.02 (o):
“Incident report” means a document used to inform management, supervisory staff, or any other appropriate staff of a program or facility of a serious injury or other event threatening the health or safety of individuals or staff.
’
Definitions/Type of Incidents - Reported
1. Injury a. A serious injury that requires professional medical treatment.
Medical professionals include but are not limited to MDs,
RNs, and LPNs.
An injury resulting in a hospitalization, fractures, broken bones and wounds requiring stitches or surgical glue.
Examples:
Swollen ankle,
Open cut/wound,
Client who can not walk or move other appendages/body parts
Head injury resulting from a fall or a physical altercation.
Seizures to be recorded on a Seizure Report unless there is a serious injury. b. Contact
Guardian
Nursing
Case Manager
2. Medical Concerns a. Treatment of ailments and other medical conditions by a medical professional based on:
Sudden physical changes in health including significant illness and/or repeat or chronic issues.
Exposure of eye, mouth, other mucous membrane, non-intact skin exposure to foreign blood, chemical or other infectious materials. b. Examples:
Choking
Rashes/ severe skin irritation
Shortness of breath/trouble breathing
Dizziness c. Contact
Guardian
Nursing
Case Manager
3. Other/Client Rights a. Any suspected client rights violation, including but not limited to abuse, neglect or exploitation. b. Contact
Bureau of Developmental Disabilities Hotline & BEAS
Guardian
Case Manager
Incident Report Policy & Procedure Handout Last Revision: 2013/06/05 IR-002
3
4. Other/Restraint a. Use of physical restraint or any physical actions necessary that may be atypical. b. Contact:
Guardian
Case Manager
5. OTHER/ Serious Crimes Committed by or against a Consumer during service hours. a. Theft b. Robbery c. Burglary d. Assault e. Sexual assault f. Fire setting g. Police involvement h. Contact
Must notify a member of The Moore Center Senior i. Manager Case Manger to fill out Sentinel Event Form.
6. Behavioral
Leadership team
Guardian
Nursing
Case Manager a. Actions that are atypical or unusual for that client. b. Verbal or physical aggression. c. Self injurious behavior. d. Absence with out supervision. e. Any actions that create physical safety concerns or property destruction. f. Use of sexual conduct or language. g. Examples:
Client leaves Day or Residential Services.
Acting out such as kicking, screaming, spitting, hitting self or others.
Client hits another client. h. Contact:
Contact Guardian
Case Manager
Nursing (if needed) i. Notes:
Only use initials when another client is the target of a behavioral incident.
A secondary Incident Report is not needed if the targeted client is not injured.
Incident Report Policy & Procedure Handout Last Revision: 2013/06/05 IR-002
4
7. Motor vehicle Accident a. Any accident that takes place in any personal, agency or vendor vehicle transporting a client regardless of any injury or damage. b. Contact:
Guardian
Case Manager
Nursing c. Incident Report must be completed for each client. d. MCS Staff must contact HR to fill out “Injury Accident Form”. e. Vendors to follow vendor agency processes.
8. Death of a client a. Contact:
Must notify a member of Senior Leadership Team
Case Manager b. Case Manager
Notify BDS within 12 hrs.
Complete Mortality Report and Sentinel Event Form (within
24 hrs. when necessary).
Both to be reviewed by Maureen Rose Julian.
9. Additional Examples for an Incident Report: a. A client is in 24/7 services but is allotted 3 hours of unsupervised time.
An incident occurs during the unsupervised time.
Must document using an Incident Report. b. A client is placed at job site through The Moore Center Employment
Services and is hit by a fellow employee.
Must document using an Incident Report.
Call Client Rights Hotline at BDS & BEAS.
Incidents
1. If you have witnessed, discovered or were involved in an incident during service hours. a. Ensure the safety of the client and/or other individuals. b. Call 911 if necessary. c. Call nursing if necessary. d. Texting is not authorized. e. Email may not be used to communicate with the Guardian unless stated in the Electronic Communication Authorization form found in the client’s record. f. Contact your Supervisor. g. Contact Case Manager immediately
Required by state regulations.
If Case Management has an Out of Office Message contact the next appropriate individual as directed by that message. h. Notify other appropriate individuals. i. Fill out the Incident Report form provided by The Moore Center.
Incident Report Policy & Procedure Handout Last Revision: 2013/06/05 IR-002
5
Notification
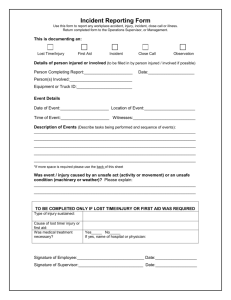
1. Incident Report form a. All fields must be completed without error;
First Name & Last Initial Client Code
Date of incident Time of incident
Location of incident
Department
Agency
Check off Emergency Response b. Fact/Response/Results
Limited to five (5) lines of text only; do not use additional paper.
Recount facts only.
Keep it clear and concise.
Example: Andrew slipped on the ice and fell. He has a deep cut on his forehead above the eye. He was taken to CMC emergency room and received eight stitches. c. Complete Notification section
Texting is not authorized.
Email may not be used to communicate with the Guardian unless consented in the Electronic Communication
Authorization form found in the client’s record. d. Review the Incident Report form with your Supervisor. e. Staff and Supervisor are required to sign and date the report. f. Vendors and The Moore Center Programs to submit Incident Report to The Moore Center;
Within 24 hrs. as required by state regulations.
Send to The Moore Center’s Health Information Management
Department
Must be in an envelope and clearly marked:
Lisa Collins/Incident Report
Via email
The Incident Report must be scanned and encrypted prior to being sent via email.
Password: Region07
Email address: lisa.collins@moorecenter.org
The Moore Center Providers will continue to send Incident
Reports into the Residential Department for supervisory review and signature prior to being sent to Lisa Collins (HIM).
Questions
1. If you have questions please contact: a. Cindy Pinder at cindy.pinder@moorecenter.org
Incident Report Policy & Procedure Handout Last Revision: 2013/06/05 IR-002
6
Case Management Incident Follow Up
1. Notable Events should be written in the monthly Case Note.
2. Case Management Incident Follow Up form; a. Completed by Moore Center Case Management Only. b. Follow up to be completed thirty (30) days from the date of the incident;
Allow enough time for
Complications;
Additional doctors visits;
Possible client rights complaint.
3. Research the incident a. Do not make assumptions – case note must be based on information that is known to be accurate and complete. b. Determine the cause(s);
Look for underlying causes as well as the obvious (e.g. lack of training; under staffing; new staff; health issues). c. Ask open-ended questions that cannot be answered by simply "yes" or "no".
Where were you and the client at the time of the incident?
What were you and the client doing at the time?
Were there distractions?
Was the activity routine or something the client has not done before or does infrequently?
What did you see, hear?
What were the environmental conditions (weather, light, noise, etc.) at the time?
Has similar/less significant incidents happened before? d.
Capture any actions taken to ensure the client’s or community’s safety.
4. Ensure all reasonable steps are taken to prevent a similar incident recurring in the future.
5. Review with your Supervisor.
6. Email the Case Management Incident Follow Up form to Cindy Pinder
(Maureen Rose Julian
’s office). a. Remember to use only the Client’s First Name and Last Initial when completing the form.
7. Send original to the HIM Department.
Questions
1. If you have questions please contact: a. Cindy Pinder at cindy.pinder@moorecenter.org
Incident Report Policy & Procedure Handout Last Revision: 2013/06/05 IR-002