supplier or reagent - McMaster University
advertisement

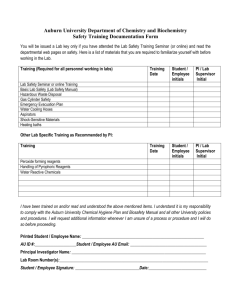
“biosafety update 2009” consists of the powerpoint presentations: “Good Culture Practices” and “Misidentification and Contamination” with their respective quizzes Biosafety training starting in Jan 2009 will consist of the in class session (offered monthly) PLUS these two presentations. All three quizzes are to be handed in at the same time – within a week or so after the in class session. 1 Good Culture Practices self paced Powerpoint study McMaster University Biosafety Office please print off the quiz or obtain copy from HSC 3N1C and return or fax to 905 528 8539 2 guiding principles of good cell culture EU (2-7) why worry? (NIH) (8-11) information / SOP’s (12-14) keep records (15-23) good culture techniques (24 – 32) risk of contamination (33 – 39) test cells regularly (40 – 43) contact us & training (44) 3 Guiding principles for Good Cell Culture Practice (EU) 1. understand the in vitro culture system you are using and the relevant factors that could affect it 2. document assurance of the quality of all materials and methods 3. document information to track materials and permit repetition of the work. 4 4. use measures to protect individuals and the environment from potential hazards 5. comply with laws, regulations and ethics 6. provide education and training to achieve good cell culture practice 5 why practice quality assurance and good culture practices? “the maintenance of high standards is fundamental to all good scientific research” to maintain a reliable/reproducible program to detect problems to respond quickly when they occur to prevent reporting erroneous results 6 goal of Good Culture Practices training program to improve the knowledge of basic biological culture practices to improve the likelihood that contamination will be detected/reduced to ensure that the intended cultures are used in experiments 7 why are we worried about cell line or culture contamination? 1) studies have shown that 20-35% of all cell lines are contaminated (HeLa cells in many cases) some cell lines have a short doubling time and are a high risk for cross contamination into other cell lines. 8 2) research results may not be accurate if you are using a contaminated cell line NIH has stated that “misidentification of cell cultures is a serious problem” (Nov 2007) please read these three articles: “Cases of mistaken identity”, “Cell line cross contamination” and “Open letter on cell line identification” http://fhs.mcmaster.ca/safetyoffice/biosafety_cell_line.html 9 3) authentication of cultures may be a future requirement for peer reviewed processes (grants and publishing) “NIH notice on authentication of cell lines” http://fhs.mcmaster.ca/safetyoffice/biosafety_cell_line.html 10 4) PI’s are responsible for the accuracy and purity of the cultures used in their research - what detailed protocols/ practices are in place in your lab in the form of a manual and SOP’s? - take this quiz to see how many of the recommended practices are currently in use in your lab (web link not yet ready) - visit a excellent McMaster research lab manual at www.dwalab.com/labman for an example 11 typical SOP’s for a culture lab • standards for the quality of culture vessels and surface coatings • sterility check for re-used items • maintenance and sterility check for automatic pipettes and pipettors • maintenance and sterility check for incubators • standards for culture reagents • Visit an excellent McMaster research lab manual at www.dwalab.com/labman as an example 12 Checking cell viability and count in practice: learn how to do it at www.jove.com “basic protocols” good microscopy for good results in practice: learn how to do it at www.jove.com “basic protocols” good freezing and recovery techniques are important for healthy cells in practice: learn how to do it at www.jove.com “basic protocols” 13 when starting with a new line/strain know the following: • • • • • • • • authenticity morphological appearance viability growth rate passage number differentiation state contaminates present (or not) appropriate +/- controls for the application 14 protocols to reduce the risk of contamination / misidentification A) keep excellent records B) use good culture techniques C) test cultured lines regularly 15 A) keep excellent records 1) obtain validated cell lines only from a reputable source in practice: do not rely solely on verbal assurances for the identity of a cell line in practice: have a documented provenance of the cell line, the genotypic and phenotypic characteristics in practice: consider purchasing new cell lines rather than getting them from the “lab next door” 16 2) keep real time paperwork/inventories on cultures in practice: several inventory options will record similar information, depending on the nature of your work in practice: this will allow for tracking of lines and who has used them, and how all material has been used www.fhs.mcmaster.ca/safetyoffice/biological_inventory.html 17 sample inventory forms any of these forms or equivalent can be used www.fhs.mcmaster.ca/safetyoffice/biological_inventory.html 18 3) have a standard coding and recording system in the lab for storage of frozen lines in practice: keep a location log book and ensure everyone uses it in practice: have a documented monitoring system for liquid nitrogen refilling procedures 19 4) do not use any cells/strain with questionable labeling in practice: if it is no longer readable, discard it, in practice: if it is not in the logbook, discard it. in practice: if the entry in the logbook does not match the label on the vial, discard it. 20 5) label vials in advance when freezing or subculturing in practice: pre label all vials for freezing and freeze only one cell line at a time. learn about freezing cells at www.jove.com “basic protocols” in practice: fill no vials or culture flasks without pre labeling 21 6) compare the label on the thawed vial with the label on the growth chamber before making the transfer. 22 B) good culture technique 1) check and record that all reagents have been tested for sterility in practice: a central facility should keep records of all sterility checks in practice: incubate an uninoculated growth medium with all reagents as a blank if there is no central prep facility 23 2) do not use the same reagent bottle (eg media) for different cell/strain lines in practice: do not share reagents among operators in practice: it would be ideal to label each reagent bottle for the cell line it is to be used for 24 3) always change pipets between reagents/cell lines and plug all pipets in practice: the plugged pipet decreases the chance that contamination can enter into the pipetting unit. in practice: if liquid enters the pipetting unit, change the HEPA filter nose piece unit 25 4) work with only one cell/strain line at a time in practice: finish all work with one line before moving on to another, this significantly reduces the chance of cross contamination 26 5) put media and reagents into flask, add cells last in practice: this prevents a cell contaminated pipet entering into the stock media and contaminating it. 27 6) handle rapidly growing cells at the end of the work session (eg HeLa) in practice: the cells are not available to contaminate slower growing lines used earlier in the work session 28 7) newly isolated lines to be characterized as soon as possible in practice: the information garnered at this step will serve as the identification tests for the future as finite cell lines may change characteristics over time In practice: avoid subjecting cells to fluctuating temperatures or culture conditions as it may cause cells to alter 29 8) quarantine all new cell/strain lines until they are shown to be not contaminated in practice: isolate new cells so that there will be no opportunity for incubator cross contamination. eg. use filtered flasks 30 9) re-evaluate your sterile technique regularly in practice: institute regular sterility checks for all aspects of your culture eg. all reagents except cell lines in culture eg. plates in incubator eg. swabs of pipeter and surface of biological cabinet 31 Conditions that increase the risk of contamination 1) new - staff or student in practice: individuals are most likely to have an incident in the first three months of working. - supplier or reagent, In practice: quality control any new reagents before placing them into general use or buy from a reputable source - equipment in practice: decontaminate and evaluate all new equipment 32 2) deteriorating conditions in practice: aseptic technique is not followed in practice: attention to detail is no longer followed in practice: quality of lab air has changed due to local sanitary conditions or external environmental conditions (eg increased fungal spore count) 33 3) poor cleaning in practice: protocols not followed or not available in a written format eg. biohood decon in practice: disinfectant not effective against the agent being cultured in practice: outdated disinfectant will be ineffective, therefore, date all disinfectants on the date of preparation eg. 10% bleach has a life span of several hours in practice: gloves not sufficiently sterilized before use 34 4) autoclave - lack of control in practice: all individuals using an autoclave must receive autoclave training in practice: quality control for autoclaves requires regular use of a biological indicator, with records in practice: there should be an understanding of appropriate packaging/loading for autoclaving in practice: the steam for autoclaves should be quality controlled. 35 5) dirty equipment in practice: pipet tissue culture nose piece filters are to be inspected regularly in practice: incubator and water source and centrifuge need to be decontaminated regularly in practice: cold/ warm rooms need to be cleaned regularly in practice: lab coats need a regular schedule of cleaning, not just when they “look dirty” 36 6) lab conditions in practice: increased general activity in lab will increase risk of contamination in practice: construction activity (ie on ductwork) may release contaminant spores in practice: increase in lab air currents are likely to affect the biological cabinet air curtain 37 7) biological cabinet in practice: blocking either front or back grill will increase contamination in practice: all biological cabinets should be certified annually in practice: two people working in one hood causes too much disruption for good culture practices 38 C) test cultures regularly 1) every time a culture is handled - check by eye for contamination - check by phase contrast microscopy in practice: learn at www.jove.com “basic protocols” 39 2) on regular intervals - run a culture without antibiotics to reveal contamination that may exist in the stock line, know what you are dealing with - if possible, use no antibiotics in culture 40 3) test cell regularly in an appropriate assay in practice: do the on–line biosafety training part 2 41 4) run positive and negative controls and do not ignore unexpected results. in practice: consider human error in practice: consider all reagents and equipment which have been in contact with the culture. assume nothing. in practice: consider that the cell line is not what you expect it to be 42 visit our biosafety website at fhs.mcmaster.ca/safetyoffice for 2009 1) “biosafety update 2009” consists of “Good Culture Practices” and “Misidentification and Contamination” and the quiz 2) “initial biosafety training” from now on will consist of the in class session offered monthly PLUS these two presentations 43