UNIT_2PART2
advertisement
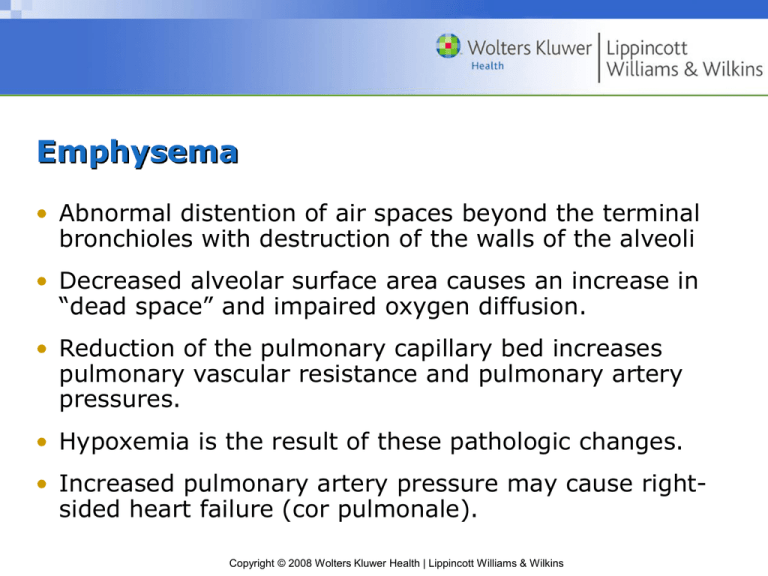
Emphysema • Abnormal distention of air spaces beyond the terminal bronchioles with destruction of the walls of the alveoli • Decreased alveolar surface area causes an increase in “dead space” and impaired oxygen diffusion. • Reduction of the pulmonary capillary bed increases pulmonary vascular resistance and pulmonary artery pressures. • Hypoxemia is the result of these pathologic changes. • Increased pulmonary artery pressure may cause rightsided heart failure (cor pulmonale). Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Changes in Alveolar Structure with Emphysema Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Normal Chest Wall and Chest Wall Changes with Emphysema Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Typical Posture of a Person with COPD Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Risk Factors for COPD • Tobacco smoke causes 80-90% of COPD cases! • Passive smoking • Occupational exposure • Ambient air pollution • Genetic abnormalities – Alpha1-antitrypsin Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Pathophysiology of COPD • Airflow limitation is progressive and is associated with abnormal inflammatory response of the lungs to noxious agents. • Inflammatory response occurs throughout the airways, lung parenchyma, and pulmonary vasculature. • Scar tissue and narrowing occur in airways. • Substances activated by chronic inflammation damage the parenchyma. • Inflammatory response causes changes in pulmonary vasculature. Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Nursing Process: The Care of Patients with COPD: Assessment • Health history • Inspection and exam findings • See Chart 24-2 and Chart 24-3 • Review of diagnostic tests Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Nursing Process: The Care of Patients with COPD: Diagnosis • Impaired gas exchange • Impaired airway clearance • Ineffective breathing pattern • Activity intolerance • Deficient knowledge • Ineffective coping Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Collaborative Problems • Respiratory insufficiency or failure • Atelectasis • Pulmonary infection • Pneumonia • Pneumothorax • Pulmonary hypertension Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Nursing Process: The Care of Patients with COPD: Planning • Smoking cessation • Improved activity tolerance • Maximal self-management • Improved coping ability • Adherence to therapeutic regimen and home care • Absence of complications Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Improving Gas Exchange • Proper administration of bronchodilators and corticosteroids • Reduction of pulmonary irritants • Directed coughing, “huff” coughing • Chest physiotherapy • Breathing exercises to reduce air trapping – Diaphragmatic breathing – Pursed-lip breathing • Use of supplemental oxygen Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Improving Activity Tolerance • Focus on rehabilitation activities to improve ADLs and promote independence. • Pacing of activities • Exercise training • Walking aids • Use a collaborative approach. Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Other Interventions • Set realistic goals. • Avoid extreme temperatures. • Enhance coping strategies. • Monitor for and manage potential complications. Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Patient Teaching • Disease process • Medications • Procedures • When and how to seek help • Prevention of infections • Avoidance of irritants; indoor and outdoor pollution and occupational exposure • Lifestyle changes, including cessation of smoking Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Question COPD is the ____ leading cause of death in the United States. a.First b.Second c. Third d.Fourth Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Chronic Bronchitis • The presence of a cough and sputum production for at least 3 months in each of 2 consecutive years • Irritation of airways results in inflammation and hypersecretion of mucus. • Mucus-secreting glands and goblet cells increase in number. • Ciliary function is reduced, bronchial walls thicken, bronchial airways narrow, and mucus may plug airways. • Alveoli become damaged and fibrosed, and alveolar macrophage function diminishes. • The patient is more susceptible to respiratory infections. Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Pathophysiology of Chronic Bronchitis Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Asthma • A chronic inflammatory disease of the airways that causes hyperresponsiveness, mucosal edema, and mucus production • Inflammation leads to cough, chest tightness, wheezing, and dyspnea. • The most common chronic disease of childhood • Can occur at any age • Allergy is the strongest predisposing factor. Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Pathophysiology of Asthma Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Medications Used for Asthma • Quick-relief medications See Table 24-2 – Beta2-adrenergic agonists – Anticholinergics • Long-acting medications See Table 24-4 – Corticosteroids – Long-acting beta2-adrenergic agonists – Leukotriene modifiers Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Question Which of the following is a methylxanthine bronchodilator? a. Aminophylline b. Atrovent c. Maxair d. Proventil Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Examples of Metered-Dose Inhalers and Spacers Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Patient Teaching • The nature of asthma as a chronic inflammatory disease • Definition of inflammation and bronchoconstriction • Purpose and action of each medication • Identification of triggers and how to avoid them • Proper inhalation techniques • How to perform peak flow monitoring • How to implement an action plan • When and how to seek assistance Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Using a Peak Flow Meter Copyright © 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins