Isolation and Identification of Streptococci and Enterococci
advertisement

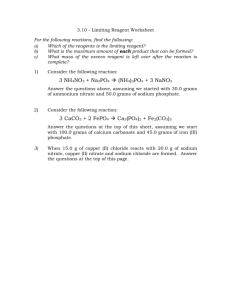
Isolation and Identification of Streptococci and Enterococci GENERAL DISCUSSION The streptococci are gram-positive cocci (0.5-1.0µm in diameter) which occur in pairs and chains of varying length. They are usually classified based on their hemolytic properties on blood agar and according to their serologic groups ( Lancefield grouping). The streptococci are usually isolated on Sheep Blood agar ( BAP) ( Tryptic soy agar with ( 5-10 ) % Sheep blood ). Hemolysis refers to is the lysis of the red blood cells in the agar surrounding bacterial colonies and is a result of bacterial enzymes called hemolysins. Reactions on blood agar are said to be beta, alpha, gamma, or double-zone: Hemolysis on sheep blood agar: Beta hemolysis refers to a clear, colorless zone surrounding the colony, where a complete lysis of the red blood cells by the hemolysins has occurred. Alpha hemolysis appears as a zone of partial hemolysis surrounding the colony, often accompanied by a greenish or brown discoloration due to oxidation of hemoglobin to met-hemoglobin by hydrogen peroxide Gamma hemolysis refers to no hemolysis or discoloration of the agar surrounding the colony. Double-zone hemolysis refers to both a beta and an alpha zone of hemolysis surrounding the colony. Gram positive cocci Gram Stain Gram Positive cocci Catalase - + Staphylococci Micrococci streptococci Growing on sheep blood agar ( hemolysis ) α S. Pneumoniae S. viridans β S.agalactiae S. pyogenes γ Enterococcus spp. (E. faecalis) Non Enterococcus (S.bovis) Serological Typing of Streptococci ( Precipitin test ) Many of the streptococci can be placed into serological groups called Lancefield groups based on carbohydrate antigens in their cell wall. Although there are 20 different Lancefield groups of streptococci, the groups A, B, C, D, F, and G are the ones usually associated with human infections. The Slidex Strepto-Kit® system is a commercial kit for typing the 6 Lancefield groups of streptococci that commonly infect humans. To make the reaction more visible, since the antigens for which one is testing are only fragments of the bacterial cell wall, the known monoclonal antibodies have been adsorbed to latex particles. In this way, when the known monoclonal antibodies react with the streptococcal cell wall antigens, agglutination of the latex particles will occur and can be easily seen with the naked eye. Dr. rebecca lancefield L L Antibody S S S L S Fc L L L L S S L=Latex particle Strepto. antigen Gram Stain Gram Positive cocci Catalase - + Staphylococci Micrococci Streptococci Lancefeild grouping ( A,B and D ) ــــــ S. Pneumoniae S. viridans A S. Pyogenes (GAS) B S.agalactiae (GBS) D Enterococcus spp. (E. faecalis) Non Enterococcus (S.bovis) β-hemolytic Sterptococci S.agalactiae S. pyogenes Bacitracin Sensitivity Test: Definitive test to differentiate between S. pyogenes & Non group A β-hemolytic Streptococci ( S. agalactiae ) Principle: A low conc. of Bacitracin (0.04 units) will selectively inhibit the growth of S.pyogenes giving a zone of inhibition around the disc. Bacitracin Sensitivity Test: Procedure: 1. Inoculate blood agar plate with the test organism. 2. Aseptically apply Bacitracin disc onto the center of the streaked area. 3. Incubate the plate at 37oC for 24 hrs. B Bacitracin Sensitivity Test: Results: Positive test: any zone of inhibition around the disc. B Bacitracin Resistant S.agalactiae B Bacitracin Sensitive S.pyogenes Bacitracin Sensitivity Test: Pyrrolidonyl-beta-naphthylamide (PYR) test S.pyogenes posses the enzyme L-pyroglutamyl aminopeptidase which hydrolyzes Pyrrolidonyl-beta-naphthylamide with the formation of free β- naphthylamine, which combines with cinnamaldehyde reagent to form a bright- red end product. Method : Rub a small amount of a colony to be tested on a surface of a filter paper impregnated with PYR ( available commercially ). Add one drop of freshly reconstituted detector reagent N,N- dimethylaminocinnamaldehyde, with detergent ( available commercially), and observe for a red color within 5 minutes. Hippurate hydrolasis test: Group B streptococci contain the enzyme hippuricase , which can hydrolyze hippuric acid . Other β streptococci lack this enzyme . The production pf hippuricase results in the hydrolysis of sodium hippurate With the formation of sodium benzoate and glycine . The hydrolysis of hippurate can be detected by one of two methods: Standard test for benzoate using ferric chloride Rapid test for glycine using ninhydrin reagent Standard test for benzoate using ferric chloride Media and reagent: Sodium hippurate medium Brain Heart infusion broth. 1% Sodium hippurate. Ferric chloride reagent Fecl3 12g. 2% aqueous HCl 100 ml. Procedure : Incubate a tube of sodium hippurate medium with the organism. Incubate for 20 hours or longer at 37 OC. Centrifuge the medium to pack the cells and pipette 0.8 ml of the clear supernatant in to a clean test tube. Add 0.2 ml of the ferric chloride reagent and mix. Result: A heavy precipitate will for upon addition of Fecl3 reagent. Rapid test for glycine using ninhydrin reagent Media and reagent: Sodium hippurate medium 1% Sodium hippurate. Distilled water. Ninhydrin reagent Ninhydrin 3.5 g. 1: 1 Acetone/butanol 100 ml. Procedure : Incubate a large loop of a β streptococci culture in to 0.4 ml of the sodium hippurate medium and incubate for 2 hours at 37 OC. Add 0.2 ml of the ninhydrin reagent. Result: The presence of a deep purple color after the adition of ninhydrin reagent within 10 minutes indicate the presence of glycine. CAMP test : The laboratory identification of group B beta hemolytic Streptococci has been simplified implementation of the CAMP test, which is easy perform and well within the capabilities of small laboratories. The CAMP phenomenon was first reported in 1944 by Cristie, Atkins, and Munch-Peterson, whose contribution is acknowledged in the acronym Principle: The hemolytic activity of Staphylococcal beta –lysin on erythrocytes is enhanced by an extracellular factor produced by group B streptococci, called the CAMP factor. Therefore, where the two reactants overlap in a sheep blood agar plate, accentuation of the beta hemolytic reaction occurs. Media and reagent: Sheep or bovin blood agar must be used. Procedure: The CAMP test is performed by making a single streak of the beta hemolytic Streptococcus perpendicular to a strain of Staphylococcus aureus that is known to produce beta-lysin . The two streak lines must not touch one another then incubate the agar in to candle jar to accelerate the hemolysis. Results: The zone of increased lysis assumes the shape of an arrow-head at the junction of the two streak lines. CAMP test : S.agalactiae Beta-hemolytic Staphylococcus aureus Beta hemolytic Streptococci not S.agalactiae α-hemolytic Sterptococci S.pneumoniae S. viridans Optochin Sensitivity Test: Definitive test to differentiate between S. pneumoniae & viridans Streptococci Principle: S.pneumoniae is inhibited by less than 5 µg/ml Optochin reagent (ethylhydroxycupreine hydrochloride ) giving a zone of inhibition. Optochin Sensitivity Test: Procedure: 1. Inoculate blood agar plate with the test organism. 2. Aseptically apply Optochin disc onto the center of the streaked area. 3. Incubate the plate at 37oC for 24 hrs. 4. Accurately measure the diameter of the inhibition zone around the disc. O Optochin Sensitivity Test: Results: Sensitive with inhibition zone equal or more than 14 mm when disk with diameter equal 6 mm or 16 when 10 mm disk is used. Bile solubility test The bile solubility test is used to determine the ability of bacterial cells to lyse in the presence of bile salts, within a specified time . S. pneumoniae possesses an autolytic enzyme which lyses the cell’s own wall during division. The addition of bile salts (sodium deoxycholate) activates the autolytic enzyme and the organisms rapidly autolyse. Other α haemolytic streptococci do not possess such an active system and therefore do not dissolve in bile. The bile solubility can be detected by one of two methods: Broth test. Agar blate test. Bile solubility Broth test : Media and reagent: 10% sodium deoxycholate or 10% sodium taurocholate. Pure culture ( broth ) of the tested organism incubate at 37 OC for 24 hours. Sterile normal saline. Test tubes. Procedure : Transfer approximately 0.5 ml of an 24 hours broth culture to each of two test tubes Add 0.5 ml of 10% sodium deoxycholate to one of the two test tubes ( marked test) Add 0.5 ml of sterile normal saline to the second test tube ( marked control ) Gently agitate broth test tubes and palce them in a 37 OC incubator or water bath for 3 hours, checking hourly. Result: Bile soluble, visible clearing of the turbid culture within 3 hours. The saline control tube should remain turbid. Bile solubility Agar test : Media and reagent: 2% sodium deoxycholate. Isolated colonies of the tested organism on agar incubate at 37 OC for 24 hours. Procedure : To well isolated colony of the test organism on 5% sheep blood agar plate, add a drop of 2% sodium deoxycholate without inverted the blate incubate in 37 OC incubator for 30 minutes. Result: Bile solublecolony dissapear leaving hemolyzed area. Colony insoluble in bile remain intact. Quellung Reaction Around the turn of the century (1900) German physician and bacteriologist Friedrich Neufeld discovered that antibodies against specific pneumococcal capsular antigens could be produced and used for typing Streptococcus pneumoniae organisms. These antibodies, when bound to the cell wall antigen produced a clearing around each individual cell with the appearance of the capsule having swollen. The word “Quellung” is German for ‘swelling’ however this is a misnomer as the capsule does not swell but simply appears enlarged with the clear zone produced by the bound antibodies. The clearing is best visualized by using a stain to enhance contrast between the clear zone of bound antibody and the surrounding material. Procedure: Colony isolate, is placed on a clean microscope slide and allowed to dry. A drop of *Polyvalent Quellung antisera is applied to the slide and mixed with a drop of methyene blue stain. A coverslip is place onto the mixture and allowed to incubate/react at room temperature for 15-20 minutes. The slide is then examined under the microscope for distinct clearing around the cells. One may have to search for a microscopic field which best shows the clearing. A distinct zone of clearing indicates a positive Quellung reaction and confirms the identification as Streptococcus pneumoniae. *Polyvalent Antisera- contains all known serotypes to identify any pneumococcus. Specific or individual antisera can be employed for scientific study of individual serotypes. Quellung Reaction Fluorescent antibody (FA) staining Streptococcus pneumoniae, FA stain showing its antiphagocytic capsule (CDC). Streptococcus faecalis broth (SF broth) : Media and reagent: Tryptone D-glucose Monopotassium phosphate Dipotassium phosphate Sodium azide Sodium chloride Bromocresol purple pH= 6.9 Principle: The tryptone and dextrose supply the nutrients required for the growth of enterococci. Sodium azide exhibits a bacteriostatic effect on gram-negative bacteria through its inhibitory action on enzymes in the electron transport system. Bromcresol purple serves as a pH indicator. Bile esculin test : Media and reagent: Beef Extract. Peptone. Esculin. Oxgall ( 1- 4 )%. * sodium azide. Ferric Ammonium Citrate. Agar 1.5% Final pH: 6.6 ± 0.2 at 25 OC Principle: Enterococci and certain streptococci hydrolyze the glycoside esculin to esculetin and dextrose. Esculetin reacts with an iron salt to form a dark brown or black complex. Ferric citrate is incorporated into the medium as an indicator of esculin hydrolysis and resulting esculetin formation. Oxgall is used to inhibit gram-positive bacteria other than Enterococci. Bile esculin test : Positive result Negative result 6.5% NaCl medium Enterococcus spp. Grow well in 6.5% NaCl medium(6.5%NaCl in brain heart infusion broth ) but S.bovis will not. Negative after 24hrs S.bovis Positive after 24hrs Enterococcus spp. Pyrrolidonyl-beta-naphthylamide (PYR) test Enterococcus spp. Posses the enzyme L-pyroglutamyl aminopeptidase which hydrolyzes Pyrrolidonyl-beta-naphthylamide with the formation of free β- naphthylamine, which combines with cinnamaldehyde reagent to form a bright- red end product. Method : Rub a small amount of a colony to be tested on a surface of a filter paper impregnated with PYR ( available commercially ). Add one drop of freshly reconstituted detector reagent N,N- dimethylaminocinnamaldehyde, with detergent ( available commercially), and observe for a red color within 5 minutes.