Chronic Obstructive Pulmonary Disease (COPD)
advertisement

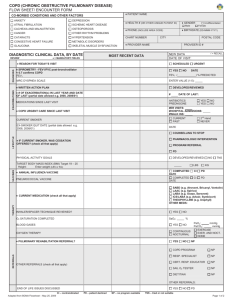
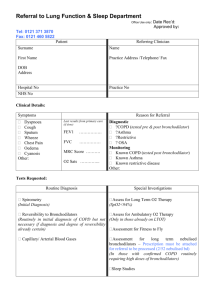
Chronic Obstructive Pulmonary Disease (COPD) • COPD is characterized by : **Chronic airflow obstruction & accelerated loss of lung function which is progressive & NOT fully reversible. ** COPD is preventable & treatable but NOT curable. **In COPD, airway obstruction is fixed & irreversible w/ different degrees of reversibility according to patients. • COPD is assoc. w/ abnormal response to noxious chemicals or gases. • Most common risk factor for COPD is SMOKING • COPD pts. experience: -productive cough -dyspnea **See table2 p.920 for comparative table b/w asthma & COPD • General Goals of Management of COPD: 1) Prevent or slow disease progression. 2) Relieve symptoms. 3) Improve exercise tolerance. 4) Improve overall health status. 5) Prevent & treat complications. 6) Prevent & treat exacerbations. 7) Decrease mortality. • 2 Major Forms of COPD: 1) Chronic Bronchitis (C.B.) 2) Emphysema 1) Chronic Bronchitis (C.B.): Defined clinically as chronic excessive secretion into bronchial tree occurring most days during a period of @ least 3 months /yr for @ least 2 consecutive yrs. 2) Emphysema: Defined anatomically as abnormal permanent enlargement of the alveoli distal to terminal bronchioles accompanied by destruction of their walls without fibrosis. • Both C.B.& emphysema are : 1) Indistinguishable. 2) Have different risk factors. 3) Have similar management strategies. ** Although Asthma & COPD are both characterized by airflow obstruction, their pathophysiologic features & response to treatment are different. • Etiology: *Smoking is major risk factor for COPD. • About 80-90% of COPD pts. have a history of current or past smoking although only 15-20% of smokers develop COPD due to genetic variation. • Other R.F. include: 1. Environmental factors(pollution&occupational) 2. Recurrent pulm. infections in childhood. 3. α₁ antitrypsin deficiency: Rare & inherited (<1% of emphysema cases) • Exacerbations of COPD typically have an infectious etiology, either viral or bacterial. • During an exacerbation, there is: 1) Increased S/S 2) Increased mucus production 3) Worsening of gas exchange 4) Worsening of airway obstruction assoc. w/ an increased risk of resp. failure. • Clinical Presentation & Diagnosis: • Clinical assessment of COPD pts. includes: 1) Medical history 2) Physical examination • Diagnosis of COPD is considered w/complaints of: *Chronic cough *Dyspnea *Sputum production * + History of risk factors • Signs & Symptoms: • Pathophysiologic changes progress over yrs. & clinical symptoms occur later. • By time pt. seeks med. help, disease is far advanced. • Sig. overlap b/w clinical presentation of C.B. & Dyspnea. Productive cough is assoc. more w/ C.B. • Dyspnea is more assoc. w/ Emphysema. • Obesity is assoc. w/ C.B. (Blue bloaters) • Wt. loss is assoc. w/ Dyspnea (Pink puffers) • Gold standard for COPD diagnosis is spirometry: FEV1/FVC < 70% • When SABA is administered & spirometry is repeated in 15-30 min.: -COPD is typically characterized by < 12% improvement in FEV1 (or <200ml in pts w/ very low lung volumes). - A large increase in FEV1 is more consistent w/ asthma. • COPD progression may develop acute & chronic complications, i.e.: 1)Pulm. HTN 2)Cor Pulmonale & Rt. CHF ( Blue Bloaters ) 3)Polycythemia 4)Hypoxemia & resp. acidosis 5)Emphysematous (Pink Puffers) • An individualized approach to therapy should be: 1) Appropriate 2) Based on the severity classification 3) Patient’s risk factors • Important initial intervention: to reduce or eliminate exposure to risk factors. • Smoking cessation: the only treatment strategy proven to slow the chronic progressive loss of lung function. • Approaches to Treatment: • Pharmacotherapy: • None of the currently available therapies is shown to prevent or slow progressive loss of lung function. • 1⁰ role : symptomatic relief • 1⁰ strategy: using bronchodilators. • Response to meds. : Different among pts. • Assessment of response & S/Es (table35.8 p.926) • Reversibility of airflow limitation through spirometry (FEV1) : Not shown in many pts. • Dyspnea : Major debilitating symptoms for advanced dz. pts. • Inhaled route of adm.(MDI, DPI, Neb.): -Pref. because > effective, faster onset & safer than oral. -All inhaled mechanisms are equally effective in chronic management. -MDI & DPI: > convenient -Nebulizer: initial treatment in exacerbation. *Bronchodilator combination used for additive benefits & reduced S/Es. 1) Bronchodilaters: A. Beta-2 Agonists: -SABA -LABA B. Anticholinergics: -SA Ach -LA Ach C. Methylxanthines I. Bronchodilators: A) Beta-2 Agonists: Examples of SABA: -Albuterol -Pirbterol -Terbutaline *Albuterol:- Most commonly used inhaled SABA. - < 5 min OA -Relativ. short DA ( 4̴ hrs.w/chronic use) *In COPD, SABA: -Relieves symptoms -Improves exercise tolerance -No sig. lung function improvement Examples of LABA: ( DA 1̴ 2hrs) -Formoterol (OA ̴ 5min., pk. ̴ 30min.) -Salmeterol ( OA ̴ 15min., pk. ̴ 1-2 hrs.) Difference NOT important clinically *Sig. advantage of LABA over SABA *Considered for those NOT controlled w/ SABA • For more frequent or chronic symptoms, long acting bronchodilators (LABA, LA Ach.) are more effective in: 1. Improving lung function 2. Improving exercise tolerance 3. Improving quality of life 4. Reducing frequency of exacerbations B) Anticholinergics: 1) Short Acting: Ipratropium Br.: (by inhalation) * ≥ bronchodilation than SABA @usual doses. *Little systemic absorption. *OA within 15 min., DA 4-6 hrs. *@ max. doses bronchodilation by beta-2 agonists maybe = to that of ipratropium in COPD but S/Es are more common w/SABA. *Due to slower OA, SABA may be preferred for acute bronchospasm w/ ipratropium used on scheduled basis. *Given as 2 inhalations QID increased to 6 inh. if needed. 2) Long Acting: Tiotropium: *Once daily dosing regimen. *Comparing Tiotropium w/Ipratropium in COPD: 1.Tiotrop. used QD, Ipratrop. used QID. 2. < Multiple exacerbations w/ Tiotrop. 3. Sig. longer time to 1st exacerbation w/Tiotrop. 4. For most outcomes, Tiotrop.> effective than Ipratrop. but > expensive. • Studies did NOT show significant clinical difference between LABA & Tiotropium in COPD management. • Short- acting bronchodilators (Albuterol + Ipratropium) combination increase effectiveness & as per treatment guidelines are commonly used in the management of Mild-Mod. COPD. • Limited data are available on the use of Long-Acting Bronchodilators combination, however, (LABA + Tiotropium) combinations are used for severe COPD patients. C) Methylxanthines: • Theophylline is currently considered a 3rd- line agent in the management of COPD due to the availability of safer & more potent therapies & its risk of toxicities. • Issues to be considered with the use of Theoph.: 1) Different dosage forms &salts of theoph. are available.(SR QD or BID are most appropriate) 2) Significant variability in bioavail. between different products & patients. 3) Recommended therapeutic range for COPD 8-12ug/ml. 4) Smoking , other drugs, & disease factors interact w/ theoph. Careful monitoring of serum theoph. conc. is important. 5) Sig. S/E profile involves: GI, CNS, CV. • Summary of Bronchodilator Therapy: 1) Bronchodilators are the mainstay of therapy for chronic COPD management. 2) Inhaled form preferred over systemic. 3) Short-acting agents are used initially. 4) If symptoms continue, LA agents are >effective & convenient: Different trials showed long-acting bronchodilators (LABA & LA Ach) provided > benefit in improving different outcome measures than Short-Acting agents (SABA & SA Ach). 5) Bronchodilator combinations are commonly used with added benefit & reduced S/Es from higher doses of a single agent. 6) Oral theoph. Is an option reserved for those NOT responding to inhaled regimens or refuse to use inhaled meds. II. Corticosteroids: • Did NOT result in dramatic response (unlike in asthma) which may be due to neutrophilic nature of COPD. • Systemic corticosteroid should be avoided in chronic COPD due to its lack of benefit & serious toxicity. • ICS has superior safety over systemic. • Current Guidelines suggest: Trial of ICS therapy warranted in patients: 1) whose FEV1 < 50%. & 2) who experience frequent exacerbations. *Newer ICS agents i.e.: -budesonide -fluticasone -mometasone May have less of a risk of S/Es. • Combination of LABA & ICS: -For convenience & ease of use. -Showed greatest FEV1 response w/ No difference in the exacerbation rate. *Mucolytic/Expectorant agents: - Showed NO clinical benefit in COPD. *Respiratory stimulants: -Not recommended due to short-lived effect + potential risk. • α₁-Antitrypsin Replacement Therapy: - Only used for the rare inherited form of emphysema. - Requires weekly or twice weekly infusions. - Not indicated for other forms of emphysema. • Non-pharmacologic Approaches: 1) Tobacco Cessation 2) Pulmonary Rehabilitation 3) Nutritional Therapy 4) Keeping Immunization Current 5) Supplemental O₂ Therapy 1) Tobacco Cessation: * Difficult to achieve & maintain. • The most important intervention in the prevention & treatment of COPD. • Slows the rate of loss of lung function • Most important & beneficial intervention • Associated w/ immediate & sustained health benefit. 2) Pulmonary Rehabilitation: a. Patient Education ( ̴Dz., technique, adherence, self management skills). b. Exercise Training. c. Psychological Support & intervention (for anxiety & depression). d. Nutritional Therapy. 3) Nutritional therapy in COPD was shown to be valuable in: 1. Relieving symptoms 2. Improving exercise tolerance 3. Improving overall health status • Poor nutrition has sig. impact on COPD. • Pulm. Rehab.: 1. Less beneficial in preventing complications & exacerbations. 2. No effect in reducing mortality or slowing dz. progression. 4) Keeping Immunization Current: a. The inactivated IM Influenza virus vaccine should be used because it has been shown to reduce serious illness & death in COPD pts. b. Pneumococcal vaccine is recommended to be given SQ or IM because it provides prophylaxis against most common strains of Strep. Pneumiae. 5) Supplemental O₂ Therapy: (Long-Term Therapy) -Improves survival in COPD pts. w/ chronic hypoxemia. -Benefit seen if: - pO₂<55mmHg or -pO₂<60mmHg w/ evidence of end- organ effect of COPD, i.e.:*Cor pulmonale *Polycythemia *Cognitive impairment • Greatest benefit shown in those who used O₂ for @ least 15hrs/d. • Nasal Cannula: The most common & convenient method of O₂ supplementation. • ABGs & Pulse Oximetry: The 1⁰ methods for determining O₂ saturation. • Goal of Therapy: Maintain O₂ saturation ≥ 90%. • Most are managed @ flow rates of 1-4L/min. • Surgical Management: • For those who can NOT be managed medically. 1. Bullectomy: -Removing bullea (large air spaces in lungs)not participating in gas exchange 2. Lung Volume Reduction Surgery (LVRS): -More common -More comprehensive procedure in removing non-functional segments of lung tissue. 3. Lung Transplantation:-Used in advanced COPD • Managing Exacerbations: • Associated w/ increased morbidity & mortality. • Acute worsening in patient’s baseline, i.e.: -worsening dyspnea -increased cough -change in volume & appearance of sputum beyond the day-to-day variations. • Severity: Levels 1-3 -Level 1: Managed as outpatient (E.R.) -Level 2: Requires hospitalization -Level 3: Complicated by respiratory failure • General Management: 1) Supplemental O₂ if warranted. 2) Intensification of bronchodilation therapy. 3) Systemic corticosteroid therapy. 4) Antibiotics in most cases. 5) Ventilatory support if respiratory failure is present. 1) Level 1: • Commonly treated w/ intensification of bronchodilator therapy: -Increase dose of SA bronchodilators (comb. SABA + Ipratropium) by MDI or Neb. -Less evidence to the role of LA bronchodilators: Guidelines recommend LA bronchodilators to be continued or added if pt’s condition warrants. • Level 1 therapy involves use of Short Course of Systemic Corticosteroid: -improves lung function. & -reduces relapse rate. **Prednisone 0.5-1 mg/kg/d X 10-14 d * Insufficient data on ICS use in COPD exacerbation • Antibiotics are commonly used in COPD exacerbations: * S.Pneumoniae, M.Catarrhalis, H.Influenzae were found in pts. w/ stable COPD or exacerbation representing either colonization or infection. *The presence of 2 of 3 of the following is an indicator for antibiotic use: 1. Increased dyspnea 2. Increased sputum 3. Increased sputum purulance **Traditional antibiotics are as effective as newer ones ** Duration of antibiotic therapy= 7-10 days 2) Level 2: • Frequently treated as inpatients. • Treatment approach similar to level 1. • Oral antibiotics & corticosteroid if possible (as effective as parenteral) • Consider extended-spectrum antibiotics esp. if Ps. Auroginosa is suspected. 3) Level 3: • May require ventilatory support. • Aggressive bronchodilator therapy. • Corticosteroid therapy. • Broad-spectrum antibiotics may be warranted initially. • Follow-up w/in 1 month of hospitalization. * Theophylline oral or IV has minimum benefit in acute exacerbations of COPD. ** Prophylactic Antibiotics to reduce exacerbations is NOT proven effective & increases the risk of resistance. ** Very Important Tables: 1) Table 35.11 p.935: General Principles for Pharmacotherapy of COPD 2) Table 35.12 p. 936