BlueCare Middle Region Letter 11/11/14
advertisement

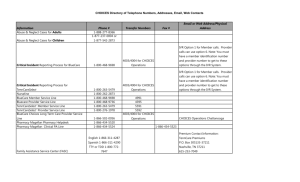
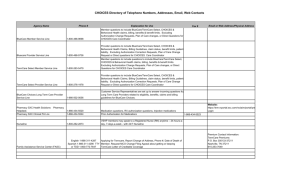
Date: Dear Health Care Provider: BlueCare Tennessee is looking forward to serving the members of the Middle Grand Region once again beginning January 1, 2015. Many of you have been providing services for TennCareSelect members, and we are happy to expand those services to additional BlueCare members. We are sending this letter to help make you aware of the transition of members, services and some guidelines that could impact you and your members. Effective 12:01 a.m. on Jan. 1, 2015, approximately 140,000 members in Middle Tennessee will be transitioned by the State of Tennessee to BlueCare Tennessee. Members will be notified of their assignment to BlueCare with a welcome letter in November, 2014, and a welcome packet to be mailed to them in December, 2014. Members will have the opportunity to notify TennCare if they wish to stay with their current Managed Care Organization (MCO) or choose another MCO. Our records indicate you currently have a provider agreement in place with BlueCare. The current terms of that contract will continue to apply as they do today once these members transition to BlueCare in January If you would like to discuss your current contracts, please contact your local Provider Network Manager by calling: Chattanooga West/Middle Tennessee (Nashville/Memphis/Jackson) Johnson City/Knoxville (East TN) (423) 535-6307 (855) 646-9258 (865) 588-4640 Ensuring our members have access to care during this transition time is important to us. BlueCare’s existing contract with you has provisions to ensure a smooth transition for members with an existing course of treatment, allowing members to continue to receive services from their treating provider for up to thirty (30) days. In certain circumstances, members may be able to temporarily keep their current health care provider. For example, a pregnant woman in her second or third trimester will be able to keep her current health care provider through her delivery and follow-up care – even if her provider does not participate in the BlueCare network. BlueCare will coordinate the care of a member during and after transition. To ensure continuity of ongoing treatment and services, the current health plans are transferring authorization information to BlueCare. Letters will be sent to you the beginning of December listing the services that have been approved for members into 2015. For the most up to date information related to authorizations and referrals, please make sure to review the authorization requirements in the Utilization Management Program section of the BlueCare Provider Manual on the BlueCare Tennessee Website at www.bluecare.bcbst.com. If one of the providers within your office does not currently have a BlueCare contract and they would like to contract, please contact the Provider Network Services area at 1-800-924-7141 and choose “touchtone” Option 2 or say “Network Contracts or Credentialing” when prompted. The staff will be able to help you with your contracting needs. If you are a primary care physician, please make sure your on-call coverage is up to date. BlueCare Tennessee and BlueCare, Independent Licensees of BlueCross BlueShield Association Things to Do: 1. Search the Provider Section of the BlueCare Tennessee’s Website – http://bluecare.bcbst.com/Providers/index.html. The website presents the most up-to-date information featuring the BlueCare Tennessee’s Provider Administration Manual which is updated quarterly, newsletters, Electronic Data Interchange, regulations, guidance and Medicaid audit contractors along with provider education and resources. 2. Please make sure you have a current Ownership and Disclosure form submitted with BlueCare Tennessee. If you need a new form or have questions, please call 1-800-924-7141 and choose the “touchtone” option 2 or say “Network Contracts or Credentialing” when prompted. To print a copy of the form, visit the BlueCare Tennessee website at http://bluecare.bcbst.com/forms/Provider%20Forms/Disclosure_form_for_a_Provider_Person.pdf. 3. Ensure your information is up-to-date with CAQH®. BlueCross BlueShield of Tennessee has partnered with the Council for Affordable Quality Healthcare (CAQH®) to offer practitioners Universal Provider Datasource (UPD), a universal credentialing application tool. With a single, uniform, online application, practitioners can enter their credentialing information and later access, manage and revise that information at their convenience. The UPD credentialing application tool is available at no cost to practitioners. Beginning Jan. 1, 2015, BlueCross will require new credentialing applications from licensed health care professionals to be submitted through CAQH. The UPD Quick Reference Guide, available on the CAQH website, <http://www.caqh.org/pdf/UPDbrochure.pdf>, provides step-by-step instructions for online registration and how to get started using UPD. To help you with any questions you may have related to the transition to the BlueCare network, there are some Frequently Asked Questions (FAQs) on the BlueCare Tennessee website. Go to www.bluecare.bcbst.com “2015 Statewide / Health Plan Changes” or call the BlueCare Provider Service Line – 1-800-468-9736. We appreciate the opportunity to work with you in our efforts to provide Tennesseans with quality, cost-effective health care. Thank you for your support. Sincerely, Amber Cambron BlueCare Tennessee CEO and President