Coxibs - คณะแพทยศาสตร์ศิริราชพยาบาล, Faculty of Medicine Siriraj
advertisement

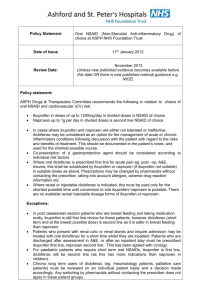
Clinical Use of NSAIDs Ajchara Koolvisoot, M.D. Division of Rheumatology Department of Medicine Outline • Clinical application & Practical use Indication Efficacy Safety • Practical approach & recommendation Efficacy : Mechanism of Action Action Mechanism 1. Anti-inflammatory COX-2 2. Analgesic & antipyretic COX-2 3. Carcinoprotective COX-2 4. Anti-platelet COX-1 ( TXA2 ) Efficacy of Specific COX-2 inhibitor = Classical NSAIDs Except : No antiplatelet effect หญิงอายุ 48 ปี มีโรค HT มีอาการปวดหลัง ตรวจพบมี OA change ที่ spine ท่ านจะสั่ งยาใด • A. Indomethacin • B. Naproxen • C. Celecoxib • D. Acetaminophen + orphenadrine • E. Acetaminophen โดดๆ หญิงอายุ 55 ปี พึง่ วินิจฉัยว่ าเป็ นโรค rheumatoid arthritis ได้ ยา ibuprofen 600 มิลลิกรัมต่ อวัน 2 สั ปดาห์ ไม่ ดีขน ึ้ ท่ านจะทาอย่ างไร • A. ให้ยาเดิม แต่เพิม่ ขนาดเป็ น 1600 มิลลิกรัมต่อวัน • B. เปลี่ยนเป็ น Indomethacin 75 มิลลิกรัมต่อวัน • C. ให้ยาเดิม แต่ add prednisolone 20 มิลลิกรัมต่อวัน • D. ให้ยาเดิม + แนะนาว่ารอยาออกฤทธิ์ก่อน และโรคเป็ นแบบนี้เอ • E. ส่ ต่อ rheumatologist Anti-inflammatory Properties • Clinical application & characteristic : No difference among all NSAIDs Individual response Drug properties - Dose & duration Optimal Use of NSAIDs • Is NSAID really needed ? Which indication ? Dose ? Interval of Rx ? • Any underlying disease ? • Drug interaction ? หญิงอายุ 48 ปี มีโรค HT มีอาการปวดหลัง ตรวจพบมี OA change ที่ spine อย่ างเดียว ท่ านจะสั่ งยาใด • A. Indomethacin • B. Naproxen • C. Celecoxib • D. Acetaminophen + orphenadrine • E. Acetaminophen โดดๆ หญิงอายุ 55 ปี พึง่ วินิจฉัยว่ าเป็ นโรค rheumatoid arthritis ได้ ยา ibuprofen 600 มิลลิกรัมต่ อวัน 2 สั ปดาห์ ไม่ ดีขน ึ้ ท่ านจะทาอย่ างไร • A. ให้ยาเดิม แต่เพิม่ ขนาดเป็ น 1600 มิลลิกรัมต่อวัน • B. เปลี่ยนเป็ น Indomethacin 75 มิลลิกรัมต่อวัน • C. ให้ยาเดิม แต่ add prednisolone 20 มิลลิกรัมต่อวัน • D. ให้ยาเดิม + แนะนาว่ารอยาออกฤทธิ์ก่อน และโรคเป็ นแบบนี้เอ • E. ส่ ต่อ rheumatologist Anti-platelet Properties • Clinical application & characteristic : Drug Anti-platelet Character Classical NSAIDs ++ Reversible T1/2 dependent COX-2 inhibitor - - ASA ( low dose ) +++ Irreversible ยาใดในกลุ่ม NSAIDs สามารถใช้ ในโรค familial polyposis coli ได้ • A. Celecoxib • B. Etoricoxib • C. Indomethacin • D. ASA • E. All of above Carcino-protective Properties • Clinical application : Disease Familial adenomatous polyposis ( FAP ) Choice Most classical NSAIDs & ASA COX-2 inhibitor : Celecoxib Dose 200-400 mg BID reduced number 28%, size 30.7% ( placebo 4.5% & 4.9% ) ( NEJM 2000 June 29; 342: 1946-1951 ) Inhibited by NSAIDs Apoptosis Growth factor Induced apoptosis Angiogenesis ยาใดในกลุ่ม NSAIDs สามารถใช้ ในโรค familial polyposis coli ได้ • A. Celecoxib • B. Etoricoxib • C. Indomethacin • D. ASA • E. All of above Adverse Effects Diverse physical, chemical, Inflammatory & mitogenic stimuli COXIBS COX-1 COX-2 Tissue specific isomerases Prostanoids Prostacyclin Endothelium Kidney Platelet brain Thromboxane A2 Prostaglandin D2 Platelet Smooth m. vv. Macrophage Kidney Mast cell Brain Airway Prostaglandin E2 Prostaglandin F2α GI Uterus Brain Airway Kidney Smooth m.vv. Smooth m vv. Eye Adverse Effects • Gastrointestinal > 10% • Cardiovascular • Renal & electrolytes 1-10% • CNS • Hematologic • Dermatologic & hypersensitivity • Hepatic < 1% Safety Risk of Cardiovascular Events NSAIDs & CVS : Mechanism Platelet COX-1 X Arachidonic acid NSAID Thromboxane TXA2 Cox-2 inhibitor Prothrombotic state Endothelial COX-2 X X Prostacyclin PGI2 Antithrombotic state ยา Coxibs ใด มีผลข้ างเคียงทาง CVS น้ อยทีส่ ุ ด • A. ทุกตัวในกลุ่ม ทาให้เกิด thrombosis มากพอๆกัน • B. Lumiracoxib • C. Etoricoxib • D. Celecoxib • E. Parecoxib Kearney PM, et al. BMJ 2006 Vascular events 1.42 ( 1.13-1.78 ) Myocardial infarction 1.86 ( 1.33-2.59 ) Coxibs increase risk of MI & vascular events > Placebo Dose-Response Relationship of AMI risk 2.5 Diclofenac > 150 2 Rofecoxib > 25 Naproxen > 1000 Celecoxib > 200 1000 > 150 ac <= g > 200 = 200 0.5 Odds Ratio Naproxen < 1000 Diclofenac < 150 en <= mg Celecoxib < 200 b > 25 Rofecoxib < 25 1 <= 25 1.5 COX-2 Inhibitors : Chemistry Generic name Chemistry COX-2 • Celecoxib Sulphonamide 30 • Valdecoxib Sulphonamide 261 • Parecoxib Sulphonamide 261 • Rofecoxib Sulphonyl 276 • Etoricoxib Sulphonyl 344 • Lumiracoxib Phenyl acetic acid 433 Half-life & CV Risk • Half-life : Rofecoxib Valdecoxib > Celecoxib Longer T1/2 More CV events Coxibs & BP Effect Effect of Time to CV events • Within the first 10-30 days of Rx • Cumulative effect with time • Risk persists 30 days after discontinuation ยา Coxibs ใด มีผลข้ างเคียงทาง CVS น้ อยทีส่ ุ ด • A. ทุกตัวในกลุ่ม ทาให้เกิด thrombosis มากพอๆกัน • B. Lumiracoxib • C. Etoricoxib • D. Celecoxib • E. Parecoxib Coxibs : Cardiovascular Risk • Drug : Class effect ? No Individual properties ? : Yes Dose-related Dose Molecule/Chemistry Yes Half-life Yes Effect to BP & sodium Yes • Duration of Rx Yes Is Naproxen Cardio-protective ? Versus placebo Versus Coxibs Risk of MI in Classical NSAIDs Study Relative risk Relative risk 1.19 ( 1.08.1.31 ) Classical NSAIDs increase risk of MI > Placebo ยา NSAIDs ใด มีผลข้ างเคียงทาง CVS มากทีส่ ุ ดในกลุ่ม • A. ทุกตัวในกลุ่ม ทาให้เกิด thrombosis มากพอๆกัน • B. Diclofenac • C. Ibuprofen • D. Meloxicam • E. Naproxen Summary : Meta-analysis & Systemic Review • Rofecoxib • Celecoxib • • • • Naproxen Diclofenac Piroxicam Ibuprofen < 25 mg/d > 25 mg/d > 400 mg/d < 200 mg/d RR 1.33* -1.73* 2.19* 1.56* -2.70* 1.0 0.92-0.97 1.40* -1.63* 1.06 ( 0.70-1.59 ) 1.07-1.51* Thromboxane Inhibition ( COX-1 mediated ) Prostacyclin Inhibition ( COX-2 mediated ) Diclofenac Rofecoxib Celecoxib Etoricoxib Lumiracoxib Ibuprofen Anti-thrombotic More GI side toxicity Prothrombotic Less GI side effect COX-2 Inhibitors : COX-Selectivity ASA Naproxen ยา NSAIDs ใด มีผลข้ างเคียงทาง CVS มากทีส่ ุ ดในกลุ่ม • A. ทุกตัวในกลุ่ม ทาให้เกิด thrombosis มากพอๆกัน • B. Diclofenac • C. Ibuprofen • D. Meloxicam • E. Naproxen EMEA : June 2005 • Coxibs should not be used in pts with established CAD, stroke and/or peripheral arterial disease • Caution when prescribing Coxibs in pt with CAD risk ( HT, hyperlipidemia, DM, smoking ) • Use the lowest effective dose & shortest duration • Warning of hypersensitivity esp. in first month use GI Side Effects Renal Side Effects ชายอายุ 79 ปี เป็ น HT คุมได้ ดี BP 120/80 พึง่ ได้ รับยา Etoricoxib 1 สั ปดาห์ รักษา OA knee ซึ่งได้ acetaminophen ไม่ ดีขน ึ้ มาพบท่ านเนื่องจาก ขา 2 ข้ างบวมกดบุ๋ม ไม่ มีอาการอื่น BP 140/100 ท่ านจะ ปฏิบัติอย่ างไรเป็ นลาดับแรก • A. ตรวจ U/A และ renal function ทันที • B. ตรวจ LFT และ ดู albumin ในเลือด • C. ยาเดิม เพิ่ม furosemide prn. และ follow up • D. แนะนาว่ามันเป็ นเช่นนี้เอ เพราะเป็ น HT ให้ ดอาหารเค็ม • E. ดยา Etoricoxib ทันที และ เขียนเป็ น drug list แพ้ยา Renal side effect • Incidence up to 1-5% • Risk Volume-contracted states Low cardiac output Other condition compromised renal functions Aging, septicemia, DM, premature baby etc. NSAIDs & Renal Effect Arachidonic acid Coxibs NSAIDs COX-1 COX-2 PGE2 Sodium retention • Peripheral edema • Blood pressure • Weight • CHF (rarely) PGI2 Hyperkalemia Acute renal failure Others : Nephrotic syndrome interstitial nephritis Brater. Am J Med. 1999;107:65S. ชายอายุ 79 ปี เป็ น HT คุมได้ ดี BP 120/80 พึง่ ได้ รับยา Etoricoxib 1 สั ปดาห์ รักษา OA knee ซึ่งได้ acetaminophen ไม่ ดีขน ึ้ มาพบท่ านเนื่องจาก ขา 2 ข้ างบวมกดบุ๋ม ไม่ มีอาการอื่น BP 140/100 ท่ านจะ ปฏิบัติอย่ างไรเป็ นลาดับแรก • A. ตรวจ U/A และ renal function ทันที • B. ตรวจ LFT และ ดู albumin ในเลือด • C. ยาเดิม เพิ่ม furosemide prn. และ follow up • D. แนะนาว่ามันเป็ นเช่นนี้เอ เพราะเป็ น HT ให้ ดอาหารเค็ม • E. ดยา Etoricoxib ทันที และ เขียนเป็ น drug list แพ้ยา หญิงอายุ 29 ปี มีโรค SLE มี active arthritis ได้ ยา chloroquine และ Naproxen 500 มิลลิกรัมต่ อวัน ต้ อง ผ่ าฟันคุด 4 ซี่ ท่ านจะแนะนาอย่ างไร • A. ดยา 24-48 ชม. ให้ acetaminophen แล้วผ่าได้เลย • B. ลด dose 250 มิลลิกรัม/วัน ผ่าได้เลย ( จาเป็ นต้อ ใช้ยา ) • C. ดยา 24-48 ชม. และเปลี่ยนเป็ น prednisolone 20 มิลลิกรัม/วัน ผ่าได้เลย • D. ดยา 5-7 วัน และเปลี่ยนเป็ น celecoxib 400 มิลลิกรัม/วัน • E. ดยา 5-7 วัน ให้ผป.ทนปวดเอา Hematologic : Bleeding • GI • Hemorrhagic stroke • Intra / post-operative bleeding Significant in GU surgery Tosillectomy Underlying bleeding disorder Discontinuation before surgery ASA 7-10 days NSAIDs 3-5 x T1/2 หญิงอายุ 29 ปี มีโรค SLE มี active arthritis ได้ ยา chloroquine และ Naproxen 500 มิลลิกรัมต่ อวัน ต้ อง ผ่ าฟันคุด 4 ซี่ ท่ านจะแนะนาอย่ างไร • A. ดยา 24-48 ชม. ให้ acetaminophen แล้วผ่าได้เลย • B. ลด dose 250 มิลลิกรัม/วัน ผ่าได้เลย ( จาเป็ นต้อ ใช้ยา ) • C. ดยา 24-48 ชม. และเปลี่ยนเป็ น prednisolone 20 มิลลิกรัม/วัน ผ่าได้เลย • D. ดยา 5-7 วัน และเปลี่ยนเป็ น celecoxib 400 มิลลิกรัม/วัน • E. ดยา 5-7 วัน ให้ผป.ทนปวดเอา Other side effects • Dermatologic & hypersensitivity reaction Skin Piroxicam, sulidac, mefenamate Hypersensitivity ASA - asthma • Central nervous system side effect Headache Indomethacin Aseptic meningitis Ibuprofen, sulindac, naproxen Other Properties • Potential application : Closed patent ductus arteriosus Alzheimer disease Practical Approach & Recommendation Is an NSAID needed ? Inflammation ? No Use non-pharmacologic or other pharmacologic Rx Yes Yes Is there a contraindication to NSAID ? - Renal insufficiency ( CrCl < 30 ) - Allergic reaction - Concurrent GI injury No Is there a reason that a classical NSAID cannot be used ? - GI risk+ & Bleeding risk No Use classical NSAID No Yes Use COX-2 inhibitor ( or classical NSAID + PPI+) Is patient at increased risk for CV events ? Select NSAID on the basis of GI risk Yes Avoid NSAID esp. COX-2 inhibitor Quiz ชายอายุ 66 ปี มีโรค angina pectoris ได้ ยา ASA อยู่ ล้ มสะโพกคราก 1 วัน ไม่ มีกระดูกหัก ท่ านจะสั่ งการรักษาอย่ างไร • A. เพิม่ ASA จาก 75 mg/d เป็ น 75 mg tid. • B. เพิ่ม Naproxen 500 mg/d + Omeprazole • C. เพิ่ม Naproxen 500 mg/d + off ASA • D. เพิ่ม Celecoxib 400 mg/d • E. ส่ PM&R ให้ทากายภาพบาบัด ให้ Parecoxib ฉีดลดปวด prn ชายอายุ 66 ปี มีโรค angina pectoris ได้ ยา ASA อยู่ ล้ มสะโพกคราก 1 วัน ไม่ มีกระดูกหัก ท่ านจะสั่ งการรักษาอย่ างไร • A. เพิม่ ASA จาก 75 mg/d เป็ น 75 mg tid. • B. เพิ่ม Naproxen 500 mg/d + Omeprazole • C. เพิ่ม Naproxen 500 mg/d + off ASA • D. เพิ่ม Celecoxib 400 mg/d • E. ส่ PM&R ให้ทากายภาพบาบัด ให้ Parecoxib ฉีดลดปวด prn หญิงอายุ 38 ปี แพ้ยาซัลฟา เป็ นโรค psoriatic arthritis ปวดมากต้ องรับประทานยาแก้ ปวดหลายชนิด หลังกินยามีผื่นทัว่ ตัว ยาใดน่ าจะเป็ นสาเหตุมากทีส่ ุ ด • A. Etoricoxib • B. Indomethacin • C. Nimesulide • D. Meloxicam • E. All of above หญิงอายุ 38 ปี แพ้ยาซัลฟา เป็ นโรค psoriatic arthritis ปวดมากต้ องรับประทานยาแก้ ปวดหลายชนิด หลังกินยามีผื่นทัว่ ตัว ยาใดน่ าจะเป็ นสาเหตุมากทีส่ ุ ด • A. Etoricoxib • B. Indomethacin • C. Nimesulide • D. Meloxicam • E. All of above ชายอายุ 19 ปี วินิจฉัยเป็ น ASA-induced asthma มี acute tendinitis ท่ านจะให้ ยาใด • A. Indomethacin • B. Naproxen • C. Etoricoxib • D. None of above ชายอายุ 19 ปี วินิจฉัยเป็ น ASA-induced asthma มี acute tendinitis ท่ านจะให้ ยาใด • A. Indomethacin • B. Naproxen • C. Etoricoxib • D. None of above Thank You For Your Attention Recommendation Prophylaxis of NSAID-induced GI Side Effects Supot Pongprasobchai, M.D. Assistant Professor, Division of Gastroenterology, Siriraj Hospital NSAID-induced GI Side-Effects Ulcer complications 1-2% Ulcers 20% Dyspepsia 25-50% No lesion/Erosions 60-100% Determination of Gastroduodenal Mucosal Integrity Defensive vs Aggressive Factors Acid Pepsin Mucus HCO3 Bile Alcohol Blood flow PGs Aggressive Defensive Pathogenesis of PU Caused by NSAIDs PGs Acid (acute) Aggressive HCO3 Mucus (chronic) Defensive NSAID-induced Gastropathy 1-2% annually 1-2% annually Strategies to Prevent GI Complications of NSAIDs General Use least ulcerogenic NSAID, short duration Identify risk factors Low-risk : Moderate-risk : High-risk : Very high-risk : no risk factor 1-2 risk factors ≥ 3 risk factors, use of ASA or anticoagulant previous ulcer complications Apply appropriate prevention Co-therapy with gastroprotective drugs Coxib Which non-selective NSAID has lowest GI side-effects? A. B. C. D. E. Aspirin Diclofenac Ibuprofen Indomethacin Piroxicam Relative Risk of GI Complications with NSAIDs Ibuprofen 1 Fenoprofen 1.6 ASA 1.6 1.8 Diclofenac 2.1 Sulindac Diflusinal 2.2 Naproxen 2.2 2.4 Indomethacin 3 Tolmetin 3.8 Piroxicam 4.2 Ketoprofen 9.2 Azopropazon Ketorolac 1 2 3 4 5 6 Relative risk 7 8 9 10 Henry D. BMJ 1996;312:1563-66 Strategies to Prevent GI Complications of NSAIDs General Use least ulcerogenic NSAID, short duration Identify risk factors Low-risk : Moderate-risk : High-risk : Very high-risk : no risk factor 1-2 risk factors ≥ 3 risk factors, use of ASA or anticoagulant previous ulcer complications Apply appropriate prevention Co-therapy with gastroprotective drugs Coxib Risk Factors of Ulcer Complications from NSAIDs Prior GI events 2.5-4.8 Multiple NSAIDs (including ASA) 2-4 2-3.5 Age (>65) Anticoagulant 3 Steroid therapy 2 Co-morbid illness 2 H.pylori infection 2 1 2 3 4 Relative risk 5 6 Number of Risk Factors & Incidence of Ulcer Complications % NNH 5 20 18 15 NNH 12 10 5 8 NNH 125 0.8 NNH 50 2 0 No Risk Factor 1-2 Factors 3 Factors 4 Factors Silverstein FE. Ann Intern Med 1995;123:241-9 Strategies to Prevent GI Complications of NSAIDs General Use least ulcerogenic NSAID, short duration Identify risk factors Low-risk : Moderate-risk : High-risk : Very high-risk : no risk factor 1-2 risk factors ≥ 3 risk factors, use of ASA or anticoagulant previous ulcer complications Apply appropriate prevention Co-therapy with gastroprotective drugs Coxib Strategies to Prevent GI Complications of NSAIDs General Use least ulcerogenic NSAID, short duration Identify risk factors Low-risk : Moderate-risk : High-risk : Very high-risk : no risk factor 1-2 risk factors ≥ 3 risk factors, use of ASA or anticoagulant previous ulcer complications Apply appropriate prevention Co-therapy with gastroprotective drugs Coxib Which co-therapy is most effective in reducing NSAID-associated ulcer complications? A. B. C. D. E. Misoprostal PPI H2-RA Sucralfate Rebamipide Prophylaxis of NSAID-induced Gastropathy Meta-Analysis Serious GI events H2-RA PPI Misoprostal No No Symptomatic No ulcers Endoscopic ulcers Mortality No No No (double dose) Rostom A. Cochrane database of systematic reviews 2007 GI Side Effects of Coxib VS. ns-NSAID Meta-analysis Endoscopic ulcers RR 0.26 [0.23-0.30] Ulcer complications RR 0.39 [0.31-0.50] Ulcer complications (ASA users) RR 0.89 [0.52-1.53] 0.1 0.2 0.5 Favours coxibs 1 2 5 10 Favours ns-NSAID Rostom A. Clin Gastroenterol Hepatol 2007;5:818-28 65 YO woman had Hx of UGIB following NSAID use 2 years ago Now she requires NSAID for severe OA What is the most appropriate management? A. B. C. D. E. Ibuprofen + misoprostal Ibuprofen + PPI Coxib Coxib + PPI No NSAID/Coxib Efficacies of Each Preventive Strategies in Very High-Risk Patients Chan FKL. NEJM 2001; 344: 967-73 Chan FKL. NEJM 2002; 347: 2104-10 Chan FKL. Lancet 2007; 369: 1621-6 NSAID + Hp eradication COXib NSAID + PPI COXib + PPI Prophylaxis of NSAID-induced Gastropathy Recommendation GI Risk Low-risk 6 mo GI complications rate (%) 0.8 • No risk factor Moderate-risk 2 • 1-2 risk factors High-risk 8 • 3 risk factors • on anticoagulant • on ASA* Very high-risk • Prior PU complication 18 Prophylaxis of NSAID-induced Gastropathy Recommendation GI Risk Low CV Risk High CV Risk Low-risk • No risk factor Least ulcerogenic NSAID, lowest effective dose Moderate-risk • 1-2 risk factors High-risk • 3 risk factors • on anticoagulant • on ASA* Very high-risk • Prior PU complication Chan FKL. AP&T 2004;19:1051-61 Prophylaxis of NSAID-induced Gastropathy Recommendation GI Risk Low CV Risk High CV Risk Low-risk • No risk factor Least ulcerogenic NSAID, lowest effective dose Moderate-risk • 1-2 risk factors High-risk • 3 risk factors • on anticoagulant • on ASA* Very high-risk • Prior PU complication Chan FKL. AP&T 2004;19:1051-61 Prophylaxis of NSAID-induced Gastropathy Recommendation GI Risk Low CV Risk High CV Risk Low-risk • No risk factor Least ulcerogenic NSAID, lowest effective dose Moderate-risk • 1-2 risk factors NSAID + PPI/MSP Coxib High-risk • 3 risk factors • on anticoagulant • on ASA* Very high-risk • Prior PU complication Chan FKL. AP&T 2004;19:1051-61 Prophylaxis of NSAID-induced Gastropathy Recommendation GI Risk Low CV Risk High CV Risk Low-risk • No risk factor Least ulcerogenic NSAID, lowest effective dose Moderate-risk • 1-2 risk factors NSAID + PPI/MSP Coxib High-risk • 3 risk factors • on anticoagulant • on ASA* Coxib + PPI/MSP *NSAID + PPI/MSP Very high-risk • Prior PU complication Chan FKL. AP&T 2004;19:1051-61 Prophylaxis of NSAID-induced Gastropathy Recommendation GI Risk Low CV Risk High CV Risk Low-risk • No risk factor Least ulcerogenic NSAID, lowest effective dose Moderate-risk • 1-2 risk factors NSAID + PPI/MSP Coxib High-risk • 3 risk factors • on anticoagulant • on ASA* Coxib + PPI/MSP *NSAID + PPI/MSP Very high-risk • Prior PU complication Coxib + PPI/MSP Chan FKL. AP&T 2004;19:1051-61 Coxib in Patients with CV Risk Important Issues Increased risk of thrombosis risk of Coxib Aspirin decrease GI safety of Coxib Aspirin is like another NSAID Symposium: Clinical NSAIDs Usage 12 Sep 2007 NSAIDs for Acute Pain รศ.พญ.วิมลลักษณ์ สนัน่ ศิลป์ ภาควิชาวิสัญญีวิทยา คณะแพทยศาสตร์ศิริราชพยาบาล Vimolluck Sanansilp, Siriraj Question 1 A 51-year-old man presents with a one-day history of moderately severe low back pain that began after lifting a heavy box. He has a normal neurological examination. He has epigastric pain off and on and has history of allergy to sulfa. What analgesics would you offer? 1. Are NSAIDs an appropriate choice of medication in this patient? 2. If so, which NSAIDs will you prescribe & why? 3. If not, why? Vimolluck Sanansilp, Siriraj Question 2 A 72-y-o man underwent an explor-lap with bowel resection. He has Lt hemiplegia. He gets IV morphine for postoperative pain relief but still has pain score of 7-8. 1. Would you add any NSAIDs to enhance analgesia for this patient? 2. If so, which NSAIDs will you prescribe & why? 3. If not, why? Vimolluck Sanansilp, Siriraj Question 3 A 70-y-o woman underwent Total Knee Arthroplasty. Parecoxib 40 mg i.v. x 3 d, etoricoxib 60 mg p.o. x 5 d. are prescribed. POD 1, drainage = 400 ml blood, BP 120/70 mmHg, PR 96/min, urine output 460 ml/24 h. POD 2, BP 180/100 mmHg, BUN 20, Cr 2.6, edema 2+. What do you think is(are) the problem(s)? Vimolluck Sanansilp, Siriraj NSAIDs and coxibs • Non-selective NSAIDs and coxibs reduce pain safely and effectively in many patients • Neither are as safe as initially thought • Both have similar cardiorenal profiles should be reserved for patients at low risk for cardiac failure or thromboembolic events • CV safety profile: coxibs are contraindicated in patients with known atherosclerotic disease and those at risk of CV thromboembolic events Vimolluck Sanansilp, Siriraj NSAIDs and coxibs • Induced perioperative bleeding small added risk • Surgeons - reluctant to use NSAIDs in some types of surgery:- endoscopic/microscopic or involving the airway, head & neck, plastics, urology and neurosurgery, where bleeding interfere surgical field / increase the level of risk • Devoid of bleeding risk, coxibs = more safely, preor intra-operatively, analgesia + reduce strong opioid rescue pain relief in postoperative period (opioid sparing effect) Vimolluck Sanansilp, Siriraj Vimolluck Sanansilp, Siriraj • Act by inhibition of COX-2 • May be sufficient for moderate pain, • An adjunct in a multimodal regimen to reduce opioid requirements, to improve pain relief and reduce opioid associated side-effects (:- N/V) • Traditional non-selective NSAIDs associated with GI complications: dyspepsia & gastric erosions serious ulcer bleeds and perforations • COX-2 selective inhibitors (coxibs) was developed to improve GI safety in long term antiinflammatory analgesic therapy • Concerns over the CV safety of coxibs and NSAIDs in some postoperative patients • Recommendations and strict guidelines implemented for the use of coxibs, primarily for long-term indications • Efficacy and safety evaluation for the short-term use, focusing on the issues relevant to the surgical setting:- bleeding risk, and GI safety International multicentre study of 1671 patients, CV events (including myocardial infarction, cardiac arrest, stroke and pulmonary embolism) were significantly more frequent among the patients given parecoxib and valdecoxib than those receiving placebo. Nussmeier NA, Whelton A, Brown MT, Langford RM, Joshi G, Verburg KM. Safety of parecoxib and valdecoxib in the treatment of pain following coronary artery bypass surgery. N Engl J Med 2005;352:1081—91. 462 patients, undergoing CABG, reported proportionately more serious CVS sequelae in the patients who received parecoxib/valdecoxib postoperatively. Ott E, Nussmeier NA, Duke PC, Feneck RO, Alston RP, Snabes MC et al. Efficacy and safety of the cyclooxygenase 2 inhibitors parecoxib and valdecoxib in patients undergoing coronary artery bypass surgery. J Thorac Cardiovasc Surg 2003;125:1481—92. By contrast, in a similarly designed study of 1050 non-cardiac major surgery patients, the group randomised to receive parecoxib and valdecoxib did not differ from the placebo patients in any of the four safety categories: cardiovascular events, renal events, surgical wound complications, and GI complications. Nussmeier NA, Whelton A, Brown MT, Langford RM, Joshi G, Singla NK et al. Safety and efficacy of the cyclooxygenase-2 inhibitors parecoxib and valdecoxib after noncardiac surgery. Anesthesiology 2006;104(3):518—26. A combined analysis of 6979 patients in 19 cardiac and non-cardiac surgery studies (10 orthopaedic surgery, 5 gynaecological surgery, 2 general surgery, 2 CABG), in which parecoxib in doses ranging from 20 to 80 mg was administered, the CV thromboembolic event rates were comparable to placebo [parecoxib 20—80 mg/day 1.0% (39/3821) and placebo 0.9% (27/3158)]. Schug S. Poster presentation. ESA; 2006. • Choice of selective COX-2 inhibitor for the acute pain setting is narrow. • Both parecoxib and oral lumiracoxib are licensed for the management of postoperative pain. • Lumiracoxib being limited to orthopaedic and gynaecological surgery. Usual recommended dose for Cox-2 inhibitors in postop. pain Celecoxib (Celebrex®) 200-400 mg/tab Parecoxib (Dynastat®) 40 mg/amp Etoricoxib (Arcoxia®) 60, 90, 120 mg/tab Lumiracoxib (Prexige®) 100, 400 mg/tab first day: 400 mg single dose followed by 200 mg after 12 h if needed, then 200 mg b.i.d. as needed 20-40 mg IV/IM q 12 h (short period) (Can keep diluted med in room temp for 24 h) 120 mg once daily Leaflet: 400 mg once daily not exceed 5 consecutive days Vimolluck Sanansilp, Siriraj …cancelled the registration of lumiracoxib in Australia due to concerns that it may cause liver failure. …8 reports of serious liver adverse reactions to the drug, including two deaths and two liver transplants. Vimolluck Sanansilp, Siriraj NSAID Contraindications Dehydration Hypovolemia Nephrotoxic agents Anticoagulants Vimolluck Sanansilp, Siriraj NSAIDs and Asthma • Study of stable asthmatics given diclofenac orally (Short et al. 2000) • Measured PEFR and FEV 1 pre- and post administration • 56% had drop in values but max 15% • None had to increase their medication • Suggest - acceptable in stable asthmatics Vimolluck Sanansilp, Siriraj Safety Information for COXIBs • Contraindications – Pregnancy and lactating women, Age < 16 y – Patients with Sulfonamide allergy history – Experienced angioneurotic edema, urticaria or allergictype reactions after taking acetylsalicylic acid or NSAIDs or other COX-2 selective inhibitors – Patients who undergone Coronary Artery Bypass Graft (CABG) surgery – Patients with IHD or stroke, CHF – Currently GI bleeding / Active peptic ulceration – Patients who have cardiovascular risks – Patients with renal and hepatic impairment Vimolluck Sanansilp, Siriraj Back to basic analgesia 11th WCP at Sydney, 2005 • • • • Ibuprofen Naproxen Diclofenac Ketorolac • Combination drugs – Opioid + NSAIDs – Opioid + acetaminophen – Tramadol + acetaminophen • Intervention Rx Vimolluck Sanansilp, Siriraj NSAID-Induced Upper GI Bleeds and Perforations Rate of GI Bleeds and Perforations (per 1000 patient years) 3.1 Nabumetone Ibuprofen 4.3 Indomethacin 4.4 5.6 Mefenamic Acid 6.5 Ketoprofen 6.7 Naproxen 7.8 Diclofenac 15.9 Piroxicam 0 2 4 McDonald TM, et al. BMJ 1997; 315: 1333-7. 6 8 10 12 14 16 Vimolluck Sanansilp, Siriraj NSAIDs – for Acute Pain • • • • • • Postoperative – mild to moderate pain Orthopedic – acute low back pain1,2 Dental – periodontitis Oral surgery – 3rd molar surgery Gynecological – dysmenorrhea Urological – renal colic 1 Griffin et al. Do NSAIDs help in acute or chronic low back pain? Am Fam Physician 2002;65 2 Tulder et al. Non-steroidal anti-inflammatory drugs for low-back pain. The Cochrane Database of Systematic Reviews 2000, Issue 2. Art. No.: CD000396. DOI: 10.1002/14651858 Vimolluck Sanansilp, Siriraj NSAIDs – When to give? • Preoperative – premedication preemptive analgesia preventive analgesia • Intraoperative • Postoperative Vimolluck Sanansilp, Siriraj Preemptive analgesia Noxious stimuli Initiating analgesic regimen before onset of noxious stimuli Neurons of dorsal horn of spinal cord “windup/central sensitization (process)” Neurons of dorsal horn of spinal cord become “sensitized” Level of pain Limit subsequent pain Vimolluck Sanansilp, Siriraj Analgesic choices - based on level of pain Strong opioid severe +/- adjuvant +/- NSAIDs Weak opioid moderate +/- adjuvant +/- NSAIDs mild Non-opioid/NSAIDs +/- adjuvant Vimolluck Sanansilp, Siriraj Multimodal Analgesia ₪Improved antinociception Morphine Codeine Tramadol due to synergistic/ additive effects Potentiation ₪Reduce dose of each analgesic NSAIDs,2 agonist, acetaminophen, regional blocks ₪May reduce severity of side effects of each drug Kehlet H, Dahl JB. Anesth Analg. 1993;77:1048–56. Vimolluck Sanansilp, Siriraj Treatment for common menstrual cramps (primary dysmenorrhea) • Lie down at the first sign of pain • Current recommendations = not only adequate rest and sleep, but also regular exercise (especially walking) • Nonpharm. strategies: heating pad, massage, yoga, etc. For mild cramps: aspirin / acetaminophen, or acetaminophen + diuretic For moderate menstrual cramps: main agents are NSAIDs, which lower the production of PG and lessen its effect:ibuprofen; naproxen sodium; and ketoprofen http://www.medicinenet.com/menstrual_cramps/article.htm Vimolluck Sanansilp, Siriraj NSAIDs - Route of administration • • • • Oral IV IM Rectal suppository1 diclofenac (suppo) 50 mg x3 or placebo 1x3 during the first 24 h postoperatively reduces the need for opioids significantly with maintained or improved analgetic effect reduce negative side-effects of systemic opioids 1Olofsson. Eur J Obstet Gynecol Reprod Biol 2000;88:143-6. Vimolluck Sanansilp, Siriraj NSAIDs - Route of administration • • • • • Oral IV IM Rectal suppository Peri- & intra-articular1 Improve early analgesia and mobilization vs contin. Fem. n. block in TKA under spinal anesthesia 1Toftdahl et al. Acta Orthopaedica 2007;78:172-9. Vimolluck Sanansilp, Siriraj NSAIDs - Route of administration Continuous intrawound infusion of diclofenac • Oral demonstrates a greater opioid sparing effect and • IVbetter postoperative analgesia than the same dose administered as an intermittent intravenous • IM bolus during the first 24 h after surgery. • Rectal suppository • Peri- & intra-articular • Local infiltration – single/continuous1 1Lavand’homme et al. Anesthesiology 2007; 106:1220–5. Vimolluck Sanansilp, Siriraj NSAIDs - Route of administration • Oral adm. of COX-1, but not COX-2, • Intrathecal IV specific inhibitors given on postoperative day 1 • IM has analgesic effects in an incisional model of • postoperative Rectal suppository pain in rat. • Peri- & intra-articular • Local infiltration – single/continuous • Intrathecal (COX-1)1 1Zhu et al. Anesth Analg 2005;100:1390 –3. Vimolluck Sanansilp, Siriraj Before prescribing NSAIDs,……weigh risks vs benefits Cost GI CVS Benefits Vimolluck Sanansilp, Siriraj Oral Analgesics for Acute Nonspecific Pain • The safest NSAID is ibuprofen in doses of 400 mg • Higher doses may offer greater analgesia but with more adverse effects • Other NSAIDs fail to demonstrate consistently greater efficacy or safety than ibuprofen • Coxibs provide equivalent efficacy to traditional NSAIDs but lack a demonstrable safety advantage for the treatment of acute pain Vimolluck Sanansilp, Siriraj Oral Analgesics for Acute Nonspecific Pain Direct comparative studies between NSAIDs and acetaminophen (1,000-mg dose) : more effective than acetaminophen in some situations (e.g., dental and menstrual pain) equivalent analgesia in others (e.g., orthopedic surgery and tension headache).1,2 1. Scott D, Smith C, Lohmander S, Chard J. Osteoarthritis. Clin Evid 2003;(9):1301-26. 2. Hyllested M, Jones S, Pedersen JL, Kehlet H. Comparative effect of paracetamol, NSAIDs or their combination in postoperative pain management: a qualitative review. Br J Anaesth 2002;88:199-214. Vimolluck Sanansilp, Siriraj Oral Analgesics for Acute Nonspecific Pain Traditional NSAIDs EFFICACY • Dysmenorrhea1 : ibuprofen=naproxen > acetaminophen/aspirin • Postpartum perineal pain2 : ibuprofen > acetaminophen+codeine+caffeine 1. Zhang WY, Li Wan Po A. Efficacy of minor analgesics in primary dysmenorrhoea: a systematic review. Br J Obstet Gynaecol 1998;105:780-9. 2. Peter EA, Janssen PA, Grange CS, Douglas MJ. Ibuprofen versus acetaminophen with codeine for the relief of perineal pain after childbirth: a randomized controlled trial. CMAJ 2001;165:1203-9. Vimolluck Sanansilp, Siriraj Oral Analgesics for Acute Nonspecific Pain Traditional NSAIDs SAFETY AND ADVERSE EFFECTS • Ibuprofen excellent GI safety profile, not different from placebo (dose 800-1,200 mg/d)1 • Higher doses of naproxen and ibuprofen increased GI side effects similar to other NSAIDs2 1.Kellstein DE, Waksman JA, Furey SA, Binstok G, Cooper SA. The safety profile of nonprescription ibuprofen in multiple-dose use: a metaanalysis. J Clin Pharmacol 1999;39:520-32. 2.Bansal V, Dex T, Proskin H, Garreffa S. A look at the safety profile of over-thecounter naproxen sodium: a meta-analysis. J Clin Pharmacol 2001;41:127-38. Vimolluck Sanansilp, Siriraj Oral Analgesics for Acute Nonspecific Pain COX-2 Selective NSAIDs EFFICACY • Theoretically, provide analgesia = traditional NSAIDs without many of the side effects • Meta-analysis of celecoxib, showed fair to good efficacy for postoperative pain with an NNT of 4.5 (95% CI, 3.3 to 7.2) compared with placebo1 1. Barden J, Edwards JE, McQuay HJ, Moore RA. Single dose oral celecoxib for postoperative pain. Cochrane Database Syst Rev 2004;(3):CD004233. Vimolluck Sanansilp, Siriraj Oral Analgesics for Acute Nonspecific Pain COX-2 Selective NSAIDs SAFETY AND ADVERSE EFFECTS • Greater numbers of thrombotic CV events • May impair renal function and have no benefit over traditional NSAIDs in this area • In elderly patients with hypertension - may be associated with edema and ↑ BP1 1. Whelton A, White WB, Bello AE, Puma JA, Fort JG, for the SUCCESS-VII Investigators. Effects of celecoxib and rofecoxib on blood pressure and edema in patients > or = 65 years of age with systemic hypertension and osteoarthritis. Am J Cardiol 2002;90:959-63. Vimolluck Sanansilp, Siriraj Oral NSAIDs in the Treatment of Acute Pain Medication Efficacy* Max dosage per day Recommended Ibuprofen (400 mg initially) Good 2,400 mg Naproxen (Aleve) Good 1,376 mg Alternative choices Diclofenac (Voltaren) Good 150 mg Piroxicam (Feldene) Good 20 mg Ketorolac (Toradol) Good 40 mg Meclofenamate (Meclomen) Good 400 mg Meloxicam (Mobic) Good 7.5 mg Nabumetone (Relafen) Good 2,000 mg COX-2 inhibitors Fair to good Celecoxib (Celebrex), 400 mg * Poor: number needed to treat (NNT) > 6, Fair: NNT = 3 – 6, Good: NNT = <3 Sachs. Oral analgesics for acute nonspecific pain. Am Fam Physician 2005;71:913-8 Vimolluck Sanansilp, Siriraj Analgesic Side effects class Dosage Comment No evidence that any one NSAID is more effective than another NSAIDs GI, platelet function inhibition, renal dysfunction 400 mg ibuprofen safest inexpensive choice; decreases some adverse GI events with misoprostol 800 mg, H2 blockers, and PPI Selective COX-2 inhibitors Renal dysfunction; hypertension; thrombotic events Once or twice per Expensive day, only advantage over most traditional NSAIDs for acute pain Sachs. Oral analgesics for acute nonspecific pain. Am Fam Physician 2005;71:913-8 Vimolluck Sanansilp, Siriraj Recommendation Label Acetaminophen in doses up to 1,000 mg is the initial choice for most mild to moderate acute pain. B The first-line NSAID for safety, efficacy, and cost is ibuprofen in doses of 400 mg. A For moderate to severe pain, consider narcotic acetaminophen or narcotic ibuprofen combination. B Tramadol, propoxyphene, and codeine provide inferior analgesia A to other recommended agents. COX-2 inhibitors provide analgesia equal to NSAIDs at greater cost and may be reserved for patients who have a history of GI bleeding and have failed treatment with acetaminophen. B A = consistent, good-quality patient-oriented evidence; B = inconsistent or limited-quality patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, opinion, or case series. Sachs. Oral analgesics for acute nonspecific pain. Am Fam Physician 2005;71:913-8 Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain A. Managing pain in the older patient: • NSAIDs and COX-2 inhibitors in older people requires extreme caution • Acetaminophen is the preferred non-opioid analgesic Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain B. Managing acute pain during pregnancy: • Use of NSAIDs during pregnancy does not seem to increase the risk of adverse birth outcome, but ↑risk of miscarriage. Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain C. Managing pain in the puerperium (perineal pain, breast and nipple pain): 1.Acetaminophen and rectal NSAIDs – effective in perineal pain after childbirth. 2.Acetaminophen and NSAIDs – equally, but only modestly, effective in treating uterine pain. 3.Acetaminophen and several NSAIDs, in particular ibuprofen, seem safe non-opioids in lactation. Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain D. Abdominal pain of nonsurgical origin:dysmenorrhea, renal and biliary colic, and irritable bowel syndrome: 1.Analgesics do not interfere with the diagnostic process in acute abdominal pain. 2.NSAIDs – superior to opioids in the treatment of renal colic. 3.Onset of analgesia is fastest with IV NSAIDs in renal colic. 4.NSAIDs + vitamin B1 – effective in the treatment of primary dysmenorrhea. Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain E. Pain associated with acute orofacial conditions:- sinusitis and oral ulceration: 1.NSAIDs and coxibs provide better analgesia with fewer adverse effects than acetaminophen, acetaminophen/opioid combinations, acetaminophen/tramadol combinations, tramadol, or weaker opioids after dental extraction. 2.Aspirin and NSAIDs increase the likelihood of reoperation for post-tonsillectomy bleeding. Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain F. Pain management of acute headache including migraine, cluster headache and postdural puncture headache (PDPH): 1.Aspirin-metoclopramide is effective in Rx of migraine with mild symptoms. 2.Addition of caffeine to aspirin or acetaminophen improves analgesia in acute tension-type headache. 3.Ibuprofen + acetaminophen are effective in the treatment of migraine with mild symptoms. 4.Simple analgesics:- aspirin, acetaminophen, and NSAIDs, either alone or in combination, are effective in the treatment of episodic tension-type headache. Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain G. Acute musculoskeletal pain: 1.Understand that topical + oral NSAIDs improve acute shoulder pain. 2.Treat pain with acetaminophen; if it is ineffective, NSAIDs may be used. Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain H. For nonselective NSAIDs and acetaminophen, know: 1. Different routes & dosage (:- oral, IV, rectal). 2. How to modify doses or withhold NSAIDs in presence of comorbidity (CHF, renal disease, ulcer disease, coagulopathy). 3. How to select particular NSAIDs to lessen risk of specific side effects (:- nonacetylated compounds for platelet sparing; nabumetone to lessen gastrointestinal blood loss). 4. There is a “plateau effect” = dosage increases beyond the recommended range increase the incidence of side effects but do not improve analgesia. Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain H. For nonselective NSAIDs and acetaminophen, know: 5. Efficacy + utility of NSAIDs when administered via intra-articular, topical, local infiltration routes 6. Pharmacokinetic profiles of the NSAIDs 7. Controversies concerning NSAIDs and orthopedic surgery 8. Efficacy of NSAIDs for acute pain: aspirin, ibuprofen, diclofenac, piroxicam, naproxen, and ketorolac Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Acute and Postoperative Pain I. For the COX-2 inhibitors, know: 1. Structural differences between the agents and conventional NSAIDs. 2. Selectivity for the COX-2 enzyme between different agents. 3. Comparisons between COX-2 inhibitors and nonselective NSAIDs in terms of analgesic activity and side-effect profile. 4. The pharmaco-economic impact of COX-2 inhibitors. 5. Opioid-sparing effects. 6. Controversies concerning COX-2 inhibitors Charlton J E, editor. Core Curriculum for Professional Education in Pain. IASP Press, Seattle 2005. Vimolluck Sanansilp, Siriraj Vimolluck Sanansilp, Siriraj