Consult Liaison & Therapeutic Alliance
advertisement

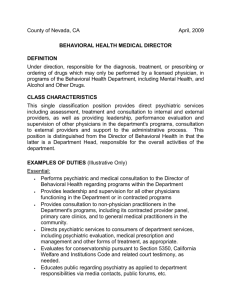
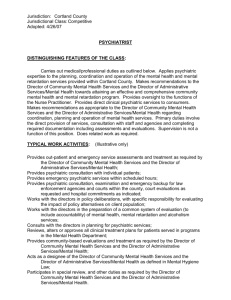
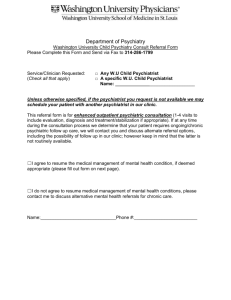
Consult Liaison & Therapeutic Alliance Tony A. Hanna PGY-III Psychiatry Objectives Define Consultation liaison psychiatry. Understand the scope of psychosomatic medicine. Outline the indications for consultation in C/L psychiatry. Outline the model for C/L psychiatry. Understand the approach to C/L psychiatry. Define therapeutic alliance and the 12 “do’s” of C/L psychiatric etiquette. Consult Liaison Services Dr. Fitzgerald (Attending) Dr. Tzoneva (Fellow) Dr. PGY (resident) Medical student Definition Consultation-Liaison Psychiatry is a subspecialty of psychiatry that incorporates clinical service, teaching, and research at the borderland of psychiatry and medicine. (Lipowski, 1983) Psychosomatic medicine: 1) Studies the correlations of psychological and social phenomena with physiological functions 2) Focuses on the interplay of biological and psychosocial factors in the development, course and outcome of all diseases. 3) Advocates the biopsychosocial approach to patient care. History of Consultation – Liaison Psychiatry Its early origins reflect the emergence of General Hospital Psychiatry. In the 1920s psychiatry became closer to medicine as hospitals started to establish psychiatric units . The concept of psychosomatic relationships and the role of emotions and psychological states in the genesis and maintenance of organic diseases emerged. Thus, Consultation – Liaison Psychiatry became an applied form of psychosomatic medicine. History of Consultation – Liaison Psychiatry Considered the earliest advocate for integration of psychiatry and medicine. Wrote the first comprehensive book on mental illness by an American – “Medical Inquiries and Observations upon the Diseases of the Mind” Stressed that diseases of the mind are as certainly object of medicine as diseases of the body. Benjamin Rush 1745 - 1813 History of Consultation – Liaison Psychiatry Developed the concept of psychobiology. Advocated the study of the person in the context of physical, social, psychological life events. Spoke of the medically useless contrast between mental and physical disorders Adolf Meyer (1866 – 1959) History of Consultation – Liaison Psychiatry Considered one of the pioneers of psychosomatic medicine. Worked at the Columbia-Presbyterian Hospital as a psychiatrist assigned to the department of medicine. In 1936 published the conclusions of her study of 600 patients with cardiovascular diseases, diabetes, or fractures. Helen Flanders Dunbar Psychological factors appeared to influence both the etiology and course of the illness in a substantial proportion of these patients. In 1934/35 with Rockefeller foundation grants five general hospitals were able to develop psychiatric departments and stimulate closer collaboration between psychiatrists and other physicians. By the 1960’s-1970’s a subspecialty scientific literature had developed. In 1974 the psychiatric education branch of the NIMH decided to support the development and the expansion of consultation liaison services throughout the US. By 1980, NIMH supported 130 programs and materially contributed to the training of more than 300 consult-liaison psychiatry fellows. Consult-liaison psychiatry continued to grow during the 1980’s despite the federal budget cuts. The years since 2000 have seen a focus on achieving added qualification status by the American Board of Medical Specialty. Fellowship training guidelines and certification examination development are necessary steps toward that goal. Most common reasons for consultation: Delirium, dementia, amnesia and other cognitive disorders-25% Affective disorders, primary or secondary to medical condition-25% Adjustment disorder, maladaptive response to identified stressors, including medical illness15% Somatoform disorders, anxiety disorders, personality disorders -each <10% Data on the distribution of axis II disorders are limited. Models for Consultation The five models for consultation: Patient-oriented (Lipowski 1967) Crisis-oriented (Weisman and Hackett 1960) Consultee-oriented (Shiff and Pilot 1959) Situation-oriented (Greenberg 1960) Expanded psychiatric consultation (E. Meyer and Mendelson 1961) Approach to the Consultation Consultation style Patient confidentiality Patient follow-up Consultation style Characteristics of effective psychiatric consultant (Goldman, Lee, Rudd, 1983): 1. Talks with the referring physician, nursing and other staff before and after consultation. Clarifying the reason for the consultation is the initial goal. 2. Establishes the level of urgency. 3. Reviews the chart and the data thoroughly. 4. Performs a complete mental status exam and relevant portions of a history and physical exam. 5. Gets collateral from family, friends as indicated. 6. Makes notes as brief as appropriate. 7. Arrives at a tentative diagnosis. 8. Formulates a differential diagnosis. 9. Recommends diagnostic tests. 10. Has the knowledge to prescribe psychotropic drugs and be aware of their interactions. 11. Makes specific recommendations that are brief, goal oriented and free of psychiatric jargon and discusses findings and recommendation with consultee – In person whenever possible. 12. Respects patient’s rights to know that the identified “customer” is the consulting physician. 13. Follows-up the patient in hospital, and arranges out-patient care, including help arranging postdischarge referrals. 14. Does not take over the aspects of the patient’s medical care unless asked to do so. 15. Follows advances in the other medical fields and is not isolated from the rest of the medical community. Patient Confidentiality Maintaining absolute Doctor-Patient confidentiality is not possible for a psychiatric consultant. Explain the dual relationship to the patient. Patient Follow-up Frequency and duration of psychiatric follow-up will vary widely depending on the patient’s needs and the financial circumstances. Psychiatric consultant should follow-up patient until they are discharged from the hospital or clinic or until the goals of the consultation are achieved. Case Presentaion Reason for Consult: LG- 38/y/y AAF was assaulted and sustained multiple facial fractures, pt. developed meningitis and endocarditis and is treated with oral Zyvox. Pt refused to leave the room, she thinks that people will look at her and treat her funny. HPI- 38y/y AAF who lives with her mother, grandmother, daughter and 2 grandchildren. Sits for the grandchildren and grandmother who had stroke. 4/21/06 spent the weekend at a motel and upon leaving at midnight, her boyfriend dropped her (at her request) at a disabled neighbor who lives two blocks from the Pt’s house. According to the patient, she wanted to check on her neighbor, but her neighbor did not answer the door. The Pt walked to her house but first decided to stop at a grocery across the street from her house. Before entering the store, she was assaulted and the Pt. does not remember any details until she was in the ER at LSU-S. Pt was transferred from Monroe. Pt denies being depressed but stated she is self-conscious because of her left eye, periorbital scar, loss of vision and ptosis. ”What will people say about this?” “My grandchildren will be scared of me.” Psychiatric review of systems MAPSS Mood-depression (sigecaps): sleeps 8-10 hours,+ helpless, occasional crying spells, no guilt or frustration, not hopeless, appetite normal, good energy with normal concentration. Mood-mania (digfast): negative Anxiety- no flash back, no nightmare Psychosis- no hallucination, no delusion Substance- no tobacco, started beer drinking at age 17 which increased to 6 beer/daily for the last year, history of THC and cocaine abuse X 9 years, last use 3 years ago. Safety- no SI/HI Social History 12th grade education, single with 6 children, liked to socialize, watch TV, go to casino, no church activity, no military service, no history of abuse, jailed a few months, 13 years ago due to an altercation and violating her parole. Past Medical & Psychiatric History none Family History Father & Mother living but separated, no problems. 3 sisters – one sister with HTN 6 children- two daughters, 4 sons, no problems. MSE A&O x4 in casual clothes, cooperative and pleasant, speech normal, mood and affect euthymic, TP organized, TC no hallucinations or delusions, no SI/HI Registration 3/3, Recall 2/3, spells WORLD forward and backward, abstract intact ( do not cry over spilled milk) insight and judgment good. Assessment Axis I - Adjustment disorder with anxiety - ETOH / cocaine abuse - THC abuse in remission Axis II- deferred Axis III- s/p assault with facial and skull fx meningitis, endocarditis, loss of vision-left, ptosis, anemia NC/NC Axis IV- unemployed Axis V- GAF45/55 Treatment/Recommendation Self disclosure Examine pt thoughts Desensitization Alcohol and drug counseling Follow-up with MMH upon discharge Continue to encourage pt to walk out of the room No need for medication. Follow-up Pt was called at home 5/20/06 Mother stated that the Pt is back to her self, not depressed and is following up with MMH, also the Pt has weekend plans to go away and will not return until Monday. What is the most important issue in psychiatric care? SAFETY What is the second most important issue? Therapeutic Alliance What is Therapeutic Alliance? The readiness of a patient to work with energy with a willing psychotherapist. It has not commonly applied to the type of brief encounter experience by the consultation-liaison psychiatrist in hospital setting. Nonetheless, insofar as the consulting psychiatrist fosters hope and expectation in patients seen in that context, however brief the contact , the relationship (alliance) has the capacity to promote maturation and well-being in any patient. The psychiatric consultant makes use of all the principals of good psychotherapy although they are often modified to accommodate the realities of the hospital setting and the unusual way in which psychiatrist and patient are brought together. Dr. Joel Yager’s twelve behaviors as a list of “do’s”, somewhat analogous to the ten commandments of etiquette in the psychiatric consultation described by Pasnau. I. Sit Down. Sitting reduces the status difference between MD and Pt and the likelihood that the Pt will perceive the MD to be assuming a lordly demeanor and also conveys to the patient that the MD has some time to spend with them. Introduce yourself. State the reason for the visit. Ask for permission to sit. II. Do something tangible for the patient. Farther the rapport. Be helpful in small ways, do what a good nurse will do, ask the Pt if he is comfortable. Increase the comfort of the Pt. III. Touch the Patient The physical intimacy of touch is helpful with a frightened, dependant, and/or very physically ill patient and conveys a human caring that can reduce the feeling of aloneness and alienation in dehumanizing medical environments. Handshake, hold Pt hand, touch Pt shoulder The least touched Pt – AIDS, Cancer IV. Smile Reduces interpersonal distance Decreases sense of threat Has a disarming effect Must be culturally acceptable V. Begin by telling the patient what you know about his/her situation. Ask the patient to correct you. The positive effects * Pt does not have to go through the information again. * helps to get feed-back from Pt. * Pt will assess the level of the consultants understanding and concern. VI. Ask the patient what his/her most pressing concerns of the moment are. The Pt’s preoccupation with major fear or concern needs to be cleared to have the Pt’s full attention and cooperation. Clears the air so the necessary information can be used more effectively. VII. Ask in detail about the patient’s belief system regarding the nature, cause and prognosis of the illness or injury, and about the patient’s specific concerns about pain, disability, disfigurement or death. Tune into the Pt perspective and expectations of what the Pt is confronting. Correct misimpressions and provide education. (facilitate cooperation with RX) VIII. Ask in detail about the patient’s family major social roles such as occupation, and the impact of the current illness or injury on those relationships and roles. Pt is concerned about the negative consequences of the illness on loved ones and on the ability to maintain major social role functions in family, work and community. IX. Ask about the specific personal characteristics, activities and attainments the patient has achieved in life in which he/she takes pride and find an opportunity to complement these qualities. Improve self esteem and the Pt feels that the consultant appreciates the Pt, not as a simply dependent creature. X. Acknowledge the human blight in which the patient finds him/herself. The physician should tell the Pt that faced with similar circumstances, the physician might well display similar psychological difficulties. Strengthen the physician/Pt relationship Legitimize and validate the Pt and support self esteem. XI. Fully explain the need for and purpose of mental status exam in an informative way and involve the Pt as an ally an co-investigator. XII. Leave the patient with something concrete. Give the Pt a revised formulation. Tell the Pt what you intent to do with the information. Ask the Pt for feedback. Tell the Pt when you are coming back for follow-up. 2000 My vet gave me an Axis II diagnosis. Personality disorder -incompatible with large dogs in house. Treatment Guido Hanna a pure-bred dachshund, who believes he is a doberman, was added to the family. Guido Hanna Discussion