File - Krystal Morris MSN Portfolio
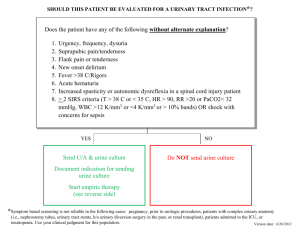
advertisement

Oral Case Presentation Krystal Morris April 12, 2012 47 year old Caucasian male who presented to the ED with a chief complaint of “going through a really bad alcohol withdraw lately.” Three days prior to coming into the ED, patient began binge drinking, up to 2L of Vodka per day, his last drink one day ago. Patient reports that he binge drinks to the point of blacking out. Patient’s wife found him minimally responsive yesterday. Throughout the day, patient became more alert. Since yesterday, the following symptoms have progressed: Sweating, palpitations, nausea, dry heaves, vomiting. No food or fluid intake for several days. Patient denies fever, chest pain, chest pressure, no vomiting frank blood or coffee ground emesis. Regular bowel movements with no frank blood in the stools, no black or tarry stools. Patient reports he binge drinks every 1-3 months, usually for 2-3 days for the past 20 years. Patient’s wife disagreed with these numbers, stating in the last year the patient binge drinks 2-3 nights every week. Patient reports that he goes to alcohol support groups, and his wife states that he really doesn’t go. 20 years ago when binge drinking began, patient experienced first withdrawal symptoms with some seizure activity. Patient has been on Librium on a PRN basis for 20 years. His primary care provider will currently not prescribe the medication because of noncompliance issues. He is a 25 pack year smoker. Patient reports difficulty initiating stream and painful urination. Two weeks ago, patient was seen at a low income health care clinic in town for urinary frequency and difficulty initiating a stream, although he reports that he has always had an overactive bladder. Urinalysis there was negative for infection. Prostate exam performed and patient was told it was enlarged. Past Medical History: Bilateral inguinal hernia repair. Patient denies a history of CVA, CAD, DVT/PE or Diabetes. Review of Systems Constitutional: Chills, sweats, fatigue, decreased activity. No fevers. Eye: Dizziness and vertigo several days ago. Not present at this time. Ear/Nose/Mouth/Throat: Negative Respiratory: Negative. Cardiovascular: Palpitations, no chest pain or heaviness associated with palpitations. Gastrointestinal: Nausea, vomiting, loss of appetite. No food or drink other than alcohol for several days. Genitourinary: Urinary frequency, urinary hesitancy. Hematology/Lymphatic: negative Endocrine: negative Musculoskeletal: Patient reports trips/falls frequently when balance is off from alcohol consumption Integumentary: Negative Neurologic: Alert and oriented x4. Denies headache Psychiatric: Anxiety, Depression, denies any current suicidal ideations. Physical Exam General: Alert and oriented, no acute distress. Vital signs: Blood pressure: 150/77 (101), heart rate 105, O2 sats 96% on room air, 37.0 TMax Eye: Pupils are equal, round, and reactive to light HENT: Normocephalic, atraumatic Neck: Supple Respiratory: Lung are clear to auscultation bilaterally. Respirations are non-labored. Breath sounds are equal. Symmetric chest was expansion. Cardiovascular: Irregularly irregular rhythm. No murmur, 3+ pulses, equal in all extremities. Capillary refill <3 seconds. Gastrointestinal: Normal bowel sounds. No tenderness to light palpation. RUQ tenderness to deep palpation Musculoskeletal: Normal full range of motion. 5+ strength in all extremities. Integumentary: Warm, dry. Neurologic: Alert, oriented. Normal sensory. Cranial nerves II-XII are grossly intact . No nystagmus or tremors. Psychiatric: Cooperative, appropriate mood and affect, non-suicidal. Building Differential/Working Diagnosis The patient’s history of alcohol abuse was the most significant part of his history in making my differential diagnosis. He had been heavy binge drinking up to 2L of vodka per day x3 days. From his basic symptoms, it was apparent he was starting to have some withdrawal symptoms. Working/Differential Diagnosis Closed head injury Patient reports blacking out and has a history of falls. Newer abrasion on lip. Hypovolemia Frequent vomiting Obtain orthostatic blood pressures to further assess. Start IVF if necessary Illicit drug abuse Based of symptoms of sweating, palpitations UDS Obtain history from patient and wife Bipolar Disorder Patient’s binge drinking could be a sign of mania follow by low periods when patient is withdrawing Pyelonephritis Urinary frequency, hesitancy Obtain UA. Has patient been having fevers? Flank pain? Blood in urine? Librium Withdrawal Patient usually takes medication for withdraw symptoms, hasn’t been able to obtain a refill from his primary care physician due to compliance issues. Symptoms of withdrawal include sweating, palpitations, tremors Alcohol Withdrawal Patient has been binge drinking several days, history of alcohol abuse Making the Diagnosis Labs were the most significant aspect of the work-up formulating the final diagnoses Lab tests ordered: CBC, CMP, PT/INR, Cardiac Markers, Hgb A1C, toxicology screen, urinalysis and culture EKG: Sinus tachycardia with trigeminal pattern PVCs. Chest X Ray: Negative on wet read, awaiting final report Labs & Diagnostics CBC & Differential WBC 17.8 H RBC 5.01 Hgb: 15.8 Hct: 43.7% MCV: 87.2 Platelets: 300 Neutrophils: 76.6% H Lymphocytes: 13.8% L CMP PT/INR Na: 120 L K 3.7 Cl: 79 Co2: 21 Glucose: 162H BUN 23 Creatinine: 1.2 Ca: 10.1 Total Protein: 8.4H Albumin: 5.1 Alk Phos: 64 AST: 32 ALT: 39 Total Bilirubin: 0.6 Lipase: 23 GFR: >60 Hgb A1C: 5.6% with estimated glucose of 114 PT: 12.50 sec INR: 0.95 Cardiac Studies CKMB: 5 Myoglobin: 295H Troponin: <.01 CK: 483 H Toxicology Screen Negative for: Ethanol Barbituates Bezodiazepines Cannaboid Cocaine Methadone Phencyclidine Oxycodone Acetaminophen Amphetamines Urinalysis Clarity: Clear Glucose: Negative Bilirubin: Negative Ketones: TRACE Specific Gravity: 1.020 Blood: MODERATE amount PH: 6.0 Protein 100mg/dl H Nitrates: Negative WBCS: 12 to 50 H RBC: 5 to 10 Bacterial FEW Hyaline Casts: 50 to 100H Mucous: Present This UA was then sent for culture Sepsis present on admission SIRS criteria: WBC >12,000, Tachycardia >90 Alcohol withdrawal Patient reports binge drinking x3 days. Reporting withdraw symptoms such as chills, diaphoresis, fatigue, insomnia, anorexia, & palpitations. Start ETOH Withdrawal protocol. UTI Present on Admission, culture pending See lab results for abnormal values from culture Plan of Care: Start IV Rocephin. Once culture is back, make sure organism is susceptible to Rocephin. 1g IV Q24H. Abnormalities on UA results indicate a UTI per literature. First line treatment for uncomplicated UTI in men is Bactrim and Floroquines (Cipro, Levaquin). According to Micromedex 2.0, Rocephin is an appropriate choice for an uncomplicated UTI. Maximum daily dose is 2g IV. 1g is dosage that is prescribed. Therefore, this antibiotic is an appropriate choice for this patient. Hyponatremia Na: 120 Plan of Care: Monitor Na on Labs. Start NS gtt at 125ml/hr. Monitor for a slow rise in the serum Na. Monitor for MS changes that can be associated with hyponatremia. Acute Renal failure BUN/Creatinine ratio is greater than 20/1 (23/1.2) Plan of Care: Monitor urine output and lab trends According to the literature, an increase in serum creatinine >0.5mg/dl above baseline is considered Acute renal failure. Baseline creatinine was obtained 3 months prior, showing a creatinine of 0.7mg/dl. Creatinine today is 1.2. This is >0.5 above baseline, therefore can be considered acute renal failure. Volume depletion is the likely cause for the increase in creatinine. Therefore, volume resuscitation and closely monitoring urine output is vital to this patient. Hypochloremia Cl: 79 Plan of Care: Monitor labs for increase in Cl, likely from vomiting. Plan to stop vomiting through the use of antiemetics. IVF to help with the volume depletion. Orthostatic Hypotension due to dehydration Baseline BP 150/77. Drop in BP from supine to sitting and then sitting to standing Plan of Care: Bolus 1L NS, start maintenance IVF, NS @ 125ml/hr Intractable N/V Times several days Plan of care: PRN IV Antiemetics and NPO for now, okay to advance as tolerated Sinus Tachycardia with Trigeminal pattern PVCs Per EKG and telemetry monitoring Plan of care: Telemetry and electrolyte monitoring. Cardiac enzymes Q6h x3 more draws. Troponin was <.01, myoglobin elevated Urinary Frequency X2 weeks Plan of Care: Started on Rocephin IV which will help with urinary frequency from UTI Elevated glucose likely to stress response and infection Glucose 165 on Chemistry. A1C 5.4% Plan of Care: Monitor CBG Q6 hours. History of Alcohol Abuse Several other hospital visits for alcohol abuse. History per patient Plan of Care: Psych nurse referral. Social work consult. Pt interested in rehabilitation options Depression Previous suicide attempts x2 Plan of Care: Psych nurse referral. Pt reports uncontrolled depression with current medication he is taking History of Seizures with alcohol withdraw: Last seizure 20 years ago. Pt was on Libirum PRN Plan of Care: Seizure precautions and high fall risk. Withdraw protocol ordered It is important to identify patients with SIRS criteria early. What are the criteria for Systemic Inflammatory Response Syndrome? Systemic Inflammatory response syndrome SIRS criteria states that 2 or more of the following must be present in order for + criteria: Temperature >38.5 or <35 HR >90 RR >20 or PaCo2 <32 WBC >12,000 or <4,000 >10% immature bands Sepsis Known source on infection must be present. used to properly diagnosis sepsis along with 2+ of the above SIRS criteria Severe Sepsis At least one of the following signs if hypo perfusion or organ dysfunction Areas of mottled skin Capillary refill >3 seconds Urine output <0.5 mL/kg for at least one hour, or renal replacement therapy Lactate >2 Mental status changes Platelet count <100,000 DIC Acute lung injury or acute respiratory distress syndrome (ARDS) Cardiac dysfunction Septic shock — Septic shock exists if there is severe sepsis plus one or both of the following