File - Nursing Portfolio
advertisement

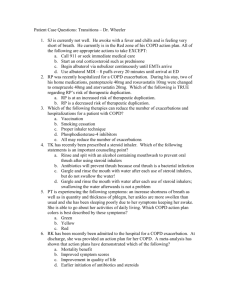
Running Head: TEACHING PLAN: COPD Teaching Plan: COPD Sara Hannah California State University Stanislaus 1 TEACHING PLAN: COPD 2 Patient Information: Patient RH is a 55 year old Caucasian male who has been recently diagnosed by his primary care physician with Chronic Obstructive Pulmonary Disease (COPD). RH has a 25 year smoking history and drinks alcohol socially. RH has an increased BMI and reports a sedentary lifestyle. Upon being diagnosed with COPD, RH has many questions. Those questions will be addressed in the teaching plan below. Evaluation for teaching: RH’s primary language is English but he is hard of hearing. There is no language barrier but it will be important to make sure that what is said to RH has been heard. This can be done by asking RH to repeat back directions and information. RH is literate but his education level is limited therefore east-to-read pamphlets and brochures should be used. RH has no physical disabilities. He works five days a week and lives at home with his wife and two children. RH appears skeptical about his diagnosis. He states he has tried to quit smoking in the past and has not been able to. He states his wife also smokes which makes it hard for him to stop. He smokes more when stressed and his job is demanding at times which makes him smoke more. He states he is tired of coughing and his episodes of shortness of breath. He is ready to make changes towards a healthier lifestyle and states he is willing to listen to his options. RH appears ready to learn. The issue will more likely be sticking to a regimen in this case, including sticking to smoking cessation. The patient has heard of COPD in the past; he states that his father had it. He watched his father need oxygen more and more just to be able to breath. He states he does not want to let himself get to that point. He has a considerable amount of knowledge on TEACHING PLAN: COPD 3 what COPD looks like but not a lot of knowledge about his options for treatment and prevention of exacerbation. Appropriate referrals will include scheduling an appointment with a pulmonologist for further evaluation if needed. Teaching Plan: Outlined below are teaching points to review with the patient. The teaching is divided into a background of COPD, treatment options and how a nebulizer is used. Behavioral objectives include identifying what COPD is, what the symptoms are and why it develops. Also included is the importance of treatment and smoking cessation. The content below identifies what leads to a diagnosis of COPD and what to do once diagnosed. It reviews what can make COPD worse and what can make it better. Outlined also are the prevalence of COPD in The United States and what can happen if left untreated. Medications and treatment options are included with focus on nebulization. Instructional teaching methods include one-on-one discussion with therapeutic communication. This includes eye contact, speaking clearly and directly, and asking for verification of understanding. Must consider hard-of-hearing here. Nebulizer information and brochures can be used. Websites and videos should be shared if RH would like more information once back home. Evaluation of teaching will include verbal verification of the following topics: the importance of smoking cessation, plan with willingness to initiate of smoking cessation, list of changes towards healthier lifestyle including diet and exercise and the ability to verbalize treatment options that are available. 4 TEACHING PLAN: COPD COPD Teaching Points Background: COPD stands for chronic obstructive pulmonary disease. It is a progressive respiratory disease that makes breathing more difficult over time. It is characterized by chronically poor airflow. Main symptoms include shortness of breath, a cough that lasts longer than 3 months a year for over 2 years, and sputum production. Most people with chronic bronchitis have COPD. The most common cause of COPD is tobacco use. Other factors include genetics and air pollution but those play a smaller role. Long-term exposure to irritants such as these causes an inflammatory response in the body. Part of this response is the narrowing of small airways and breakdown of lung tissue known as emphysema. To diagnose COPD, lung function tests are done evaluating airflow. COPD is different from asthma in that is does not improve significantly with medication. Pulmonary function testing includes patient history, a physical, chest x-rays, arterial blood gas analysis and pulmonary function testing. These are performed by a respiratory therapist. Two common function tests are TLC (total lung capacity) and MVV (maximal voluntary ventilation). An incentive spirometer is the most recognizable of the tests. Teaching for patients with COPD includes smoking cessation, vaccinations, rehabilitation, bronchodilators, steroids, long-term oxygen therapy and lung transplantation. COPD is the most common lung disease. It is the fourth leading cause of death in the world. COPD affects 329 million people totaling 5% of population. Estimated economic cost was over $2.1 trillion in 2010. TEACHING PLAN: COPD 5 Advanced stages of the disease leads to strain on the right ventricle of the heart secondary to high pressure on arteries of the lungs. This leads to leg swelling and jugular vein distension. Respiratory diseases are especially dangerous in young children and the elderly. Treatment of COPD with Nebulizer: A nebulizer treatment is important for the patient with COPD because it allows the bronchodilators to reach constricted alveoli because of the mist form that it takes. Nebulizers are machines that convert liquid medicine into a mist that you inhale into your lungs. Nebulizers can be a good option for those with COPD that have a difficult time using an inhaler. The process of nebulization involves a compression air pump, tubing, a well for medicine, and either a mask or mouthpiece to breath into. The pump continuously pushes air through the tube. When the air passes through the well with the medication, it mixes with the liquid to form tiny droplets that are small enough for the patient to breath into the lungs. The patient should breath in and out normally. Each treatment lasts between 515 minutes depending on the type of medication and nebulizer. Medication choices include bronchodilators and anticholinergics. Some people with COPD need treatment with inhaled corticosteroids that reduce swelling in air passages. They can be long acting or short acting. -Short-acting bronchodilators that are beta2-agonists include Albuterol (Proventil), Alupent, Maxair and Xopenex (Levabuterol). -Long-acting beta2-agonists that are considered controllers or maintenance TEACHING PLAN: COPD 6 include Serevent, Foradil, Perforomist and Brovana. These should be taken every day and not just with flare ups. -An Anticholinergic that affect nerve impulses sent by vagus nerve is Ipratropium (Atrovent). -Common hospital prococol calls for the popular duoneb treatment which is a mixed medication including Albuterol and Ipratropium. Common dose of Albuterol via nebulizer is 2.5 mg 3-4 times a day. Common dose of Xopenex is 0.63 mg 3 tid. Common dosage of Ipratropium is 500 mcg or 1 vial 3-4 times a day. Patients should ask their healthcare provider if they need to use the nebulizer daily or just in cases of COPD flare-ups. Patients need to be aware of their prescribed amount of medicine to use, which is usually 2-5 drops, and to not take more medication if it isn’t working. They should instead seek medical help right away. It is important to keep track of you medication and to get prescriptions refilled on time incase of a flare up. Side effects include headache, dizziness, dry mouth, cough, blurred vision, nausea, hoarseness. Instructions For Use (Using Duoneb for this example) -Advantages and disadvantages -Hook up hose to machine -Put prescribed amount of liquid medicine on outer portion of well -Close chamber and flip the switch to begin air flow TEACHING PLAN: COPD -Standard airflow is 5 L/min at home and per hospital protocol -Apply mask or mouthpiece to patient; mist will show that medicine is being administered -Duoneb is Albuterol and Ipratropium -Treatment lasts 5-10 minutes -Breathing should be regular with some slow deep breaths as tolerated by patient -disinfecting should be done in container with 1 part distilled vinegar and 3 parts warm water 3 times a week; wash with dish soap after each use -Avoid cleaning tubing, rinse all washed components and set out to air dry -Filter on pump should be replaced; increasing frequency with more frequent treatments 7 8 TEACHING PLAN: COPD References Anderson, Leigh Ann (2014, January). How to use a nebulizer. Drugs.com. Retrieved March 10, 2014 from http://www.drugs.com/cg/how-to-use-a-nebulizer.html Kaneshiro, Neil. (5/26/2012). How to use a nebulizer. Medline Plus. Retrieved March 10, 2014 from http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000006.htm Potter, Patricia, Anne Perry, Patricia Stockert, Amy Hall. Fundamentals of Nursing, 8th Edition. Mosby, 2013. VitalBook file.