Medical management of stable angina
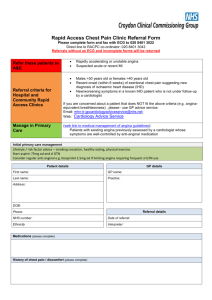
advertisement

Actions for Practice Teams Medical management of stable angina due to coronary artery disease June 2012 www.pctsla.org Actions for Practice Teams Why are we looking at this? • • • • • 2 Approximately 140,000 men and 116,000 women in the West Midlands have angina.1 Approximately 1% of visits to a GP are because of chest pain.2 Between April 2010 to March 2011, approximately 11,000 patients were referred to rapid access chest pain clinics in the West Midlands3 Between April 2010 and March 2011, approximately 10,000 emergency hospital admissions in the West Midlands were because of angina pectoris.4 Optimal management of angina could reduce complications of the disease, improve patient quality of life, decrease GP and hospital attendance and costs to the NHS. Actions for Practice Teams What are we covering? The following slides provide information on: • • • • Features and diagnosis of stable angina Education and lifestyle advice Secondary prevention of cardiovascular disease in patients with stable angina Anti-anginal drug therapy o Short-acting nitrates o Beta-blockers o Calcium channel blockers o Long-acting nitrates o Nicorandil o Ivabradine o Ranolazine 3 Actions for Practice Teams Introduction • • 4 Angina is caused by restriction of blood flow and oxygen to the heart, usually due to obstructive coronary artery disease (CAD)5-7 Angina adversely affects quality of life and increases the risk of myocardial infarction and mortality. In clinical trials of stable angina: o annual mortality is approximately 0.9 to 1.4%.5 o annual incidence of non-fatal myocardial infarction (MI) is between 0.5% and 2.6%. 5 • Risk factors for angina are5,6: o Older age o Male sex o Cardiovascular risk factors (e.g. history of smoking, diabetes, hypertension, dyslipidaemia, family history of premature CAD) o History of documented CAD (e.g. MI, coronary revascularisation) Actions for Practice Teams Features of stable • angina6,7 5 Symptoms of typical stable angina are: o central or left-sided chest pain or discomfort (may radiate to neck, jaw, shoulders and arms) o precipitated by physical exertion o relieved by rest or GTN within about 5 minutes • People with: o Non-angina chest pain have one or none of these features o Atypical angina: two features o Typical angina: all three features Actions for Practice Teams • • Features of acute coronary syndrome6 6 Stable angina should be clearly distinguished from acute coronary syndrome (MI/unstable angina) as these patients require urgent hospital admission. Patients with acute coronary syndrome (ACS) may present with o o o o pain in the chest or arms, back or jaw for longer than 15 minutes chest pain with nausea and vomiting, sweating, breathlessness chest pain associated with haemodynamic instability new onset chest pain, or abrupt deterioration in previously stable angina, with recurrent chest pain occurring frequently and with little or no exertion. Actions for Practice Teams NICE CG95: diagnosis of stable • • • • angina6 7 Stable angina should be diagnosed according to NICE guidance. Local guidance should also be consulted. In people presenting with intermittent stable chest pain, NICE recommend that stable angina diagnosis should be based on: clinical assessment alone or clinical assessment + diagnostic tests If a person presenting with stable chest pain has features of typical angina (based on clinical assessment) + estimated likelihood of CAD is greater than 90%, further diagnostic testing is not necessary. Manage as angina. In people without confirmed CAD, in whom diagnosis of stable angina is uncertain (people with estimated likelihood of CAD 10 to 90%), clinical assessment + further diagnostic tests are required. o Treat as stable angina while waiting for the results. • NICE do not recommend use of exercise ECG to diagnose or exclude stable angina in people without known CAD. Non-anginal chest pain Atypical angina typical or atypical symptoms, assume estimate > 90%. For women > 70 years assume estimate of 6190% EXCEPT women at high risk with typical symptoms (estimate risk > 90%) • Values are % of people at each middecade age with significant CAD. • Hi = High risk = Diabetes, smoking and hyperlipidaemia (total cholesterol > 6.47 mmol/litre) • Lo = Low risk = None of these three • The shaded area represents people with symptoms of non-angina chest pain, who would not be investigated for stable angina routinely. NOTE: These results are likely to overestimate CAD in primary care populations. If there are resting ECG ST-T changes or Q waves, the likelihood of CAD is higher in each cell of the table. Typical angina Actions for Practice Teams NICE (CG95): Percentage of people estimated to have CAD according to typicality of symptoms, age, sex and risk factors6 • For men aged > 70 years with Age (years) 35 45 55 65 Men Women Men Women Men Women 8 Lo 3% 9% 23% 49% Hi 35% 47% 59% 69% Lo 1% 2% 4% 9% Hi 19% 22% 25% 29% Lo 8% 21% 45% 71% Hi 59% 70% 79% 86% Lo 2% 5% 10% 20% Hi 39% 43% 47% 51% Lo 30% 51% 80% 93% Hi 88% 92% 95% 97% Lo 10% 20% 38% 56% Hi 78% 79% 82% 84% Actions for Practice Teams Education and lifestyle advice • • • • • 9 Offer advice including information on long-term course, risks and benefits of treatment. Address concerns (e.g. impact of stress, anxiety or depression, physical exertion including sexual activity). Dispel myths. Advise on self-management skills such as pacing activities and goal setting. Advise on lifestyle changes including smoking cessation, healthy diet with adequate intake of fish, fruit and vegetables, weight loss and control of lipid levels, alcohol within safe limits LGV and PSV licence holders should inform the DVLA Advise patients to seek professional help urgently if their angina suddenly worsens. Actions for Practice Teams Secondary prevention of CV disease in patients with stable angina8 Offer a statin to all patients in line with NICE guideline on lipid modification (CG67) Consider aspirin 75 mg daily Consider angiotensin-converting enzyme inhibitors (ACEi) if the patient has diabetes. ACEi should be continued if already taken for other comorbidities. Initiate antihypertensive therapy, if appropriate. Manage other co-morbidities including diabetes and renal disease. Review existing medication for exacerbating drugs (e.g. NSAIDs). For most patients, treatment should be initiated with simvastatin 40 mg. Consider risk of bleeding and comorbidities. NICE recommend ACEi for some patients with hypertension (CG127), heart failure (CG108), diabetes (CG87, CG15), chronic kidney disease (CG73) or post-MI (CG48) 10 Actions for Practice Teams NICE CG126: Anti-anginal drug therapy8 11 Offer a short acting nitrate (for immediate short term relief)1 and either a beta blocker or calcium channel blocker (CCB) as first-line treatment2 If symptoms not controlled on either beta-blocker or CCB, consider other option or use both drugs together3 If beta blocker or CCB not tolerated consider switching to other option If both beta blocker or CCB not tolerated consider monotherapy with a long-acting nitrate or ivabradine or nicorandil or ranolazine If symptoms not fully controlled, consider adding a long-acting nitrate or ivabradine4 or nicorandil5 or ranolazine If symptoms not satisfactorily controlled with two anti-anginal drugs and the person is waiting for revascularisation (or revascularisation not appropriate), consider adding third anti-anginal drug. Do not offer a third anti-anginal drug if stable angina is controlled with two drugs 1) Advise on how and when to use and explain side effects. Dose should be repeated if pain has not gone 5 mins after first dose. Call ambulance if pain not gone 5 mins after second dose. 2) Review response to all drug treatment 2 to 4 weeks after starting or changing treatment. Titrate dose (according to symptom control) up to maximum tolerated dose 3) When combining a calcium channel blocker with a beta-blocker, use a dihydropyridine CCB (e.g. amlodipine or felodipine) 4) When combining ivabradine with a CCB, use a dihydropyridine CCB 5) Nicorandil is not currently licensed for use as add-on therapy Actions for Practice Teams Which beta-blocker? • • • • • 12 No good evidence that one beta-blocker is more effective in than another in managing stable angina.9 Select according to contraindications, co-morbidities, patient preference and cost.8 Avoid beta-blockers if history of asthma or bronchospasm. Contraindicated in decompensated heart failure or critical peripheral vascular disease.9 Do not combine a beta blocker with verapamil and use caution with diltiazem.9 Sudden withdrawal may cause exacerbation of angina9 Actions for Practice Teams Which calcium channel blocker? • • • • • 13 CCBs include dihydropyridines (e.g. amlodipine, felodipine), benzothiapines (diltiazem), and phenylalkylamines (verapamil).9 Important differences between CCB classes but evidence does not support a recommendation to use a specific CCB. Choose according to contraindications, co-morbidities, patient preference and cost.8 Dihydropyridines may cause reflex tachycardia, flushing, headache, and ankle swelling. Short acting formulations of nifedipine are not recommended.8,9 Diltiazem and verapamil may cause bradycardia o Avoid in heart failure9 o Do not combine a beta blocker with verapamil, caution with diltiazem9 o Constipation common with verapamil9 Prescribe SR nifedipine and diltiazem (other than 60 mg) by brand Actions for Practice Teams • • • • • Other anti-anginal drugs: long-acting nitrates 14 Treatment option if first-line therapies inadequately control symptoms or are contraindicated/not tolerated.8 Long acting nitrates are less expensive than ivabradine and ranolazine. Isosorbide mononitrate is generally preferred to isosorbide dinitrate. Continuous use of long-acting nitrates induces tolerance, with reduced therapeutic effect o Standard release isosorbide mononitrate should be used in an asymmetric dosing interval to minimize development of tolerance9 o Modified release isosorbide mononitrate should be used once daily to maintain a nitrate-low period9 MR isosorbide mononitrate more expensive than standard-release. If an MR preparation is appropriate, brand name prescribing of the lowest cost MR preparation is recommended. Actions for Practice Teams Other anti-anginal drugs: nicorandil • 15 Treatment option if first-line therapies inadequately control symptoms or are contraindicated/not tolerated.8 • Potassium-channel activator with a nitrate component. • Headache is a common side effect.9 • MHRA safety advice (2008)10: o Consider nicorandil treatment as a possible cause in people who present with symptoms of gastrointestinal ulceration. o Ulcers are refractory to treatment; withdraw nicorandil. o Withdraw only under the supervision of cardiologist • • Advise patients to not drive or operate machinery until it is established that nicorandil does not impair their performance9 Not currently licensed for use as add-on therapy.9 Actions for Practice Teams Other anti-anginal drugs: ivabradine • • • • • 16 Treatment option for patients in sinus rhythm if first-line therapies inadequately control symptoms or are contraindicated/not tolerated.8 Lowers heart rate at rest and during exercise. (Note: ventricular rate at rest should not be allowed to fall below 50 beats per minute).11 If combined with a calcium channel blocker, use a dihydropyridine calcium channel blocker (e.g. MR nifedipine, amlodopine or felodipine).8 Visual disturbances (phosphenes) are a common adverse effect.11 Data on long term efficacy and safety are limited.8 Actions for Practice Teams Other anti-anginal drugs: ranolazine • • • • • 17 NICE guidance includes ranolazine as treatment option if firstline therapies inadequately control symptoms or are contraindicated/not tolerated.8 Ranolazine increases exercise time and reduces frequency of angina attacks but effects are modest and clinical significance is uncertain.8,13 Data on long-term efficacy and safety are limited. Safety concerns: associated with QT interval prolongation and syncope, contraindications include some other cardiac agents.9 MTRAC do not recommend ranolazine for prescribing.12 SMC does not recommend use of ranolazine in NHS Scotland.13 Patients taking ranolazine should carry a “patient alert card.”14 Actions for Practice Teams Annual Cost of anti-anginal drugs ivabradine (Procoralan®) (5 mg bd - 7.5 mg bd) ranolazine (Ranexa®) (500 mg bd - 750 mg bd) isosorbide mononitrate M/R (Monomax SR®) (60 mg M/R bd) isosorbide mononitrate (20 mg tds) nicorandil (10 mg bd - 20 mg bd) diltiazem (Angitil SR®) (120 mg tds) diltiazem (60 mg tds) felodipine (5 mg - 10 mg) metoprolol (50 mg bd - 100 mg tds) verapamil (80 mg tds - 120 mg tds) bisoprolol (10 mg od -10 mg bd) amlodipine (5 mg - 10 mg) atenolol (100 mg) £1,047 £524 £596 £596 £231 £23 £155 £84 £135 £67 £110 £55 £68 £19 £65 £29 £30 £15 £13 £12 £11 £0 £200 Maximum Prices: Drug Tariff May-12 and MIMS Jun-12 18 £400 Minimum £600 £800 £1,000 £1,200 Actions for Practice Teams Investigation and • • revascularisation8 19 If symptoms are not adequately controlled with optimal medical treatment (two anti-anginal drugs + secondary prevention drugs), consider revascularisation (CABG or PCI) CABG also option to improve prognosis in a specific subgroup of patients with left main stem or proximal three-vessel disease Actions for Practice Teams What are the key actions/issues? • • 20 Do you know how many emergency hospital admissions from your practice are due to angina pectoris? Are you aware of the local care pathways for people with stable angina? o Care pathways for chronic stable angina currently may vary from area to area according to local commissioners and the local services available. • Review current prescribing for patients with stable angina to ensure that it is in-line with NICE and MHRA guidance. For example: o Short-acting nitrates (e.g. glyceryl trinitrate) should be prescribed for all patients with stable angina o For first-line treatment , use either a beta-blocker or a CCB o Anti-anginal drugs other than beta-blockers or CCBs should not be used as first-line treatments for stable angina Actions for Practice Teams Key actions/issues continued.. 21 o Check patients prescribed a beta-blocker do not have underlying asthma or bronchospasm o Check for patients prescribed a beta-blocker with verapamil (could lead to extreme bradycardia) o Check for patients with heart failure prescribed diltiazem/verapamil (may cause deterioration) o Check for patients prescribed ivabradine with verapamil/diltiazem (not recommended) o Review use of potentially exacerbating drugs (e.g. NSAIDs) Actions for Practice Teams References 22 1. Coronary Heart Disease Statistics 2010 edition. British Heart Foundation Statistics website. http://www.bhf.org.uk/research/statistics.aspx 2. Stewart S, Murphy NF, Walker A et al. The current cost of angina pectoris to the National Health Service in the UK. Heart 2003;89:848-53. 3. Rapid Access Chest Pain Clinic. Department of Health. May 2011. http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/Integratedperfomancemeasuresm onitoring/DH_112551 4. Hospital Episode Statistics. April 2009 to March 2011. 5. Fox K, Garcia MA, Ardissino D et al. Guidelines on the management of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur Heart J 2006;27:134181. 6. Chest pain of recent onset: Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin. CG95. National Institute of Health and Clinical Excellence. 2010. http://publications.nice.org.uk/chest-pain-of-recent-onsetcg95/introduction <accessed 5/2012> 7. Jokhu P, Curzen N. Ischaemic heart disease: stable angina. Medicine 2010; 38: 414-420. 8. The management of stable angina (CG126). National Institute of Health and Clinical Excellence. 2011. http://www.nice.org.uk/Search.do?searchText=angina&newsearch=true&x=0&y=0#/search/?reload 9. BNF 63 (2012) British National Formulary. 63rd edn. London: British Medical Association and Royal Pharmaceutical Society of Great Britain. 10. Nicorandil: gastrointestinal ulceration. Drug Safety Update. 2008. Medicines and Healthcare products Regulatory Agency http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON085019 <accessed 5/2012> 11. Procoralan. Electronic medicines compendium. 2012. http://www.medicines.org.uk/EMC/medicine/17188/SPC/Procoralan/#INDICATIONS <accessed 5/2012>12) 12. Ranolazine (Ranexa). Midlands Therapeutics Review and Advisory Committee. 2009. http://www.keele.ac.uk/pharmacy/mtrac/mtracverdictsheetsescas/ <accessed 5/2012> 13. Ranolazine, 375mg, 500mg and 750mg prolonged-release tablets (Ranexa®). Scottish Medicines Consortium. 2012. http://www.scottishmedicines.org.uk/files/advice/ranolazine_Ranexa_2nd_Resubmission_FINAL_Dec_2011_for_website.pdf <accessed 5/2012> 14. A.Menarini Pharma U.K.S.R.L. Ranexa 375 mg prolonged-release tablets. Electronic medicines compendium. 2012. http://www.medicines.org.uk/EMC/medicine/21402/SPC/Ranexa+prolonged-release+tablets/ <accessed 5/2012>