General Medical Microbiology
advertisement

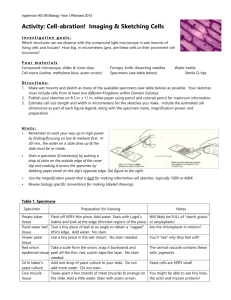
MICR 301 – Fall, 2011 • • • • • • • • • • • • • Office Hours Lecture Schedule & Reading Texts Case Study Reports Websites Course Prerequisite Course Objectives Class Attendance Student Evaluation & Grading Academic Honesty Model of Creative Problem Solving Critical Thinking Skills Laboratory Schedule QUESTIONS??? General Medical Microbiology Specimen Collection and Processing Specimen Collection • Failure to isolate causative agent of infectious disease frequently result of faulty collecting or transport techniques • Therefore, when collecting specimen for microbiological examination, several general considerations need to be addressed Specimen Considerations • Representative of disease process – i.e. for pneumonia - sputum not throat swab • Sufficient material collected • Avoid contamination by patient’s microbial normal flora • Collect before antibiotic therapy started • At acute phase of disease • Delivered promptly to lab • Clinical information to guide culture and ID Sterile Specimen • • • • • Blood Cerebral spinal fluid (CSF) Tissue Serous fluids Specimens from the lower respiratory tract (LRT) • Urine directly from bladder or kidney Specimen With Microbial Normal Flora (NF) • Upper respiratory tract (URT), including mouth and nose • Sputum (LRT) • Feces • Genital tract • Skin • Low number organisms: – Conjunctiva of eye – External ear Circumventing Normal Flora • Antiseptics (iodine, alcohol) - apply to skin prior to aspiration of abscess, blood, CSF • Decontamination – selectively inhibit or destroy NF i.e. treat sputum with NaOH before culturing for Mycobacteria • Selective media – inhibit growth of NF and allow growth of pathogen i.e. bile salts for Enterics • Quantification – >#MOs than expected; i.e. procedure used for urine culture Urine Culture • A calibrated loop delivers 1 ul of urine (10-3ml) • If colony count >100 colonies (#MOs >105/ml) is considered significant and indicates infection Circumventing Normal Flora - Microscopy • Cytological exam - look for presence of squamous epithelial cells in urine, sputum, or wound specimens • If present, indicate likely contamination with skin or mucosal flora • A new specimen should be requested when numerous squamous epithelial cells present Poor Sputum Specimen • Numerous squamous cells observed (oval, rounded) • Suspect mucosal cells from oral tract Good Sputum (LRT) Specimen • Lung epithelial cells (elongated) • None or few squamous cells Circumventing NF: Invasive Procedures • Allow physician to avoid NF when collecting specimen: – – – – Transtrachael aspirate Suprapubic aspirate Bronchoscopy (bronchial wash) Needle biopsies Transtrachael Aspirate Suprapubic Aspirate Specimen Identification • • • • • Patient’s name and ID number Patient’s location Patient’s physician Site/source of specimen Type of exam requested (bacteria, fungus, virus, parasite) • Tentative clinical diagnosis • Date and time of specimen collection • If antibiotics administered - type, dosage and time Specimen: Swab • Convenient and economical, but: • Often inadequate amount • Recovery of bacteria usually <10% of original innoculum • Often used for throat cultures and for cervical, vaginal and urethral secretions • Newer “Flocked Swabs” – increase surface area, collect more sample (fluid, cells) • Should not be used: – Pus or exudate is available – Surgical specimens – Anaerobe or Mycobacterium Specimen: Devices, Transport, Media • Syringes – good for aspirates; needles plugged with sterile stopper • Tubes, bottles, and jars – sterile, leak proof • Fecal transport systems – polyvinyl alcohol fixative for preservation of fecal parasites • Sexually transmitted diseases - best to inoculate media directly at bedside of patient or use swab/transport media to retain viability • Specimens for virus or anaerobe culturing need appropriate transport media to retain viability Specimen Transport • Promptly transport to lab – Preserve viability fastidious MOs – Prevent overgrowth rapidly growing bacteria which may not be pathogen • Sometimes refrigeration warranted i.e. urine specimen • Refrigeration kill some fastidious MOs – Streptococcus pneumoniae (sputum) – Neisseria gonorrhoeae (genital tract) Blood Specimen • Septicemia – organisms or their toxins present and growing in blood • Bacteremia - presence of organisms in blood without causing infection • For septicemia, 2-3 cultures collected by venipuncture in a 24 hour period: – Collect 20-30 mls for each culture – Inoculate into media directly at bedside of patient Wound Specimen • Best specimen is aspirate of pus or exudate • A swab is usually not a good way to collect specimens from wounds Sterile Body Fluids • Meningitis and encephalitis – collect CSF via a lumbar puncture • Pleural, pericardial and synovial fluid – aspirate and collect sufficient amount Respiratory Specimen • Upper respiratory tract infection – a swab is sufficient • Lower respiratory tract infection – collect sputum. Alternatively, may use: – Transtracheal aspiration – Bronchial wash – Lung aspirate Urinary Tract Specimen • Clean voided midstream specimen to limit NF • Catherization • Suprapubic aspiration of bladder or kidney GI and Genital Specimen • Gastroenteritis – collect stool sample in sterile container • Intestinal parasite - three separate stool specimens collected as some present intermittently • Genital tract infection – swab or aspirate of exudate plus direct inoculation onto media Other Specimens • Ocular infection – a swab is sufficient • Tissue specimen – by biopsy or autopsy Direct Gross Exam of Specimen • CSF – if cloudy indicates infection • Sputum – color, consistency and odor gives clues as to causative agent – Clear=virus – Greenish=bacteria • Stool - mucous and blood is typical of dysentery • Anaerobe – often foul odor • Actinomycete - visible granules (which are bacteria aggregates) Microscopy Exam: Differential Stain – Gram Stain • Gram(+) or Gram(-) • Oil immersion – shape of bacteria • Low power - fungi, some parasites, WBCs (hallmark of acute bacterial infection is numerous PMNs) • Positive and negative controls always done • Gram stain of direct smear provide important information for some specimens, but useless for others (Give examples of each) • Important not to over interpret Gram stain result Gram Stain of Bacillus species (B+) Gram Stain of Staphylococcus aureus (C+) Gram Stain of Neisseria species (C-) Gram Stain of Haemophilus species (B-) Differential Stain: Acid-fast Stain • Acid-fast and non Acid-fast MOs • Clinically important for diagnosing TB • Mycobacterium tuberculosis grows slowly, may be 6-8 weeks before culture report • Important to physician - if seen in direct smear, start TB antimicrobial therapy Special Stain:Spore Stain • Spore structure formed by vegetative cell under adverse conditions, for survival • Position of spore may be diagnostically important • Bacillus, Clostridium Capsule Stain • Outer structure, carbohydrate or protein; protect against host phagocytosis • Background and MO stained, capsule left unstained • Klebsiella pneumoniae Trichrome Stain • For permanent stained smears of intestinal parasites • Giardia lamblia (trophozoite) Iron-hematoxylin Stain • Another way to make permanent stained smears of intestinal parasites • Entamoeba histolytica (cyst) Wright Stain / Giemsa Stain • Stain for blood cells • Parasites and bacteria in the blood are seen • Trypanosoma in a blood smear India Ink Wet Mount • For encapsulated yeastlike fungi, capsule remains unstained • Cryptococcus neoformans Lactophenol Cotton Blue Stain • Observe fungi • Hyphae, conidia 10% KOH Wet Mount • Observe fungi from skin scrapings • KOH destroys epithelial cells without harming fungal elements Iodine Stain • Used for examination of parasitic helminths in stool • Stained egg in fecal specimen Class Assignment • Textbook Reading: Chapter 6 Specimen Collection and Processing • Key Terms • Learning Assessment Questions