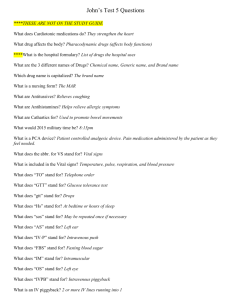
IV Priming/IV Medications
advertisement

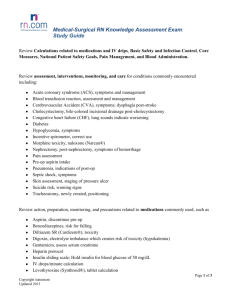
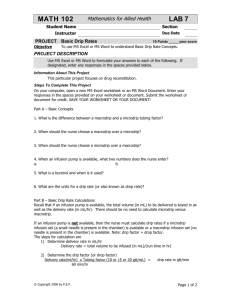
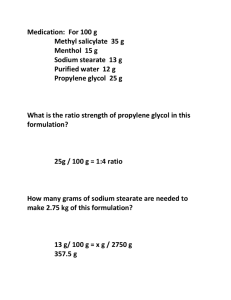
Chapter 27 (Perry & Potter) IV Priming Why do clients need an IV? Replacing fluids Correct or prevent nutritional imbalances Provide IV medication therapy Nursing Responsibilities 1. Know the correct solution & equipment needed & how to initiate the infusion 2. Regulate the infusion (with or without a pump) 3. Care for an maintain the system 4. Indentify and correct problems 5. Discontinue the infusion Categories of IV solutions 1. 2. 3. Isotonic Hypotonic Hypertonic Determined by serum electrolyte values and fluid volume balance RN must understand the rationale for IV fluid administration and the type of solution ordered Establish IV Access IV catheter can remain in place for 96 hrs (check hospital policy, most are 72 hours), IV solution replaced every 24 hours Palpate insertion site daily and prior to initiating infusion Inspect site if client c/o pain at site or developed S&S of infection Change transparent dressing if becomes damp, soiled, loose Clean injection port with antiseptic before accessing system Supplies Administration set (IV lines) Correct IV solution Antiseptic swabs Tape IV pole, rolling or ceiling mounted Hospital gown with snaps 1-3 ml normal saline, 3 ml syringe (or larger)…prefilled n/s syringes may be available, to flush IV catheter prior to initiating infusion Nursing Diagnosis Risk for imbalanced fluid volume Deficient fluid volume Excess fluid volume Risk for infection Assessment Review physician’s order (type, amount and/or rate) 6 medication rights (medication, dose, client, route, time, documentation) Physical assessment pertaining to IV fluid administration Understand rationale and purpose of IV fluid, potential incompatibilities, and potential side effects Implementation Change gown Prepare tubing and solution Check solution (6 rights) Color Clarity Expiration date Leaks Open infusion set (maintaining sterility of each end) Place roller clamp 2-5 cm below drip chamber and move to OFF position Remove sheath over port on IV solution bag Remove tubing spike (DO NOT TOUCH) Insert spike into IV bag Priming: Compress drip chamber, fill 1/3 to ½ Remove cap on end of tubing, KEEP and maintain sterility Slowing open roller clamp and prime tubing with fluid, return roller clamp to OFF position Inspect for air bubbles, tap tubing where bubbles are visible, and invert ports and tap to fill and remove air Replace cap from end of tubing Label tubing and bag with date and time Prepare n/s (1-3 ml) to flush intermittent infusion device (saline lock, PIID, clave) (p. 749 – establish IV access, pictureA) Saline lock is attached to end of IV catheter which is then attached to the primary line Has a port or stopper (needleless) Must be irrigated q8-12 h, and before & after each drug infusion (hospital policy) Saline or heparinized saline (hospital policy) Sterile technique Regulating IV Flow Rate (Gravity) Flow rate established using pump (ml/hr) or gravity (gtt/min) If line patent and IV infusion initiated, flow rate must be established Educate client regarding positioning Inspect site often What is the drop factor: number of drops per ml (gtt/ml) IV tubing provides: Microdrip: 60 gtt/ml Macrodrip: Abbott: 15 gtt/ml Travenol: 10 gtt/ml McGaw: 15 gtt/ml Calculating drip rate: ml/hr x gtt/ml 60 min = drops/min If ml/hr unknown: ml/hr = total infusion (ml) hours of infusion Remember: if infusion is not exactly 1 hour (15 min, 30 min, 120 min, etc…) you must calculate hourly rate. 50 ml x ? 15 min 60 min = 200 ml hr Example: Order: D5W @ 75 ml/hr Drop factor: 15 gtt/ml Calculate drip rate: ? gtt/min Answer: 75 ml/hr x 15 gtt/ml = 18.75 gtt/min 60 minutes (18-19 gtt/min) Example: Order: Give 1 L Ringer’s Lactate over 4 hours Drop factor: 15 gtt/ml Calculate drip rate: ? gtt/min Answer: 1000 ml x ? 240 min 60 min = 250 ml hr 250 ml/hr x 15 gtt/ml = 62.5 gtt/min 60 minutes (62- 63 gtt/min) Establishing Drip Rate Count drops in drip chamber for 1 minute (with second hand), adjust roller clamp as needed (2-5 cm below drip chamber) If very fast or very slow, count for 30 sec (x 2) and adjust roller clamp. Count for 1 full minute once clamp is adjusted . Evaluation Monitor infusion at least q1h (note volume, rate) Assess for S&S of overhydration or dehydration, response, lab values Assess S&S of infiltration, inflammation, clot in catheter, kink or knot in tubing etc… Recording and Reporting Rate of infusion, gtt/min, and ml/hr in nursing notes or IV fluid form Document any ordered changes in IV fluid rates Report rate, solution, volume remaining to the nurse assuming care of client at break or change of shift Practice Priming Chapter 21 (Perry & Potter) Piggyback (p. 737) A small IV bag connected to short tubing that is connected to the upper Y port of a primary infusion line. The small bag is set higher than the primary infusion bag. Upon completion of the secondary solution when the solution in the tubing falls below the primary drip chamber the primary solution begins again. IV Medication Secondary line (piggyback) Prepare medications: 6 rights and 3 checks Medical history & allergies Review medication indication Drugs prescribed 1 to 6 times per day, dissolved in small volumes of IV fluid Usual infusion time : 30 to 60 minutes Check compatibility of drug to solution When mixing powders for injections, remember: •Check the type of fluid recommended to dissolve the powder •The amount of fluid to add •The strength of the solution made (mg/ml) •Further dilution for infusion •Infusion time Where to find information regarding reconstitution of the powder •The label of the vial •Package insert inside the vial package •Nursing Drug book •Compendium of Pharmaceuticals and Specialties ( CPS) •Parenteral drug manual Medication Calculation Example: Order: Drug 0.65 g QID IV Label directions : Add 2.5 ml water for injection. Provides approx volume of 3 ml (325mg/ml) Note : the manufacturer gives the strength of the solution Desire 0.65g Have: 325 mg/ml Stock : in every ml Desire: 0.65 g Have: 325 mg/ml Stock : in every ml Convert: 0.65g to mg 1g = 1000 mg ( therefore answer should be bigger) 1000mg = Three zeros Therefore move decimal point three spaces to the right 0.65 g = 650 mg Desire X Stock = Amount Have 650 mg 325 mg X 1ml = 2mL Calculation of Drip Rate Example: Order: Flagyl 500mg/100 ml normal saline IV BID (administered over 1 hour) Drop factor: 15 gtt/ml Calculate drip rate: ? gtt/min Answer: 100 ml x ? 60 min 60 min = 100 ml/hr x 15 gtt/ml = 25 gtt/min 60 minutes 100 ml hr When calculating IV rates, if the medication volume exceeds 5 – 10 ml, add this into calculations Example: Amount: 100 ml NS plus 8 ml penicillin=108 ml Duration: Give over 30 minutes Calculate rate: ? ml/hr Answer: 108 ml x ? = 216 ml 30 min 60 min hr Let’s Practice (vial containing a powder) p.706 Reconstitution of medication Adding to secondary bag Attaching secondary line to primary line Regulating rate Follow 6 rights and 3 checks Wash hands Gather supplies Medication, secondary line,10 ml syringe, 18-22 gauge needle (filtered if indicated), alcohol swabs, dilutant (saline or sterile water), mini bag (medication bag), medication label, MAR Order Ampicillin 500 mg IV, q6h See vial for directions: to have 500 mg/ml add 5.6 ml dilutant IV drug manual indicates: add to 50 - 100 ml normal saline and infuse over 60 minutes How many ml of medication will you add to your minibag? What is the rate (ml/hr)? What is the drip rate with drop factor of 15 gtt/min? Answers: 50 ml X ? = 50 ml 60 min 60 min hr gtt/min = 50 ml/hr X 15 gtt/min = 12.5 gtt/min 60 min (12-13) 100 ml X ? = 100 ml 60 min 60 min hr gtt/min = 100 ml/hr X 15 gtt/min = 25 gtt/min 60 min Preparation Remove cap covering medication and dilutant (6 rights, 3 checks), swab both rubber seals with alcohol swab and allow to dry Attach needle (or needleless device) to syringe, pull back on plunger drawing the equivalent amount of air (i.e. 5.6 ml) as solution and inject into solution (hold plunger firmly, vial on flat surface) Invert vial and allow pressure from the vial to fill syringe with solution (5.6 ml), pull back gently if required. Keep tip of needle in fluid. Place vial on flat surface to remove needle Inject dilutant into medication vial, remove needle and recap (scoop technique) Roll in palms (DO NOT SHAKE) Wait until medication is clear, swab medication bottle again, and withdrawal desired amount (follow same steps as withdrawing dilutant (inject equal volume of air (i.e.1 ml) as medication to be removed) Add medication to secondary bag, wipe port with alcohol swab, lay medication bag on flat surface, insert needle and inject. Discard needle (no need to recap) Mix medication turning gently end to end Complete medication label (apply to back of medication bag) Spike bag with secondary IV tubing, ensure clamp is CLOSED Clean port of main line and connect secondary tubing to medication bag, squeeze and fill drip chamber. Back prime: drop medication bag below level of primary drip chamber, open secondary line roller clamp, prime line, hang medication bag above primary fluid bag (use hook to lower main bag) Regulate flow by adjusting regulator clamp or using IV pump Observe for S&S of reaction Assess IV site frequently Order Ampicillin 500 mg IV, q6h See vial for directions: 500 mg/ml add 5.6 ml solution IV drug manual indicates: add to 50 - 100 ml normal saline and infuse over 60 minutes Answers: 50 ml X ? = 50 ml 60 min 60 min hr gtt/min = 50 ml/hr X 15 gtt/min = 12.5 gtt/min 60 min (12-13) 100 ml X ? = 100 ml 60 min 60 min hr gtt/min = 100 ml/hr X 15 gtt/min = 25 gtt/min 60 min Next Lab Subcutaneous Injection & Insulin Chapter 21