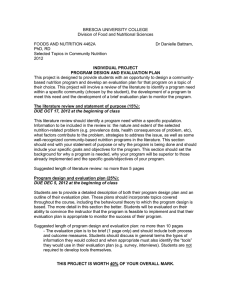
Total Parenteral Nutrition (TPN) Presentation
advertisement
In the name of GOD Total Parenteral Nutrition (TPN) Presented by: 1 Shadi Farsaei (Assistand professor of pharmacotherapy) INDICATION Inability to absorb nutrients via the GI tract because of one or more of the following: Massive small bowel resection Intractable vomiting when adequate EN is not expected for 7-14 days. Severe diarrhea Bowel obstruction GI fistulae: PN is indicated for patients with prolonged inadequate nutritional intake longer than 5-7 days who are not candidates for EN. 2 Cancer: antineoplastic therapy, radiation therapy, or HSCT moderately to severely malnourished patients receiving active anticancer treatment who are not candidates for EN. PN is unlikely to benefit patients with advanced cancer whose malignancy is unresponsive to treatment. PN is appropriate for patients undergoing HSCT who are malnourished and who are anticipated to be unable to ingest and/or absorb adequate nutrients for 7-14 days. Pancreatitis: severe pancreatitis with prolonged inadequate nutritional intake longer than 5-7 days who are not candidates for EN. PN should be used when EN 3 exacerbates abdominal pain, ascites, or fistula output. Critical care whom EN is contraindicated or is unlikely to provide adequate nutritional requirements within 5-10 days. Organ failure (liver, renal, or respiratory): moderate to severe catabolism when EN is contraindicated. Burns: whom EN is contraindicated or is unlikely to provide adequate nutritional requirements within 4-5 days. Perioperative PN Preoperative: for 7-14 days for patients with moderate to severe malnutrition who are undergoing major GI surgery, if the operation can be safely postponed. Postoperative: for patients in whom EN is 4 contraindicated or is unlikely to provide adequate nutritional requirements within 7-10 days. Eating disorders: anorexia nervosa and severe malnutrition who are unable or unwilling to ingest adequate nutrition. 5 Adult PN therapy is not an emergent intervention and should not be initiated until the patient is hemodynamically stable. In general, adults who are not candidates for enteral nutrition should be considered candidates for PN after 7 to 14 days of suboptimal nutritional intake. 6 PATIENT ASSESSMENT Nutrition History: malnutrition Weight History 5% of usual weight within 1 month, or 10% of usual weight within 6 months Physical Examination Anthropometry Biochemical Assessment 7 Visceral Proteins for Nutrition Assessment 1. Brown RO, Bradley JE, Bekemeyer WB, Luther RW. Effect of albumin supplementation during parenteral nutrition on hospital morbidity. Critical care medicine. 1988;16(12):1177-82. 2. Koretz RL. Intravenous albumin and nutrition support: going for the quick fix. JPEN Journal of parenteral and enteral nutrition. 1995;19(2):166-71. 3. Rubin H, Carlson S, DeMeo M, Ganger D, Craig RM. Randomized, double-blind study 8 of intravenous human albumin in hypoalbuminemic patients receiving total parenteral nutrition. Critical care medicine. 1997;25(2):249-52. PERIPHERAL LINE 700-900 mOsmol Chang IV each 2-3 d Dextrose 10% Aminoacid 5% Intralipid ? Energy < 1 kcal/ml Dilution of dextrose/aminofusion with Intralipid 9 PARENTERAL NUTRITION Peripheral Parenteral Nutrition (15 lit D5W/day for a 70 kg Central Parenteral Nutrition (TPN) - needs CV-line to administer hyperosmolar solutions !!!) Osmolarity: (%Dex × 50) + (%Aminoacid × 100) 150 mOsm for electrolytes, … 10 Subclavian PICC Jugular Femoral (more infection !) PICC: Peripherally inserted central catheter 11 12 13 PERIPHERAL VEIN THROMBOPHELEBITIS Hydrocortisone 5 mg/L Heparin 1000 U/L Topical nitroglycerin Concurrent administration of intralipid ? Decreases osmolarity, buffers the pH, and improves peripheral vein tolerance, it does not eliminate the risk of thrombophlebitis. 14 ESTIMATION OF ENERGY EXPENDITURE Weight & metabolic state Harris-Benedict equations: BEE (M) (kcal/day) : 66.47+13.75W+5H-6.76A BEE (F) (kcal/day) : 65.51+9.56W+1.85H-4.68A BEE: 20-25 kcal/kg/day TEE (kcal/day): BEE × Stress factor × Activity factor 15 Stress factors: Surgery: 1.1-1.2 Infection: 1.2 Trauma: 1.5 Sepsis: 1.6 Burns: 1.6-2 Activity factors: Confined to bed: 1.2 Out of bed: 1.3 Normal activity: 1.5 16 Estimation of protein requirement Hypermetabolic/hypercatabolic state secondary to trauma or burn: 2 g/kg/day 17 COMPONENTS OF TPN FORMULATIONS Macro: Calorie: Dextrose 20%, 50% Intralipid 10%, 20% Protein: Aminofusion 5%, 10% Fluid Micro: Electrolytes (Na, K) Minerals (Mg, Ca, PO4) Trace elements (Zn, Cu, Cr, Mn, Se) Vit (A, E, C, B, Folic acid) 18 19 20 21 DEXTROSE 20%, 3.4 50% (from CV-line) kcal/g 60-70% of calorie requirements should be provided with dextrose 22 SPECIAL CONSIDERATIONS Max infusion rate of dextrose: 0.5 g/kg/h (to avoid hyperglycemia, glycosuria, fatty liver, hyperosmolar coma) Max rate of dextrose metabolism : 5 mg/kg/min or 7 g/kg/d “K” should be added to dextrose solutions If BS > 200, Insulin should be added 0.1 U/g Dextrose 23 AMINOFUSION 5%, 10% (from CV-line) 1-1.5 g/kg/day Should not be used as a calorie source 24 ESTIMATION OF PROTEIN REQUIREMENTS 0.8 g/kg/day RDA Hospitalized patient, minor stress Moderate stress 1.2–1.5 g/kg/day Severe stress 1.5–2 g/kg/day 1–1.2 g/kg/day 25 26 27 28 Na K Mg Acetate Cl H2PO4 43 25 2.6 59 57 9 mmol/L mmol/L mmol/L mmol/L mmol/L mmol/L 29 30 INTRALIPID 10%, 20% (from peripheral or CV-line) 30-40% of calorie requirements should be provided with Intralipid Serum Max. TG level must be < 400 mg/dl 2.5 g/kg or 60% total calories 31 1022 Kcal/L 345 mOsmol/L 32 1080 Kcal/L 1 liter contains: A- Active constituents: Glycerine (glycerol) 25g Phospholipids from egg 6g Soya beans 100g B- Other Constituents: Sodium Oleate, Sodium hydroxide & water Total energy= 1080Kcal/L 33 34 AN IMPORTANT SOLUTION Concentrate Source isotonic solution of essential FFA Substitute for CHO for ventilated pts. 35 Caloric density of intravenous nutrients 36 Electrolytes (daily requirements for TPN): 37 38 Recommended adult daily dose of parenteral vitamins 39 AVAILABLE DOSAGE FORM FOR PARENTERAL ROUT Amp Vit A: 50000 IU Amp Vit D: 300,000U Amp Vit K: 1, 10 mg ??!! Amp Vit E: 100 IU Amp Vit C: 500 mg Amp Vit B complex Amp Vit B12: 100, 1000 mcg Amp Soluvit (Fressenius) 40 41 42 43 44 VITALIPID INDICATIONS Vitalipid N Adult is indicated as a supplement in complete intravenous nutrition to meet the daily requirements of the fat-soluble vitamins A, D2, E and K1. As above, Vitalipid N Infant is indicated in paediatric patients up to 11 years of age. 45 The vitamins are soluble in the oil phase of the emulsion, which has the composition corresponding to that of Intralipid 10%. The daily maintenance dosage of the vitamins A, D2, E and K1 are supplied during intravenous nutrition when: (i) 10 mL of Vitalipid N Adult are added to 500 mL Intralipid 10% or 20%. (ii) 1 mL of Vitalipid N Infant per kg bodyweight per day up to a maximum of 10 mL is added to Intralipid 10% or 20%. 46 47 48 49 50 51 The recommended dose is 1 mL Peditrace/kg body weight/day for infants and children with a weight of up to 15 kg. The basic requirements of trace elements are covered by a daily dose of 15 mL to children weighing more than 15 kg Infusion time: The infusion time should not be less than 8 hours. The infusion should be given at a very slow rate. 52 WATER ml/day = 1500 ml + (IBW-20) × 20 30-35 ml/kg Average healthy adult : 5 L/d Fluid restricted: ≤ 2 L/d Emesis, diarrhea, agitation, ventilation, fever 53 54 55 MONITORING: Baseline: Wt, Na, K, BUN, Cr, Glu, Ca, P, Mg, CBC, PT, INR, TG, LFT, Alb Daily: Wt, V/S, I/O, Na, K, BUN, Cr, Glu 2-3 times a week: CBC, Ca, P, Mg Weekly: Alb, LFT, INR 56 REFERENCES Mirtallo, 57 J., D. Johnson, et al. (2004). "Safe practices for parenteral nutrition." Journal of Parenteral and Enteral Nutrition 28(6): S39-S70. Koda-Kimble, Mary Anne, and Brian K. Alldredge. Applied Therapeutics: The Clinical Use of Drugs. Baltimore: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2013. DiPiro, Joseph T. Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw-Hill Medical, 2011. …..