cns-developmental-abnormalities
advertisement

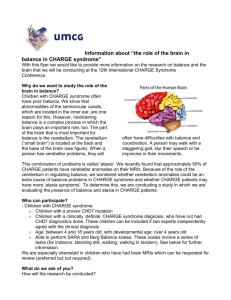
CNS Pathology Introduction & Congenital Abnormalities • 2% body Wt but 20% Oxygen. • Hypoxia First to get affected. • No regeneration – Permanent cells. • Fluid tissue… Floats in CSF. • Very delicate, less support. • Limited space - Hard bony shell. Congenital Abnormalities Immature Brain • Premature and very young fetuses have few convolutions. The primary sulci are the calcarine, parietal-occipital, and central sulci. They appear by about gestational age 20 weeks. • After that particularly after 25 weeks gestation secondary convolutions are formed: The pre and post central, superior temporal, and frontal gyri • After 28 weeks there is a more brain specific formation of the secondary and tertiary convolutions. The premature brain does not have any myelin except in the tegmentum of the brainstem. • Myelination of the corticospinal tracts is seen at about 39 weeks gestation. The entire premature and term infant brain appears white. I. GENERAL POINTS • The incidence of malformations is higher in children with intrauterine growth retardation and in multiple pregnancies. • Race and geographic factors may be of importance. • The development of the brain continues for years after birth and thus the term congenital anomaly applies to some brain conditions that develop postnatally. • Inflammatory responses do not occur before the sixth fetal month and parts may be absorbed without trace of neuroglial or connective tissue repair. • The same anomaly may occur as a result of genetic or environmental causes. • Probably the most important factor in teratogenesis is the timing of the insult, followed by the specific nature of the agent and genetic factors. • The incidence of CNS malformations, giving rise to mental retardation, cerebral palsy, or neural tube defects, is estimated at 1% to 2%. • Malformations of the brain are more common in the setting of multiple birth defects. • Prenatal or perinatal insults may either cause failure of normal CNS development or result in tissue destruction. • Because different parts of the brain develop at different times during gestation (and afterwards), the timing of an injury will be reflected in the pattern of malformation. II. ETIOLOGY • Genetic Factors: very few cerebral anomalies are caused by simple Mendelian inheritance, but some examples include: – Forms of microcephaly inherited as autosomal recessive – Sex-linked variety of hydrocephalus – Hereditary congenital facial paralysis- autosomal dominant – Some anomalies have a high risk of recurrence within families – Some anomalies are associated with inborn errors of metabolism • Cytogenetic Abnormalities – Most important group are the trisomies, e.g., Down's – Others include translocations, deletions (e.g., cri du chat), and sex chromosomes (e.g., Turner's, Klinefelter's) • Maternal Age • Maternal Infections (rubella, CMV). Different patterns of malformation correlate with mishaps (known or unknown) at different time: • Idiopathic (most of cases) • Known causes include – maternal alcoholism, – mercury poisoning, – lead poisoning, – radiation, – exposure to vincristine – folic acid deficiency – hypervitaminosis. III. Neural tube defects • Among the earliest stages in brain development is the formation of the neural tube, the inside of which will become the ventricular system and the wall of which will become the brain and spinal cord. • Failure of a portion of the neural tube to close, or reopening after successful closure, may lead to one of several malformations. • All are characterized by abnormalities involving some combination of neural tissue, menginges, and overlying bone or soft tissues. • Collectively, neural tube defects are the most frequent CNS malformations III. NEURAL TUBE DEFECTS (DYSRAPHIC DISORDERS) • Anencephaly – Basically a complete absence of the cerebral hemispheres. – The calvarium is hypoplastic or absent. – If the occipital bones are formed, rudimentary brain stem and cerebellum may be found. – Most common anomaly in humans. Anencephaly • Encephalocele and Cranial Meningocele – Consists of a protrusion of brain or meninges through a cranial defect. – Most frequent in the occipital region, i.e., 75-80% of cases. – The mass of tissue is often voluminous and is usually attached to one of the cerebral hemispheres by a narrow pedicle. – Genetic and environmental factors may be of etiologic importance. • Spinal Meningocele, Myelomeningocele, and Myelocele – All are usually associated with spina bifida. Meningocele consists of herniation of both dura and arachnoid through a vertebral defect, the spinal cord remaining in its normal position. – Meningomyelocele consists of the above in addition to the spinal cord (closed) being herniated as well. – Myelocele consists of all the above, but the spinal cord is open and flat with CSF leaking onto the exposed surface. – Hydrocephalus commonly occurs in association with all of the above. IV. ARNOLD CHIARI MALFORMATION • Complex Deformity of the Brain and Cerebellum (Four types): – Type I: LESS SEVERE FORM • Ectopia of the cerebellar tonsils. • May be a cause of late onset hydrocephalus, • May be associated with a minor deformity of the medulla. – Type II: MOST COMMON TYPE • By far the most common type seen in neonates • Usually associated with a lumbar myelomeningocele • Consists of lengthening of the vermis and tonsils of the cerebellum and their downward displacement through the foramen magnum into the spinal canal. • Characteristic Z shaped kink at the junction of the medulla and cord. • Cranial vault anomalies. – Type III: VERY RARE TYPE • Cervical spinal bifida, • the entire cerebellum being herniated through the foramen magnum. – Type IV: • Cerebellar hypoplasia. • cerebellar tonsils herniating through the foramen magnum• a characteristic of ArnoldChiari malformation • ACM (in practice this refers to type II) usually associated with communicating hydrocephalus. • The malformation develops early in gestation at the age of 10 weeks. Clinical Correlation The Arnold Chiari malformation may be associated with normal intellagence (if the hydrocephalus is shunted) or mental retardation. It is also associated with lower limb paralysis and urinary and fecal incontinence due to the meningomyelocoele. Type I can cause neck pain and cranial nerve signs and may sometimes have to be treated with surgical decompression. V. ANOMALIES OF THE SPINAL CORD Usually these are described in the adult, so they could represent acquired lesions. • Hydromyelia: is an over distension of the central canal. (Local dilatation of the central canal of the spinal cord.) – in the lumbar region – may be asymptomatic and only an incidental finding at autopsy – may be associated with ACM in 40% of cases of the latter. • Spina bifida (congenital anomaly) – Defective closure of the vertebral column. – Spina bifida is one of the most serious neural tube defects compatible with prolonged life. – Its severity varies from the occult type with no findings to a completely open spine (rachischisis) with severe neurologic disability and death. – In spina bifida cystica, the protruding sac can contain meninges (meningocele), spinal cord (myelocele), or both (myelomeningocele). – Spina bifida is most common in the lower thoracic, lumbar, or sacral region and usually extends for 3 to 6 vertebral segments. – The sac in a myelomeningocele usually consists of meninges with a central neural plaque. If not well covered with skin, the sac can easily rupture, increasing the risk of meningitis. VI. MALFORMATIONS OF THE CEREBELLUM • Agenesis of the Cerebellum: uncommon • Hypoplasia • Dandy Walker Malformation (absence of cerebellar vermis and dilatation of 4th ventricle) • L'hermitte Duclos Disease (Dysplastic granulomolecular hypertrophy of the cerebellar cortex) VII. HOLOPROSENCEPHALY (ARHINENCEPHALY) • Covers a large spectrum of anomalies from cyclopia to agenesis of one olfactory bulb. • In the most severe form, there is an anterior holosphere with no interhemispheric fissure and a single ventricle. • The brain is often smaller than normal and the olfactory bulbs and tracts are absent. • Optic nerves are absent and gyri are broad and have an abnormal pattern. • Brain stem and cranial nerve structures may be normal. Semilobar holoprosencephaly Face of an infant with semilobar holoprosencephaly •Shows closeset eyes, absent nose and abnormal mouth often seen in this form of holoprosencephaly A single large ventricle with fusion of midline structures, including thalami. The affected fetuses and neonates typically have severe facial defects, such as cyclopia, as well. Underlying chromosomal abnormalities, such as trisomy 13, or maternal diabetes mellitus are possible causes, but some cases are sporadic. • The large single ventricle seen here inside a single hemisphere represents the "alobar" form of holoprosencephaly in which there was no division of hemispheres. • Cyclopia and agnathia are the major facial associations. • Rhinencephaly is characterized by a proboscis-like nose above a single median eye. Cyclopia is also known as synophthalmia, which is the fusion of the eyes THE PROBOSCIS MONKEY VIII. ANOMALIES OF CELL MIGRATION • Ectopias and Heterotopias: These terms refer to misplaced groups of neurons, such as an island of gray matter in the subcortex. – More common in the cerebellum than the cerebrum. • Cerebellar Cortical Dysplasia. IX. ABNORMAL SURFACE CONFIGURATIONS OF THE BRAIN • Agyria (lissencephaly): Total absence of gyri • Pachygyria: A few broad malformed gyri varying in size and number • Polymicrogyria: An increased number of gyri some of which may be abnormally small. • This is a horizontal section of a microcephalic brain which shows areas of no convolutions lissencephaly or smooth brain and areas of large gyri -pachygyria. • Note how thick the cortex is and how thin the white matter characteristic of lissencephaly and pachygria • Coronal section through this brain shows the cortex to be thrown into numerous small gyri characteristic of polymicrogyria. • Note the enlarged ventricles and small size of the white matter. • These patients are usually retarted and may have seizures or other neurologic findings X. MICROCEPHALY • Small brain usually associated with a small head. Brain Weight < 900 g. • Congenital microcephaly may follow intrauterine infections with rubella, CMV, Toxoplamosis. • Congenital microcephaly is also a part of many chromosomal abnormalities and other syndromes: Gross chromosomal abnormalities • Trisomy 18 • Trisomy 13 • Wolf-Hirschhorn syndrome • Cri du Chat syndrome • Partial deletion of long arm of 13 Contigous gene syndromes • Miller-Dieker syndrome • Langer-Giedion syndrome • Prader-Willi syndrome • Aniridia-Wilms tumour syndrome Autosomal recessive disorder • JohansonBlizzard syndrome • Seckel syndrome • Smith-LemliOPitz syndrome • Coffin-Siris syndrome Rubinstein-Taybi syndrome Maternal PKU Coronal sections through to half brains at the level of the thalamus showing a normal adult brain on right and a smaller, microcephalic brain on left. XI. MEGALENCEPHALY Macrencephaly • Proportionate enlargement of the whole brain, usually associated with the presence of a variable mental aberration. • Well-formed, but too big (>1800 gm). Causes: – tuberous sclerosis, – cerebral lipidoses, • Alexander's leukodystrophy. • Unilateral megalencephaly or hemimegalencephaly is a rare condition and is characterized by the enlargement of one-half of the brain. – Children with this disorder may have a large, sometimes asymmetrical head. – Often they suffer from seizures and mental retardation. XII. AGENESIS OF THE CORPUS CALLOSUM • May be part of a complex malformation or be totally or partially absent in an otherwise normal brain. • Patients can be of normal intelligence but lack ability to transfer information from one hemisphere to the other XIII. NEUROCUTANEOUS SYNDROMES • • • • Tuberous Sclerosis von Hippel Lindau's Angiomatosis Sturge Weber Syndrome von Recklinghausen's Disease • This is tuberous sclerosis, an autosomal dominant condition characterized by mental retardation and seizures beginning early in life. The characteristic feature is the presence of "tubers" which are enlarged and firm, whitened gyri. A "tuber" is seen at the arrow. • Syringomyelia / syringobulbia: – Probably acquired later in life, but discussed here. – There is a tubular cavity in the center of the cord (generally cervical) and/or brainstem (bad), with surrounding gliosis. – There is loss of pain and temperature (since the crossing spinothalamic tract is damaged) over the corresponding levels. – Eventually, other sensory and motor pathways may be damaged. – Most often these conditions are idiopathic; known causes include cord tumors and Arnold-Chiari. • Neuroepithelial cysts probably arise from faulty migration during embryogenesis. They gradually grow, and become symptomatic in adult life. – The best-known are the "colloid cysts" that occlude the foramen of Munro, often causing headache only when the head remains in a particular position. • Arachnoid cysts may be large and require surgical removal. • Cerebral palsy: a brain defect present at (or presenting shortly after) birth, typically with motor and often cognitive problems. Thank you!