Dysphagia Final Exam Notes - My Professional Portfolio
advertisement
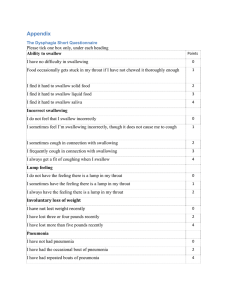
The rest of Banajee’s pediatric dysphagia lecture… Evaluation for dysphagia o Instrumentation Modified barium swallow study- or you can recommend FEES o Videoflouroscopy o Food coated with barium is ingested o Head and body in different positions o Views recorded for later analysis o Real-time visualization of the swallow process o Determine whether the individual is safe to be fed orally or not Fiber-optic endoscopic evaluation of swallowing (FEES) o Following topical anesthetic insert a flexible fiber-optic laryngoscope through the patient’s nose and down into the pharynx o Cough, hold his breath, swallow different textures of food (dyed for visualization) o Oral and esophageal phase not visible o Videoflouroscopic swallow study Responsibilities of the feeding specialist o Positioning of the infant/child o Assembling the feeding equipment o Instructing the parents who act as feeders during the study o Assuming the role of the feeder o Working with radiologist to obtain an optimum view o Helping infant/child to maintain midline head position o Evaluating stages of swallow o Making suggestions for intervention and compensatory strategies o For radiation part for infant- shouldn’t be longer than 3-5 minutes. Don’t want to expose child to radiation for longer than that. Responsibilities of the radiologist o Reviewing the films o Diagnosing anatomical abnormalities o Assessing adequacy of airway protection and swallowing parameters in conjunction with feeding specialist o Screening esophageal phase o Reviewing video tape with feeding specialist to discuss objective findings Time 2-3 mins because of hazardous radiation Getting started o Be sure the child is hungry- the first thing you want to do! Have to tell the parents not to tube feed for about 2-3 hours before o Make feeding as familiar and natural as possible (familiar utensils) o Parent/primary caregiver should feed the child o Use simultaneous audio and video recordings to document techniques/flow rates o Universal precautions Positioning o Premature infants use small seat (Tumbleform with appropriate support for head/neck/trunk at a 45 degrees) At LEAST at 45 degree angle in Tumbleform chair o For full term infants use larger seats or special seats such as a MAMA chair (multiple application, multiple articulation) 1 Evaluation (cont.) o Materials Several nipples and bottles Poor feeders need to increase the flow rate- do you need to slow the rate or increase the rate for the kid? Her preference is a cross cut (esp for kids with cleft palate). When you turn it upside down you should get ONE drop out of the nipple- shouldn’t be a large flow, shouldn’t be nothing coming out of it either Slow rate – 3.6ml/minute Fast rate – 16.2 ml/minute Have glucose, formula or breast milk that is not mixed with barium to continue with feeding between evaluations Hardest to the easiest consistencies of food o ***The hardest for a child would be thinner liquids- easiest to aspirate Various cups can be used Straw- for older child Spoons (one shallow bowl) Syringe- to get behind a tongue thrust Pacifier Picture o Lambs nipple: pliable and soft; nook nipple: broad tip. Primy nipple: can go nicely behind tongue thrust, very thin. Nosy cup: accommodates for the nose so child can just tilt cup… but you can only fill so much liquid in it. Sippy cup: banajee not a big fan, but she likes the handles. Bottles: she loves the honey bear, good to teach straw drinking. You decrease your squeeze and the child learns to suck more. Regular bottle: you don’t see plastic liner- this is ideal to use for cleft lip/palate. Cleft: they suck in a lot of air. A plastic liner squeezes as you make the child drink- less air will go in their oral cavity. Also you’d want to think about the liner for a colicke child, or for a child you need to feed in an upright position. Cleft palate positioned more upright. Curved bottle helps you feed child o Videoflouroscopic swallow study NNS- non nutritive suckle NS- nutritive suckle Procedure o Presentations For infants start with NNS- non-nutritive child: use a nipple, pacifier. DO NOT use an empty bottle- because of the air Introduce nipple feedings using regular or preemie nipple w/ regular flow rate Older children liquids may be presented via a spoon (2 ml) Increase quantity (if there is no problem) and texture and vary the utensils For infants with NPO – start opposite way around! - Start with easiest consistencies- make sure no penetration/asp ***CEREAL good to thicken liquid up for infant! - Establish NNS - Introduce familiar bottle feeding and compare nutritive suckle (NS) and non nutritive (NNS) - With older children begin with spoon feedings - Instruct parents/caregivers to feed infant the same way as they do at home 2 o Interpretations/recommendations Infants trigger at the vallecula by tongue pressing the posterior pharyngeal wall Tongue back/down movement is more posterior than in older children o More posterior in younger child Some infants may experience ventricular penetration during the initial suckle burst This penetration will clear after the first few swallows if normal o Videoflouroscopic swallow study Oral phase o Suckling from a nipple Latching on to nipple with a tight lip or tongue seal Initiates suckling Rhythmical suckling 1-2 sucks per swallow/breath Stripping the nipple Nipple compression Posterior nipple placement o Removing food from a spoon Mouth opening Closure around spoon Lip assistance to remove food- we don’t want to scrape it off their upper lip Masticating (or munching) or mashing between gums or tongue and hard palate - Munching: pushing tongue against upper lip and mashing the food - Rotary chew: side to side Manipulate the food from side to side to form a bolus Holding food in midline on dorsum of the tongue in preparation for the swallow Utensil use – spoon, fork, cup etc. o Posterior transit of the bolus o Oral transit time from the first posterior movement until the bolus reaches the head of the ramus of the mandible o Lingual peristalsis with hard and soft palate o Soft palate simultaneously with the triggering of the swallow response Pharyngeal stage o Begins with elicitation of swallow response and ends with bolus passing the CP (CRICOPHARYNGEAL) segment and then passing through esoph o Laryngeal elevation and anterior movement o Epiglottic excursion o Pharyngeal contraction, **YOU SHOULD SEE no residue- important because residue could sit and cause aspiration later, because they don’t realize it’s present. o CP dilation Esophageal phase o Primary peristalsis- going all the way down o Secondary peristalsis- going into stomach o You want to see an emptying – you don’t want to see it go back up o Video Notes: 6 month old: Pooling in valleculae is okay because he is clearing it. First stop is vallecula then pyriform sinus Cleft palate kid: Came out through the nasopharynx- nasal regurgitation - Complete or partial - Palate closes from front to back. Cleft should start from back to front. They normally close between 9-12 mos - Surgeon may leave a fistula to make sure that there is growth - For a small fistula usually the food doesn’t come up 3 Dysphagia treatment o Feeding environment Minimize auditory and visual distractions Light not too bright or too dark NEVER force-feed!!!! Noise reduced, music encouraged. Caregiver should be relaxed and unhurried Arching back is a big sign of reflux! Respond to client signals regarding feeding speed, food choices, and quantity Communication strategies developed Utensils for feeding must be appropriate o Slow-flow nipple o Teflon coated spoon o Shallow bowled spoon o Cutout cups o Body positioning Body posture and stability Upright 90 degree hip angle, symmetrical position w/ postural support to provide stability Head and neck secure to prevent extraneous movements Chin tuck Head rotation o Modification of foods and beverages- CHART o Oral motor exercises and swallowing techniques Range of motion of the tongue exercises Lip strengthening exercises Cheek strengthening exercises Jaw exercises o Bubble blowing o Straw sucking o Dysphagia treatment Vital stimulation o Very controversial- don’t do if child is having seizures! o Delivered via a vital stim therapy unit o Biphasic current Each pulse contains 2 phases Current flows to an electrode and back again before stopping Polarity rapidly alternates btwn the electrodes causes depolarization of the peripheral motor nerve at neuromuscular junction causing muscle to contract Frequency of current is between 30 and 80 Hz depending upon child The greater the current- the greater the number of muscles you are stimulating o If problem with oral phase: want electrodes higher up towards omohyoid o If child is okay with oral, having probs w/ pharyngeal: placement B- lower down o If probs with both: do vertical (one in front and one at back) o D: child is older. One in front, one on sides, etc. the anatomy determines what the placement of the electrodes would be. o *PURPOSE: you get the swallow, start decreasing the current so that the person takes over. But doesn’t always work. Later do another MBSS to see if they have improvement. For child you may not repeat MBSS, depends on the case. 4 Dysphagia: Treatment Dysphagia Treatment o Thermal Stimulation Mixed evidence of efficacy Tapping or rubbing faucial pillars Iced dental Mirror (frozen Q-tip) o Right after stimulation – pt asked to swallow. o Can give small amount of liquid via spoon/straw Reportedly alerts Nervous System Suggested 3 X Day o Thermal Stim – Icing (more for frozen q-tips – rather than ice water soaked dental mirror) o Icing some areas could possibly have dangerous consequences for the elderly, the frail, or those with heart problems. (Icing these areas would not affect a young healthy person.) Above the mouth = sympathetic nervous system response which increases heart rate. This might cause plaque to break loose from a thrombus and lead to another stroke or to a heart attack. Behind the ear= lower blood pressure to dangerous levels in some patients. Near the pinna = can cause irregular heart beat and respiratory problems. o Sensory Stimulation Presenting a warm or cold bolus, presenting foods with strong tastes or textures, or pressing spoon on the tongue when food is presented (press against tongue – slide out) If apraxia of the swallow, best to let them feed themselves, allowing the swallow to be more automatic o Chewing Provides the extra oral sensation to trigger the swallow. If used, the patient must also chew liquids prior to swallowing them o Motor Exercises – Range of Motion (ROM) and Strength Improve of lips, tongue, jaw Improve vocal fold adduction Laryngeal elevation (glottal hold and higher pitch) Tongue base retraction. o Postures to Facilitate Swallow Head Down – If delayed swallow reflex (or initiation of swallow) Moves the tongue forward & enlarges vallecula Allows more time for the larynx to elevate and the vocal folds to adduct Narrows airway and puts the epiglottis in a more over-hanging position Poor tongue control Head back position (CAUTION). Dangerous – especially if liquids! Unilateral Paralysis of Pharynx Should turn head toward the paralyzed side before swallowing. o Closes the pyriform sinus on the bad side and keeps food on the functioning side of the pharynx Unilateral paralysis of oral cavity and pharynx Tilt head to strong side. Helps direct to strong side oral and pyriform o Pocketing/Pooling of bolus in oral cavity Teach Pt to sweep buccal cavity with finger Consistencies – next slides 5 National Dysphagia Diet (2002) o Level 1: Dysphagia Pureed Homogeneous, cohesive, Pudding-like, requires bolus control, no chewing required. o Level 2: Dysphagia Mechanically Altered Cohesive, moist, semi-solid, requires chewing. o Level 3: Dysphagia Advanced Soft-solid foods, requires more chewing. o Level 4: Regular All foods allowed. Consistencies – Poor Tongue Control o Thickened Liquids Prevent splashing – less free movement Consistencies – Problems in airway closure o Thickened liquids – travels more slowly, allowing more time for laryngeal elevation and closure Consistencies – Problems with upper esophageal sphinctor (UES) i.e., pharyngo-esophageal sphinctor. o Thinner consistencies better thin liquids can drain into the esophagus through even a small opening in the p.e. segment. also ask Pt to regulate the size of the bolus that they try to swallow. Have them take small bites. Techniques for Protecting Airway – o Here and below techniques – Pt needs cognitive ability sufficient to perform action. Thus, cognitive screening important! o Supraglottic Swallow take a breath and hold it while swallowing and then coughs after the swallow This results in the voluntary closure of the vocal folds before, during and after the swallow. o Supra supraglottic swallow same procedure as with the supraglottic swallow, but bear down while holding breath o Mendelsohn Maneuver Pt told to pay attention to the way the thyroid cartilage (Adam's apple) goes up and down during swallowing. Then he learns to use muscles to keep the larynx elevated for several seconds after the swallow. Facilitates the opening of the cricopharyngus muscle (PE sphincter). Helps the patient gain voluntary control over the opening and closing of the p.e. segment. o Effortful swallow squeeze hard with his throat and neck muscles during the swallow increases the tongue driving force by causing exaggerated retraction of the tongue helps get food past the valleculae REMEMBER - Here and above techniques – Pt needs cognitive ability sufficient to perform action. Thus, cognitive screening important! If mild cognitive deficit – can be coached through each swallow (what is functionality?) Dysphagia Treatment o Placement of Percutaneous Endoscopic Gastrostomy (PEG tube) o Nasogastrtic Tube (NG Tube) 6



![Dysphagia Webinar, May, 2013[2]](http://s2.studylib.net/store/data/005382560_1-ff5244e89815170fde8b3f907df8b381-300x300.png)