Lecture 19
advertisement

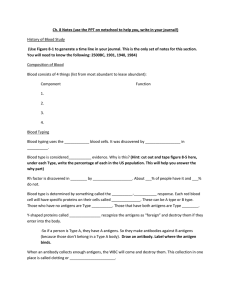
Chapter 17 Specific Defenses of the Host: The Immune Response Specific Defenses of the Host: The Immune Response •Acquired immunity - Developed during an individual's lifetime Distinct Cells in Adaptive Immune System • Lymphocytes (B cells, T cells) – Determining specificity of immunity • Specialized epithelial and stromal cells – Providing anatomic environment • APC (antigen presenting cells) - antigen presentation – mediation of immunologic functions – Monocyte/macrophage – Dendritic cells – Natural killer cells and other members of myeloid cells (leukocyte that is not lymphocyte) Blood cells differentiation Dual Nature of the Adaptive Immune System • Red bone marrow stem cells produce lymphocytes 1. B cells -Humoral immunity –Some lymphocytes that mature in red bone marrow become B cells. – Antibody production – Antibodies are found in serum and lymph. 2. T cells - Cell-mediated immunity – Some lymphocytes migrate through the thymus become T cells (T-lymphocytes) – Activation of macrophages, natural killer cells (NK) – Antigen-specific cytotoxic T-lymphocytes – Release of various cytokines in response to an antigen. Dual Nature of the Adaptive Immune System Immune system • The most important nature of immune system is self/non-self recognition. – Self/non-self recognition is achieved by having every cell of the body displays an individual specific marker. • Any cell not displaying this marker is treated as non-self and attacked. • The process is so effective that undigested proteins are treated as antigens. Major Histocompatibility Complex (MHC) • The major histocompatibility complex (MHC) is a set of cell surface molecules (proteins) encoded by a large gene family in all vertebrates. • On the cell surface, each MHC molecule displays a molecular fraction, called epitope, of a protein. – The presented antigen can be either self or nonself. – MHC population on the cell membrane gives information about the balance of proteins within the cell. • MHC molecules mediate interactions of leukocytes, with other leukocytes or body cells. • In humans, MHC is also called human leukocyte antigen (HLA). •MHC proteins transfer information about proteins within a cell to the cell surface Humoral Immunity • An antigen (Ag), or immunogen, is a chemical substance that when introduced into the body stimulates the production of specific antibodies (antibody generation) • Antibody (Ab) – A protein produced by B cells in response to recognition of an antigen – Protein made in response to exposure to bacteria and other pathogens, toxins, plant pollen and red blood cells that the body recognized as alien, or non-self. – Capable of combining specifically with that antigen. • Highly specific recognition of foreign antigens (non-self) – A vast universe of distinct antigenic specificities • Mechanisms for elimination of microbes bearing such antigens • Immunologic memory • Tolerance of self-antigens The Nature of Antigens • As a rule, antigens are proteins or large polysaccharides. – Only large molecules, infectious agents, or insoluble foreign matter can elicit an immune response in the body.) • A hapten is a small molecule that cannot cause the formation of antibodies unless combined with a carrier molecule; 1. Can elicit an immune response only when attached to a large carrier such as a protein. • The carrier may be one that also does not elicit an immune response by itself. 2. Once the body has generated antibodies to a hapten-carrier, the small-molecule hapten may also be able to bind to the antibody independent of the carrier molecule. The Nature of Antibodies • Antibody is a large Y-shaped protein an immunoglobulin (Ig) • They are secreted form of the B-cell receptor • The antibody recognizes a unique part of the antigen - epitope ( a portion of a molecule to which an antibody binds) or antigenic determinants. Figure 17.3 Antibody Structure • The Ig monomer consists of four paired polypeptide chains connected by disulfide bonds. – Two identical heavy chains – Two identical light chains • Each chain has two domains: one constant domain (C) and one variable domain (V) • The constant domains or C domains of the heavy and light chains make up the C region – The type of heavy chain present defines the class of antibody (IgA, IgD, IgE, IgG, and IgM) • The variable or V domains of the heavy and light chains together make up the V region of the antibody and confer on it the ability to bind specific antigen epitope. Figure 17.5a-c Ag-Ab Binding • Antigen-antibody complex – Affinity - the strength of the reaction between a single antigenic determinant and a single antibody – Specificity - Specificity refers to the ability of an individual antibody combining site (V) to react with only one antigenic determinant or the ability of a population of antibody molecules to react with only one antigen. Figure 17.9 IgG antibodies • • • • • • Monomer 80% of serum antibodies Fix complement In blood, lymph, intestine Cross placenta Enhance phagocytosis; neutralize toxins & viruses; protects fetus & newborn • Half-life = 23 days IgM antibodies • • • • • Pentamer 5-10% of serum antibodies Fix complement In blood, lymph, on B cells Agglutinates microbes; first Ab produced in response to infection • Involved in response to ABO blood group • Half-life = 5 days IgA antibodies • Dimer • 10-15% of serum antibodies • In secretions, mucus, salvia, tears, and breast milk • Mucosal protection • Half-life = 6 days IgD antibodies • • • • Monomer 0.2% of serum antibodies In blood, lymph, on B cells On the surface of B cells, initiate immune response • Half-life = 3 days IgE antibodies • Monomer • 0.002% of serum antibodies • On mast cells and basophils, in blood • Allergic reactions; lysis of parasitic worms • Half-life = 2 days Clonal Selection • Hematopoietic stem cell differentiate to produce naive B lymphocytes – Each lymphocyte bears a single type of receptor with a unique specificity - can recognizes only one type of antigen epitope • Naive cells mature into inactive B lymphocytes. 1. Most of them will never encounter a matching foreign antigen 2. Those that get in contact with a matching antigen are activated and produce many clones of themselves – plasma cells that produce antibodies 3. Some become memory cells Figure 17.5 - Overview Clonal deletion • Body doesn't make Ab against self, self-tolerance • Clonal deletion -the process of destroying B and T cells after they have expressed receptors for self-antigens and before they develop into fully immunocompetent lymphocytes Activation of B cells to produce antibodies • The first exposure to a microbe or an antigen, either by infection or by vaccination, leads to the activation of B lymphocytes plasma cells antibody producing cells 1. T-dependent antigens – Antigens which require participation of T cells for immune response 2. T independent antigens Figure 17.4 - Overview – Antigens that stimulate B cells without help of T cells • Repeating subunits – polysaccharides or lipopolysaccharides • Can bind multiple receptors of the B-cell Figure 17.6 Cell-Mediated Immunity • Red bone marrow stem cells give rise to T cells • mature in the thymus gland • migrate to lymphoid tissues • An antigen must be processed by an antigen-presenting cell and positioned on the surface of the APC (antigen presenting cell). • T cells recognize antigens in association with MHC on an APC Antigen-Presenting Cells APCs - B cells, Dendritic cells and Macrophages. Figure 17.13 Figure 17.12 Classes of T Cells • T cells are classified according to their functions and cell-surface glycoproteins called CDs. – Helper T Cells – Cytotoxic T Cells – Regulatory T Cells Helper T Cells • Helper T cells, or CD4 cells, are activated by MHC class II on APCs. • After binding an APC, CD4 cells secrete cytokines that activate other T cells and B cells. • TH1 cells activate cells involved in cellular immunity. • TH2 cells are associated with allergic reactions and parasitic infections. Helper T Cells Figure 17.13 Cytotoxic T Cells • Cytotoxic T cells (TC), or CD8 cells, are activated by endogenous antigens and MHC class I on a target cell and are transformed into a CTL (cytotoxic T lymphocyte). • CTLs lyse the target cell or induce apoptosis in the target cell. Cell-mediated Cytotoxicity Figure 17.10 - Overview Figure 17.14 Apoptosis • Programmed cell death is also called apoptosis • Cytotoxic T cells are able to directly induce apoptosis in cells – opening up pores in the target's membrane and releasing chemicals which bypass the normal apoptotic pathway. Regulatory T Cells • Regulatory T cells (TR) are vital for keeping the immune system in check, helping to avoid immune-mediated pathology and unrestricted expansion of effector T cell – Suppress other T cells when Ag no longer present – Involved in the checkpoints to prevent immune responses to self. T cells compete for same antigen T cells compete for cytokine signals Cytotoxic T cell Mature dendritic cell Regulator y T cell Regulator y T cells Proliferation Extracellular Killing by the Immune System • Natural killer (NK) cells lyse virus-infected and tumor cells. They are not immunologically specific. Antibody-Dependent Cell-Mediated Cytotoxicity • In ADCC, NK cells and macrophages lyse antibody-coated cells. Cytokines: Chemical Messengers of Immunity Cells • Cells of the immune system communicate with each other by means of chemicals called cytokines. – Interleukins (IL) are cytokines that serve as communicators between leukocytes. – Chemokines cause leukocytes to move to the site of infection. – Gamma Interferon activates macrophages Summary Immunological Memory • The amount of antibody in serum is called the antibody titer. • The response of the body to the first contact with an antigen is called the primary response. It is characterized by the appearance of IgM followed by IgG. • Subsequent contact with the same antigen results in a very high antibody titer and is called the secondary, anamnestic, or memory response. – Memory B cells – The antibodies are primarily IgG Antiserum • Serum containing antibodies is often called antiserum. • When serum is separated by gel electrophoresis, antibodies are found in the gamma fraction of the serum and are termed immune serum globulin, or gamma globulin Figure 17.17 Types of adaptive Immunity • Acquired active immunity; – resulting from infection – naturally this type of immunity may be long-lasting. • Acquired passive immunity – Antibodies transferred from a mother to a fetus (trans placental transfer) or to a newborn in colostrum results in naturally in the newborn; – can last up to a few months. • Artificially acquired active immunity – Immunity resulting from vaccination – can be long-lasting. • Artificially acquired passive immunity – refers to humoral antibodies acquired by injection; – can last for a few weeks. Learning objectives • • • • • • • • • • • • • • • • Differentiate between humoral and cellular immunity. Define antigen, epitope, and hapten. Explain the function of antibodies and describe their structural and chemical characteristics. Name one function for each of the five classes of antibodies. Compare and contrast T-dependent antigens and T-independent antigens. Differentiate between plasma cell and memory cell. Describe clonal selection. Describe four outcomes of an antigen-antibody reaction. Differentiate between helper T, cytotoxic T, and regulatory T cells. Differentiate between TH1 and TH2 cells. Define apoptosis. Define antigen-presenting cell. Describe the function of natural killer cells. Describe the role of antibodies and natural killer cells in antibody-dependent cell-mediated cytotoxicity. Identify at least one function of each of the following: cytokines, interleukins, interferons. Distinguish a primary from a secondary immune response. Contrast the four types of adaptive immunity.