File - Dr. Jerry Cronin
advertisement

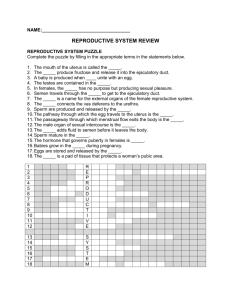
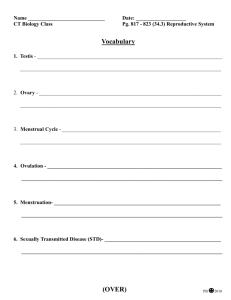
Female Reproductive Anatomy • The uterus is a pear shaped organ situated between the urinary bladder and the rectum – It serves as part of the pathway for sperm deposited in the vagina to reach the uterine tubes – It is also the site of implantation of a fertilized ovum, development of the fetus during pregnancy, and labor – During reproductive cycles when implantation does not occur, the uterus is the source of menstrual flow Female Reproductive Anatomy • Anatomical subdivisions of the uterus include: – A dome-shaped superior portion called the fundus – A central portion called the body, that tapers to a narrow isthmus – the inferior-most cervix opens into the vagina through the cervical canal Female Reproductive Anatomy • The interior of the body of the uterus is called the uterine cavity • The cervical canal has an internal os and an external os that opens into the uterine cavity and the vagina, respectively Female Reproductive Anatomy • The vagina is a fibromuscular canal lined with mucous membrane that extends from the exterior of the body to the uterine cervix. It is composed of both longitudinal and circular muscle, and has 3 basic functions: – Serve as a passageway for menstrual flow – Receive sperm – Form the lower birth canal Female Reproductive Anatomy • The vulva (female external genitalia) refers to the: – Mons pubis (created by adipose tissue) – Erectile tissue of the clitoris – Labia majora (outer limits of vulva) and labia minora (covers the vestibule) – Vestibule, the area between the labia minora – Vaginal orifice (opening) Female Reproductive Anatomy • Anterior to the vaginal orifice and posterior to the clitoris is the opening of the external urethral orifice – Mucus-secreting paraurethral glands flank the orifice (homologous to the prostate gland in males) • On either side of the vaginal orifice itself are the greater vestibular (Bartholin’s) glands which open by ducts into a groove between the hymen and labia minora. They produce a small quantity of lubricating mucous during sexual arousal Female Reproductive Anatomy • The perineum denotes the diamond-shaped area medial to the thighs and buttocks of females (and males) – the entire undersurface of the pelvis – It contains the external genitalia and anus Female Reproductive Anatomy Female Reproductive Anatomy • The breasts (mammary glands) are modified sudoriferous glands that produce milk: Each contains 15–20 lobes divided into lobules – Each lobule is composed of milksecreting glands called alveoli. The nipple has a pigmented area (areola) and openings for the lactiferous ducts Female Reproductive Anatomy Female Reproductive Physiology • During reproductive years, nonpregnant females normally exhibit cyclical changes in the ovaries and uterus – Each cycle takes about a month and involves both oogenesis (ovarian cycle) and preparation of the uterus to receive a fertilized ovum with hormones secreted by the hypothalamus, anterior pituitary, and ovaries controling the main events The Female Reproductive Cycle • The hormones secreted in the brain constitute the part of the cycle called the hypothalamic/pituitary cycle. Those hormones are GnRH, FSH, and LH –The reproductive organs in the female pelvis respond to the brain hormones by cycling at two “lower” levels • the ovarian cycle occurs in the ovaries where 1o , 2o and 3o follicles are formed • the uterine cycle refers to the monthly cycling of the endometrium when a woman is not pregnant The Ovarian Cycle • The formation of gametes in the ovaries is termed oogenesis. In contrast to spermatogenesis, which begins in males at puberty, oogenesis is more complex and begins in females before they are even born – During early fetal development, primordial germ cells migrate from the yolk sac to the ovaries where they differentiate into oogonia • Oogonia are diploid (2n) stem cells that divide mitotically to produce millions of germ cells The Ovarian Cycle • Even before birth, most oogonia degenerate, though a few develop into larger cells called 1o oocytes that enter prophase of meiosis I (during fetal development) but do not complete it until a fortunate few are called upon to do so during the reproductive years – During the interim (an arrested stage of development), each 1o oocyte is surrounded by follicular cells in a primordial follicle The Ovarian Cycle • At puberty, under the influence of LH and FSH (the brain gonadotropins), several primordial follicles will be stimulated each month, although only one will typically reach the maturity needed for ovulation – Maturing oocytes within maturing follicles undergo a series of developmental stages which ultimately brings one 2o oocyte within a 3o follicle to the point of ovulation • the ovulated 2o oocyte will have completed meiosis I, and so have the haploid number of chromosomes (1n)