Unit13
advertisement

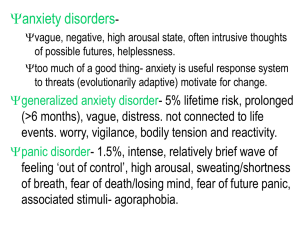
Mental Health Nursing II NURS 2310 Unit 13 Anxiety and Somatoform Disorders Key Terms Anxiety = Apprehension, tension, or uneasiness from anticipation of unknown/unrecognized danger; considered pathological when social and/or occupational functioning is affected Stress = Mental/emotional/physical strain experienced in response to stimuli from the external or internal environment Somatization = the expression of psychological needs in the form of physical symptoms; possibly related to repressed anxiety Panic = A sudden overwhelming feeling of terror or impending doom; usually accompanied by behavioral, cognitive, and physiological signs/symptoms considered to be outside the norm Hysteria = Characterized by recurrent multiple somatic complaints that are unexplained by organic pathology, and is thought to be associated with repressed anxiety Dissociation = The splitting off of clusters of mental contents from conscious awareness Amnesia = A pathologic loss of memory of an experience or specific period of time; emotional, dissociative, or organic in nature Phobia = An excessive or unreasonable fear cued by the presence or anticipation of a specific object or situation, exposure to which provokes an immediate anxiety response; the phobic stimulus is avoided or endured with marked distress Types of Anxiety and Anxiety-Related Disorders Panic Disorder Recurrent panic attacks that cause intense apprehension, fear, or terror Associated w/feelings of impending doom Accompanied by intense physical discomfort Panic attacks usually last only minutes, but symptoms of depression are common due to unpredictable nature of occurrence Average age at onset is late 20s Characterized by periods of remission and exacerbation Diagnostic Criteria for Panic Disorder include the presence of at least 4 of the following: – palpitations, pounding heart, or accelerated heart rate – sweating - parasthesias – trembling or shaking - chills or hot flashes – sensations of shortness of breath or smothering – feeling of choking – chest pain or discomfort – nausea or abdominal distress – feeling dizzy, unsteady, lightheaded, or faint – derealization or depersonalization – fear of losing control or going crazy – fear of dying Generalized Anxiety Disorder Chronic, unrealistic, and excessive worry that causes clinically significant distress or impairment in social/occupational functioning Numerous somatic complaints and symptoms of depression are common; exacerbations are stress-related Other symptoms include restlessness, fatigue, irritability, difficulty concentrating, muscle tension and sleep disturbances May begin in childhood/adolescence Diagnosed after 6 months of symptoms Phobias Includes agoraphobia, social phobia (or social anxiety disorder), and specific phobia Agoraphobia Fear of being in places/situations from which one can’t escape, or in which help might not be available if panic symptoms should occur Onset in the 20s or 30s; persists for many years Impairment can be severe and cause the individual to be confined to his/her home Social Phobia Excessive fear of situations in which a person might do something embarrassing or be evaluated negatively by others Extreme concerns about being exposed to possible scrutiny by others Fear of social or performance situations in which embarrassment may occur Onset of symptoms often begins in late childhood or early adolescence and runs a chronic, sometimes lifelong, course Impairment interferes with functioning Specific Phobia A marked, persistent, and excessive or unreasonable fear when in the presence of, or when anticipating an encounter with, a specific object or situation Frequently occur concurrently with other anxiety disorders Exposure to the phobic stimulus produces overwhelming symptoms of panic, including palpitations, sweating, dizziness, and difficulty breathing Individual recognizes that fear is excessive, but powerless to change it Obsessive-Compulsive Disorder Obsessions = unwanted, intrusive, persistent ideas, thoughts, impulses, or images that cause marked anxiety or distress Compulsions = unwanted, repetitive behavior patterns or mental acts such as praying or counting that are intended to reduce anxiety Obsessive-Compulsive Disorder = recurrent obsessions/compulsions severe enough to cause significant distress or impairment; individual recognizes behavior as excessive, but is compelled to continue due to the relief from discomfort that it provides; usually begins in adolescence or early adulthood Body Dysmorphic Disorder Exaggerated belief that the body is deformed or defective in some specific way Most common complaints involve imagined or slight flaws of the face or head Trichotillomania (Hair-Pulling Disorder) The recurrent pulling out of one’s hair from the scalp, eyebrows, and eyelashes Impulse preceded by increasing tension; the act produces sense of release or gratification Usually begins in childhood Trauma-Related Disorders Includes post-traumatic stress disorder (PTSD) and acute stress disorder Post-Traumatic Stress Disorder Develops following exposure to an extreme traumatic stressor involving a threat to the physical integrity of self or others Symptoms may begin within 3 months after the trauma or may be delayed; diagnosis occurs after symptoms that cause significant interference w/functioning have been present for at least 1 month PTSD (cont’d) Individual re-experiences the traumatic event via intrusive recollections/nightmares; may not recall every aspect of the trauma Involves either a sustained high level of anxiety/arousal or a general numbing of responsiveness; may lead to depression and/or substance abuse Acute Stress Disorder Symptomology is the same as for PTSD, but symptoms resolve within 1 month of the precipitating trauma Adjustment Disorder A maladaptive reaction to an identifiable stressor that results in the development of clinically significant emotional or behavioral symptoms that impair social/occupational functioning or are in excess of expected reaction to the stressor Occurs within 3 months after onset of stressor and persists for no longer than 6 months after stressor or its consequences have ended Manifested as depression, anxiety, actingout behaviors or a combination thereof Somatic Symptom Disorders Includes somatic symptom disorder, illness anxiety disorder, conversion disorder, and factitious disorder (previously known as Munchausen syndrome) May involve primary or secondary gains – In primary gain, the physical symptoms allow the individual to avoid some unpleasant activity or difficult situation about which he or she is anxious – Secondary gain involves the promotion of emotional support or attention the individual might not otherwise receive Somatic Symptom Disorder Characterized by multiple physical symptoms that have no medical explanation Associated with psychological distress and long-term seeking of assistance from health-care professionals Symptoms may be vague, dramatized, or exaggerated in their presentation Illness Anxiety Disorder Unrealistic or inaccurate interpretation of physical symptoms that results in excessive preoccupation about having a serious illness Illness Anxiety Disorder (cont’d) Fear becomes persistent and disabling in spite of reassurances that no organic pathology can be found History of doctor-shopping due to presumed misdiagnosis Conversion Disorder Emotional distress expressed through loss of (or change in) body function for which there is no apparent physical cause Symptoms may occur suddenly following a stressful experience Factitious Disorder The conscious, intentional feigning of physical and/or psychological symptoms on oneself or another person (i.e. by proxy) in order to receive emotional care and support May involve self-infliction of painful injuries, injection or insertion of contaminated substances, manipulation of medical assessment instruments, and/or improper use of medication Dissociative Disorders Includes dissociative amnesia, dissociative identity disorder (or multiple personality disorder), and depersonalizationderealization disorder Dissociative Amnesia Inability to recall important personal information; may be specific to a trauma or series of traumatic experiences Usually follows severe psychosocial stress, and recovery is often abrupt and complete Dissociative Identity Disorder Characterized by the existence of two or more unique personalities in a single individual Only one personality is evident at any given moment, and only one is dominant most of the time over the course of the disorder Transition from one personality to another may be sudden or gradual, and may be dramatic Symptomology causes clinically significant distress or functional impairment Depersonalization-Derealization Disorder Depersonalization = a disturbance in the perception of oneself Derealization = an alteration in the perception of the external environment Depersonalization-Derealization Disorder = characterized by a temporary change in the quality of self-awareness – Involves change in body image and feelings of unreality or detachment from the environment – Diagnosis made upon functional impairment Treatment Modalities Individual psychotherapy – Eye movement desensitization and reprocessing (EMDR) Cognitive and/or behavioral therapy – Systematic desensitization – Implosion therapy (flooding) Group/family therapy Psychopharmacology Medications used to Treat Anxiety Disorders Most commonly treated with anti-anxiety agents and sedative-hypnotics – Depress subcortical levels in the limbic system – CNS depression ranges from mild sedation to coma Classes of anti-anxiety agents include antihistamines, benzodiazepines, and miscellaneous agents – Buspirone (Buspar) does not depress the CNS 10-day to 2-week onset Does not build tolerance or dependence Sedative-hypnotics include barbiturates, benzodiazepines, and miscellaneous agents *Anti-anxiety agents: Antihistamines – Hydroxyzine (Atarax, Vistaril) Benzodiazepines – Alprazolam (Xanax) – Chlordiazepoxide (Librium) – Clonazepam (Klonopin) – Clorazepate (Tranxene) – Diazepam (Valium) – Lorazepam (Ativan) Miscellaneous agents – Buspirone (Buspar) Anti-Anxiety Agents (cont’d) Efficacy may vary – Alcohol, narcotics, barbiturates, antipsychotics, and antidepressants increases effects – Nicotine and caffeine decreases effects Common side effects include drowsiness, confusion, and lethargy Abrupt withdrawal can be life-threatening – Insomnia – Increased anxiety – Vomiting – Tremors, convulsions, and delirium *Sedative-hypnotics: Barbiturates – Secobarbital (Seconal) Benzodiazepines – Flurazepam (Dalmane) – Temazepam (Restoril) – Triazolam (Halcion) Miscellaneous Agents – Chloral Hydrate (Noctec) – Zaleplon (Sonata) – Zolpidem (Ambien) – Eczopiclone (Lunesta) Sedative-Hypnotic Agents (cont’d) Short-term use Chronic use may induce tolerance and physical/psychological dependence Additive effect on CNS depression with alcohol, antihistamines, antidepressants, or other CNS depressants Watch for decreased effectiveness of other medications metabolized by the liver Nursing Process Assessment – Gather information about client’s mood and level of anxiety, thoughts to harm self/others Diagnosis – Risk for self-directed violence R/T anxietyrelated depression – Imbalanced nutrition, less than body requirements R/T lack of interest in food – Disturbed sleep pattern R/T anxiety – Anxiety R/T panic disorder – Social isolation R/T agoraphobia Planning – Care plan – Concept map Implementation – Establish trust – Provide for safety – Perform risk assessment – Administer scheduled and PRN medications Evaluation – Mental health/psychiatric assessment tool – Review safety plan/contract – Assess for medication side effects