File
advertisement
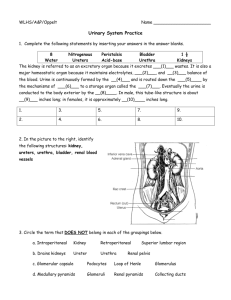
The Urinary System Physiology –II PHL 226 Prof. Dr/ Gamal Soliman Pharmacy College 1 The urinary system - Introduction The Urinary System is a group of organs that are responsible for excretion of excess fluid and other substances from the bloodstream in the form of urine. The urinary system consists of 6 principal organs: two kidneys, two ureters, the urinary bladder, and the urethra. Although the urinary system has a major role in excretion, other organs share in the excretory function: o The lungs excrete carbon dioxide and water. o The skin excrete wastes through the sweat glands. o The liver and intestines excrete bile pigments that result from the destruction of hemoglobin. Organs of the urinary system 1- The Kidneys: The kidneys are the primary organs of the urinary system as they filter the blood and excrete the wastes in the urine. The kidneys get their blood supply from the renal artery, which is a branch of the abdominal aorta. The kidneys receive 20–25% of the total arterial blood pumped by the heart each minute SO all the blood in the body passes through the kidneys several times a day. Each kidney contains around a million functional units called nephrons. 2- Ureters: They are 2 tubes of about 25 cm long. Function: They transport urine from the kidney to the urinary bladder. 3- Urinary bladder: The wall of the urinary bladder contain smooth muscle called the detrusor urinae muscle. Normally the urinary bladder can hold about 400-600mL of urine. The sense to urinate starts when the bladder is about 75% full. This stimulates the stretch receptors in the wall of the bladder to initiates a reflex called micturition (urination). The internal floor of the bladder includes a triangular area called the trigone. The trigone has 3 openings at each of its angles. o Two of the openings are from the ureters and form the base of the trigone. o The third opening, at the apex of the trigone, is the opening into the urethra. Function of UB It stores and expels urine. 4- Urethra: It is a tube that transports urine from the bladder to the outside of the body. The flow of urine through the urethra is controlled by 2 urethral sphincters. a- The internal urethral sphincter: It is smooth muscle (involuntary) . It surrounds the beginning of the urethra. b- The external urethral sphincter: It is skeletal muscle (voluntary). It surrounds the urethra at the pelvic floor. NOTES: The main difference between the urinary system of male and female is the “length of urethra.” The female urethra is short (3-4 cm long). The male urethra is much longer (about 20 cm long) Layers and cavities of the Kidney Layers of the Kidney Kidney has 2 layers: 1. The cortex: This is the layer immediately under the renal capsule. It contains the filtration structures (nephrons). 2. The medulla: The medulla is below the cortex. It contains 8-12 pyramid-shaped structures called renal pyramids. The renal pyramids are made up of hundreds of collecting ducts that transport urine from the cortex, where urine is produced, to the calyces. NOTES: The cortex and medulla make up the parenchyma of the kidney. The parenchyma are the functional parts of an organ in the body. This is in contrast to the stroma, which refers to the structural tissue of organs, namely, the connective tissues. Cavities of the kidney 1. Renal calyx There are 2 types of renal calyx: a- Minor calyx: o It is a short tube that receives urine from the collecting ducts. o There is only one minor calyx for each renal pyramid. b- Major calyx: o Several minor calyces merge to form larger spaces called major calyces. In the human body, there are 8-14 minor calyces and 2-3 major calyces. Function of renal calyces : They collect urine from the collecting ducts and empties the urine into the renal pelvis. 2. Renal Pelvis It is the superior end of the ureter which is expanded to form a funnel shape. The renal pelvis is formed by the junction of all major calyces. Function: It collect urine from the renal calyces and empties the urine into the urinary bladder through the ureters. Microscopic Anatomy – The nephron Individual nephrons cannot be seen by the naked eye. The nephron is the basic structural and functional unit of the kidney. In humans, a normal kidney contains 800,000 to 1.5 million nephrons that are connected in parallels. Classes of the nephron: a- Cortical nephrons: 85% of nephrons are located mostly in the cortex. They have short loops of Henle b. Juxtamedullary nephrons: 15% of nephrons are located close to cortex-medulla junction. They have long loops of Henle that dip into the medulla. Structure of the nephron : Each nephron is composed of 2 main structures: I- Renal corpuscle (Malpighian body). II- Renal tubule. I- Renal Corpuscle (Malpighian body): The renal corpuscle represents the basic filtration structure of the kidney. It consists of 2 structures: 1- The glomerulus 2- Bowman's capsule (The glomerular capsule). 1- The Glomerulus: The glomerulus is the site of filtrate formation. The glomerulus is a ball or knot عقدةof capillaries. The capillaries of the glomerulus are fed by an afferent arteriole and drained by an efferent arteriole. The endothelium of the glomerulus has fenestrations (pores) so these capillaries are very permeable and allow large quantities of fluid to pass from the blood into the interior of the Bowman's capsule (Bowman's space). The fluid inside Bowman's space is called the glomerular filtrate that is later processed into urine. Initial glomerular filtrate has biochemical constituents similar to that of the blood plasma (contains both nutrients and wastes). NOTES: The endothelium is the thin layer of cells that lines the interior surface of blood vessels. The cells that form the endothelium are called endothelial cells. 2- Bowman’s capsule This is an enlarged, cup-shaped closed end of the renal tubule that completely surrounds the glomerulus. Bowman's capsule has 2 layers: a. The visceral layer is in contact with the glomerulus, and is composed of specialized epithelial cells known as podocytes. b. The parietal layer is the outer layer. The space between the two layers is named Bowman's space, and this space contains the glomerular filtrate. II- Renal tubule: It is the site of reabsorption and secretion of solutes. Each renal tubule is made up of 4 segments: 1. Proximal convoluted tubule (PCT). 2. Loop of Henle. It consists of 2 straight parallel limbs: a- descending limb which joins the PCT. b- ascending limb which joins the DCT. 3. Distal convoluted tubule (DCT). 4. Collecting duct. The segments of the renal tubule differ in their function. The Blood Supply to the Nephron 1- Afferent arteriole : The afferent arteriole of each nephron branches to form the glomerulus. It supplies blood, under high pressure, to the glomerulus. 2- Efferent arteriole - A continuation of the glomerulus. It receives blood from the glomerulus and supplies blood to the peritubular capillaries (in cortical nephrons) or vasa recta (in juxtamedullary nephrons). A- Peritubular capillaries : They are the main capillaries of the cortical nephrons which arise from the efferent arteriole. B- The vasa recta : They are the main capillaries of the juxtamedullary nephrons which arise from the efferent arteriole. NOTES: The blood pressure inside the glomerulus is HIGH due to the difference in diameter of the afferent and the efferent arterioles. The blood pressure in the renal glomerulus is higher than in most parts of the body due to the difference in diameter of the afferent and the efferent arterioles. 1. Capillary endothelium (The endothelial cells of the glomerulus). 2. The basement membrane. 3. The epithelial cells of Bowman’s capsule (Podocytes) The glomerular Filtration Barrier (The filtration membrane) The filtration membrane is composed of 3 layers : 1. Capillary endothelium (The endothelial cells of the glomerulus): The endothelial cells are perforated by many large fenestrations (pores), which have a diameter of 50-100 nm. This layer is freely permeable to everything in the blood except blood cells and most proteins. 2. The basement membrane: The basement membrane is the main filtration barrier. It is a non-cellular structure that prevents any large molecules from being filtered. The anionic heparan sulphate proteoglycan in the basement membrane repels negatively charged proteins such as albumin. 3. The epithelial cells of Bowman’s capsule (Podocytes): It is a single layer of cells called podocytes, which rest on the basement membrane. The podocytes have processes known as foot processes, in addition to slit pores which control the movement of substances through the final layer of the filter. Function of the filtration membrane: 1. It allows passage of water and solutes from blood into the Bowman's space. 2. It prevents the filtration of most proteins and blood cells. NOTES: The anionic heparan sulphate proteoglycan within the glomerular basement membrane is the main barrier that prevents the free passage of proteins as albumin across the glomerular capillary walls. Almost any molecule smaller than 3 nm can pass freely through the filtration membrane into the Bowman's space. Urine formation The entire responsibility for urine formation lies with the nephron. Urine is formed in the nephrons in 3 processes: Glomerular filtration Tubular reabsorption Tubular secretion 1- Glomerular filtration It is the process of flow of water and solutes from the blood stream into the Bowman's capsule through the glomerular membrane. The increased blood pressure inside the glomerulus helps to force the following components of the blood into the Bowman's capsule : o Most of water. o Most/All of the glucose. o Most/All of the salts. o Most/All of the amino acids o Most/All of nitrogenous wastes. The fluid that cross the glomerular membrane is called the glomerular filtrate. The process of glomerular filtration is nonselective, passive process. The filtrate does not contain blood cells or plasma proteins because they are too large to pass through the pores of the capillary membrane. The Glomerular Filtration Rate (GFR): It is the volume of filtrate produced by both kidneys in one minute. o The normal GFR in adults is about 125 mL/min OR 180 L/day. o An average of 99% of the filtrate is reabsorbed, so that only 1-2 L of urine per day is excreted. o Measuring the glomerular filtration rate (GFR) is a diagnostic test of kidney function. o A decreased GFR may be a sign of renal failure. NOTES: If the diameter of the afferent arteriole is smaller than the diameter of the efferent arteriole, then: a. The blood pressure in the glomerulus will decrease. b. The pressure necessary for filtration will decrease. The glomerular filtrate contains both nutrients and wastes SO, not all of the filtered material is excreted. 2- Tubular reabsorption It is the process of returning of water and valuable solutes from the glomerular filtrate into blood through the capillaries around the tubules (peritubular capillaries and vasa recta). The PCT is the site at which most of the tubular reabsorption occurs. Reabsorption occurs by passive and active processes. The reabsorbed substances are: PCT It reabsorbs 65% of the filtered water. Of the 180 L/day of the filtrate entering the nephrons, approximately 120 L/day is reabsorbed by the PCT (65% of the filtrate) . It reabsorbs 65-80% of the filtered Na+ and Cl It reabsorbs all of the filtered glucose and amino acids (100%). It reabsorbs 85 to 90% of the filtered bicarbonate (HCO3- ). It reabsorbs more than 90% of the filtered calcium. It reabsorbs urea and uric acid. NOTE: There are two major proteins are responsible for fluid reabsorption in the PCT: a. Na+/K+-ATPase pumps: They are transmembrane proteins that are localized in the plasma membrane of the PCT. They are responsible for the reabsorption of Na+. Water and chloride then follow the transported sodium. b. Aquaporins: They are small transmembrane protein that functions as water channels in the cell membrane of the renal tubules. Movement of water through these channels does not require any source of energy. Loop of Henle a- descending limb: It reabsorbs 10% of the filtered water by osmosis. b- ascending limb: It reabsorbs 10 – 20% of the filtered Na+, K+ and Cl-. DCT : It reabsorbs water in response to the antidiuretic hormone (ADH) - released by the posterior pituitary gland. It reabsorbs Na+ ions in response to aldosterone hormone - released by the adrenal gland. It reabsorbs Ca2+ in response to parathyroid hormone (PTH) - released by the parathyroid gland. It reabsorbs 10 to 15% of the filtered bicarbonate (HCO3- ). Collecting duct: It reabsorbs water in response to the ADH. It reabsorbs NaCl in response to the aldosterone hormone. NOTES: DCT and the collecting duct are relatively impermeable to water. However their permeability to water increases in the presence of the ADH. The levels of ADH determine whether urine will be concentrated or dilute. Water reabsorption through the PCT is termed obligatory water reabsorption, whereas water reabsorption through the DCT is termed facultative water reabsorption. 3- Tubular secretion Tubular secretion is the opposite of reabsorption. The unfiltered, large molecular substances are secreted from the blood of peritubular capillaries or vasa recta into the glomerular filtrate. Secretion occurs by both passive diffusion and active transport processes Substances secreted include: PCT: It secretes wastes (urea, uric acid, creatinine), ions (H+ , NH4+), and some drugs (penicillin, morphine, salicylates). Loop of Henle a- ascending limb: It secrets urea. DCT: It secrets more K+ in response to aldosterone hormone. It secrets more phosphate in response to PTH. It secretes H+ when pH of the blood is low SO, tubular secretion is effective in controlling blood pH. It secretes ammonium ions and some drugs. NOTE: Much of the ion transport taking place in the DCT is regulated by the endocrine system. Urine is composed of filtered and secreted substances. After traveling the length of the DCT, only 3% of water remains, and the remaining salt content is negligible. Functions of the Urinary System 1- Excretory functions The urinary system excretes different waste products such as the nitrogenous compounds (ammonia, urea or Blood urea nitrogen, uric acid), creatinine and bilirubin in the urine. It eliminates foreign chemicals as drugs from the body. NOTES: The nitrogenous compounds (ammonia, urea, uric acid) are products of protein metabolism. How is urea formed in the human body? Ammonia is produced in the liver due to the degradation of amino acids. Ammonia (NH3) is a highly toxic substance. In the liver ammonia reacts with carbon dioxide to form urea and water, a process called ureogenesis. Urea is a less toxic compound than ammonia and urea. Urea is carried by the blood to the kidneys for excretion. The amount of urea in urine is related to quantity of dietary protein. The major site of uric acid production is the liver Uric acid is a product of the metabolic breakdown of purine nucleotides. Purines are obtained from both dietary sources and from the breakdown of body proteins. The kidneys excrete two-thirds of the uric acid produced daily; the remaining one-third is excreted in the stool. High blood concentrations of uric acid can lead to gout. Due to its insolubility, uric acid has a tendency to crystallize forming kidney stones. Creatinine is a normal constituent of blood. It is produced mainly as a result of the breakdown of creatine phosphate in muscle tissues. Bilirubin is the end products of hemoglobin breakdown. 2- Reabsorption of water, ions and vital nutrients. 3- Regulation of blood volume: The kidney conserve or eliminate water from the blood to regulates the volume of blood. 4- Regulation of blood pressure: The kidneys regulate blood pressure in 2 ways: Adjusting the volume of blood in the body. Via the action of the enzyme renin. The kidneys secrete renin which activate the angiotensin-aldosterone system. 5- Regulation of the ionic composition of the blood by regulating the number of Na+, K+, Cl- and other ions lost in the urine. 6- Regulation of calcium level of the blood : The kidneys reabsorb more than 90% of the filtered calcium in the PCT. Parathyroid hormone acts on the DCT to increase calcium reabsorption into the blood. 7- Regulation of the pH of the blood: by regulating the number of H+ and bicarbonate ions (HCO3-) lost in the urine. 8- Production of red blood cells: The kidneys stimulate the production of RBCs by releasing the hormone erythropoietin (EPO). EPO acts on the bone marrow to stimulate the process of erythropoiesis (production of red blood cells). Stimuli such as bleeding or moving to high altitudes (where oxygen level is low) trigger the release of EPO. 9- Activation of Vitamin D Vitamin D3 (cholicalciferol) that is absorbed by the small intestine and that is synthesized from cholesterol in the skin (Vitamin D3 synthesis requires ultraviolet from the sun) is activated in the kidneys into calcitriol which is the active form of vitamin D. The parathyroid hormone (PTH) increases the activity of α-hydroxylase enzyme in the DCT which activates cholicalciferol to calcitriol (the active form of vitamin D). Calcitriol acts on the cells of the intestine to promote the absorption of calcium. NOTES: Parathyroid hormone and vitamin D are the major hormones that influence calcium balance in the body. The human kidney secretes two hormones: 1- Erythropoietin (EPO) 2- Calcitriol, the active form of vitamin D. Deficiency disorders Insufficient calcitriol prevents normal deposition of calcium in bone. o In childhood, this produces the deformed bones characteristic of rickets. o In adults, it produces weakened bones causing osteomalacia. The most common causes of calcium deficiency are inadequate amounts of the vitamin in the diet or insufficient exposure to the sun. Antidiuretic hormone (ADH) -Vasopressin Synthesized in the hypothalamus and stored in vesicles at the posterior pituitary gland to be released into the bloodstream. The two main functions of ADH are: 1- To retain water in the body by reducing the loss of water in urine. ADH increases water reabsorption by stimulating insertion of "water channels" or aquaporins into the membranes of the DCT and the collecting ducts . It results in excretion of more concentrated urine. 2- To constrict blood vessels. Aldosterone hormone Aldosterone is a hormone produced by the cortex of the adrenal glands. It causes the DCT and collecting ducts to reabsorb sodium ions from the filtrate and secret potassium in the urine. Aldosterone is secreted in response to: o Decreased blood volume o Decreased interstitial fluid level o Decreased blood pressure. NOTE: If the level of aldosterone in the blood increases, then less sodium is excreted in the urine Juxtaglomerular apparatus (JGA) The JGA is a specialized structure formed by the DCT and the afferent arteriole of the same nephron. It is located near the glomerulus. The main function of the JGA is the secretion of renin in response to decreased renal blood pressure or blood flow. The juxtaglomerular apparatus is composed of: 1- Juxtaglomerular cells (Granular cells): surrounding the afferent arterioles. 2- The macula densa cells: lining the wall of the DCT. 1- Juxtaglomerular cells (Granular cells): Juxtaglomerular cells are specialized smooth muscle cells surrounding the afferent arterioles. They synthesize, store and secrete the enzyme RENIN. They act as mechanoreceptors. The function of the Juxtaglomerular cells is to monitor the changes in blood pressure in the arterioles. Juxtaglomerular cells secrete renin in response to 3 things: a. A decrease in the blood pressure in afferent arteriole (that could be related to a decrease in blood volume). b. Signals from the macula densa. c. Stimulation of Beta-1 receptors in the kidney (Sympathetic nervous system activity). 2- The macula densa cells The macula densa cells are specialized cells lining the wall of the DCT. They act as osmoreceptors. The function of the macula densa cells is to monitor NaCl concentration in the filtrate of the DCT. A decrease in blood pressure results in less NaCl present at the DCT. The macula densa responds to the drop in salt concentration through 2 mechanisms: a. Dilates the afferent arteriole of the glomerulus, which increases the pressure inside the glomerular and helps return glomerulus filtration rate (GFR) toward normal. b. Releases prostaglandins which stimulates the juxtaglomerular cells to release renin into the bloodstream. Renin-angiotensin system (RAS): Low levels of NaCl in the filtrate cause the macula densa cells to secret prostaglandins which stimulates the juxtaglomerular cells to release renin into the bloodstream. Renin starts a chain of linked biochemical reactions in blood by converting angiotensinogen (peptide secreted from the liver), into Angiotensin I. A second enzyme, Angiotensin Converting Enzyme (ACE), that found in capillary beds especially in the lungs and kidneys converts Angiotensin I into Angiotensin II, which is the most vasoactive peptide. Angiotensin II has the following effects: 1- It constricts blood vessels causing generalized vasoconstriction and, therefore, raises the blood pressure. 2- It stimulates the PCT in the kidney to reabsorb sodium ions. 3- It stimulates the adrenal cortex to release aldosterone, which stimulates the epithelial cells in the DCT and collecting ducts of the kidneys to promotes reabsorption of sodium ions and thus water (increase blood volume and further raise blood pressure). 4- It stimulates the posterior pituitary gland to release ADH which promotes water reabsorption, leading to raised blood volume and raised blood pressure. All of these actions lead to an increase in blood pressure. Urine and urinalysis Urine is a liquid produced by the kidneys. collected in the bladder and excreted through the urethra. The urinary system produces urine by a process of filtration, reabsorption, and tubular secretion. Urine is sterile until it reaches the urethra, where epithelial cells lining the urethra are colonized by some anaerobic Gram negative bacteria. Biochemical analysis of urine is called urinalysis and is commonly used to diagnose a wide range of diseases. Urination (micturition): When bladder fills with 200 ml of urine, stretch receptors transmit impulses to the CNS and produce a reflex contraction of the bladder. Pathway of urine: Collection duct minor calyx major calyx renal pelvis ureter urinary bladder urethra. Physical characteristics of normal urine Volume : 1-2 L / 24 h per normal adult. Colour: Yellow-amber when freshly voided, but varies with urine concentration, medications and diet. The normal colour of urine is due to urochrome (pigment produced from breakdown of bile) and urobilin (pigment produced from breakdown of Hb). Kidney stones may produce blood in urine. Odour: Mildly aromatic but becomes ammonia-like after a while due to bacterial action. pH: pH of normal urine ranges between 4.5 and 8 (average is 6.0). High-protein diets increase acidity. Vegetarian diet- increase alkalinity. Specific gravity (Density): It ranges between 1.001-1.030 g/cm3 (Sp Gr of water = 1g/liter). The higher the concentration of solutes, the higher the specific gravity. Normal urine output: o = 0.5 mL/kg body wt/hr o = 30 to 40 ml per hour for an adult o = 720 ml to 960 ml per day from 180 liters of water per day of filtered fluid (304.6 water bottles per day) Chemical composition of normal urine Human urine consists of: 1- Water: Urine is 95% water by volume. 2- Solutes (5%). The solutes includes: o Nitrogenous waste: as urea, uric acid and creatinine. o Inorganic ions: as sodium (Na+), potassium (K+), chloride (Cl-), calcium (Ca2+), ammonium (NH4+), sulfates (SO42-), and phosphates (e.g., PO43). o Trace amounts of enzymes, hormones and pigments.