Pathophysiology2014

Carcinogenesis
Patricia Jakel, RN,MN,OCN
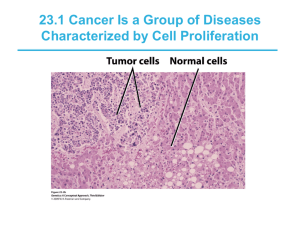
What Is Cancer?
What is cancer?
A series of cellular, genetic aberrations that cause abnormal cell proliferation.
Unchecked local growth (tumor formation) and invasion of surrounding tissue.
Ability to metastasize (e.g. spread in a contiguous fashion to form secondary sites).
Changing Approach and Outcomes
Cancer as disease change from acute to chronic
20th Century Model: “ Seek and
Destroy”
21st Century Model
Control”
: “Target and
Essential Aberrations of Malignancy
Proliferation
Evading Apoptosis-avoiding programmed cell death
Cellular Differentiation
Motility and Invasion
Recruitment of Blood Vessels and
Angiogenesis
Metastatic Spread
Cancer cells must compete successfully at each event to go forward.
Mechanism of Cancer
Apoptosis- is programmed cell death-that is, it is an active process controlled by cellular signaling. It may be triggered by the absence of a required growth factor:intercellular signals that indicate DNA damage or other injury to the cell; harmful external agents; or other intra- and extracellular events.
Mechanism of Cancer
Angiogenesis- or the formation of new blood vessels, critical step in tumor growth. Without tumors must obtain oxygen and nutrients by diffusion and therefore cannot grow larger.
The tumor remains dormant until it can stimulate blood vessel growth from nearby capillaries.
Malignant cells can release growth factors and enzymes that stimulate rapid formation of blood vessels. These chemical include VEGF- Targeted therapy.
Carcinogenesis
Refers to the process by which cancer arises.
Likely involves a series of multiple steps or cellular changes over time. This three-stage theory is the most widely used explanation of the process by which a normal cell is transformed into a cancer cell.
Pathology-cancer arsies due to cumulative alteration in a cell’s genes
1. Proto-oncogenes- the genetic portion of the DNA that regulates normal cell growth and repair: mutation may allow cell to proliferate beyond normal body needs.
Pathology
2.Tumor suppressor gene- the genetic portion of the
DNA that stops cell division; mutation may allow cells to proliferate beyond normal body needs.
3. Oncogenes- abnormal, mutated genes responsible for the transformation of a normal cell into a cancer cell. May arise from mutations in proto-oncogenes, tumor suppressor genes, or other genes.
3. Oncogenes continued-
Different types of oncogenes may act together to induce cancers.
1.p53 tumor suppressor gene-normally functions to stop cell proliferation, which allows DNA damage to be repaired.
When mutated, p53 restraint on cell proliferation is lost.
p53 mutations occur in about half of all human cancers: most common in colorectal, lung, and breast cancer.
3. Oncogene continued
2. Ras family of proto-oncogens-normally function to promote cellular growth
When mutated ras oncognes may allow cells to proliferate unrestrainted.
Ras oncogene are the most frequently detected oncogenes in human cancers; most common in pancreatic, colorectal, and thyroid cancers
Clinical Implications
Presence of certain oncogenes may have diagnostic and prognostic value.
Prevention of gene mutation is one focus of chemoprevention clinical trails.
Understanding of genetic changes may result in new targets for treatment
Genes and Cancer
Proto-Oncogenes- normal genes that participate in in normal tissue repair. Molecular “bucket brigade.”
Oncogenes- mutated proto-oncogenes. Excessively active
Secreted growth factor
Cell-surface growth-factor receptors
Membrane associated G protein
Tumor-Suppressor Genes- normal tell the cell to stop growing, role in cell cycle activity, helps with apoptosis
Relationship between genes and cancer
Cancer is a disease if genes gone awry. Genes that control the orderly replication of cells become damaged, allowing the cell to reproduce without restraint and eventually to spread into neighboring tissues and set up growths throughout the body.
Cancer Tends to Involve Multiple Mutations
Benign tumor cells grow only locally and cannot spread by invasion or metastasis
Malignant cells invade neighboring tissues, enter blood vessels, and metastasize to different sites
Time
Mutation inactivates suppressor gene
Cells proliferate
Mutations inactivate
DNA repair genes
Proto-oncogenes mutate to oncogenes
More mutations, more genetic instability, metastatic disease
Cancer and Genetics
All cancer is genetic, in that it is triggered by altered genes. However, just a small portion of cancer is inherited: a mutation carried in reproductive cells, passed on from one generation to the next, and present in cells throughout the body.
Cancer and Genetics
Most cancer is random mutations that develop in body cells division during one’s lifetimeeither as a mistake when cells are going through cell division or in response to injuries from environmental agents such as radiation or chemicals.
1. Initiation
A cancer causing agent damages the
DNA, this gene may then:
Undergo repair
Become permanently changed
(mutated)but not cause cancer unless exposed to threshold levels of cancer promotors.
Become mutated and produce a cancer cell line.
Promotion- a process by which carcinogens are subsequently introduced, resulting in one of the following changes
:
Reversible damage to the proliferation mechanism of the cell; the effects of the promoting factors may be inhibited:
Cancer-reversing agent.
Host Characteristics
Time and dose limits.
Promotion continued.
Irreversible damage to the proliferation mechanism, resulting in cancer cell transformation.
Progression
Invasion -cells continue to divide; increase in bulk, pressure, and secretion of enzymes result in local spread and invasion of surrounding structures.
Neovascularization-formation of new blood vessels.
Metastasis-the production of secondary tumors at distant sites.
Routes of metastasis
Sites
Clinical Implication
Metastasis is the major cause of death from cancer.
Most tumors have begun to metastasize at the time of detection.
Invasion and Metastasis
1
Cancer cells invade surrounding tissues and blood vessels
2
Cancer cells are transported by the circulatory system to distant sites
3
Cancer cells reinvade and grow at new location
Carcinoma in Situ
Normal Hyperplasia Mild dysplasia
Carcinoma in situ
(severe dysplasia)
Cancer
(invasive)
Neoplasm vs Tumor
Interchangeable terms
Refers to abnormal growth of tissue that serves no function and continues to grow unchecked.
Can be benign or malignant
Cancer- common term for all malignancies
Tumor Nomenclature
Hematologic Malignancies
Lymphomas
Malignancies of the lymphocyte
Subclassified as:
Hodgkin's
Non-Hodgkin's
Multiple myeloma-arises from the plasma cell (B lymphocyte) line.
Tumor Nomenclature
Hematologic Malignancies
Leukemias
Arises from hematopoietic cells
Classified according to cell type and maturity.
Lympho-denotes leukemia of lymphoid origin.
Myleo-denotes leukemia of myeloid origin
Some common carcinomas:
Lung
Breast (women)
Colon
Bladder
Prostate (men)
Different Kinds of Cancer
Leukemias:
Bloodstream
Lymphomas:
Lymph nodes
Some common sarcomas:
Fat
Bone
Muscle
Naming Cancers
Cancer Prefixes Point to Location
Prefix Meaning adenogland chondrocartilage erythrored blood cell hemangioblood vessels hepatolipolymphomelanoliver fat lymphocyte pigment cell myelomyoosteobone marrow muscle bone
Why Cancer Is Potentially Dangerous
Brain
Melanoma cells travel through bloodstream
Liver
Melanoma
(initial tumor)
100%
Tumor Grading
General Relationship Between
Tumor Grade and Prognosis
Patient
Survival
Rate
Low grade
High grade
1 2
Years
3 4 5
100%
Tumor Staging
Five-Year Survival Rates for
Patients with Melanoma (by stage)
50%
I II III
Stage at Time of Initial Diagnosis
What Causes Cancer?
Some viruses or bacteria
Some chemicals Radiation
Heredity
Diet
Hormones
U.K.:
Lung cancer
Population-Based Studies
Regions of Highest Incidence
CHINA:
Liver cancer
AUSTRALIA:
Skin cancer
JAPAN:
Stomach cancer
U.S.:
Colon cancer
CANADA:
Leukemia
BRAZIL:
Cervical cancer
100
50
Heredity? Behaviors? Other Factors?
Colon Cancer
(Number of new cases per 100,000 people)
100
70
Stomach Cancer
(Number of new cases per 100,000 people)
5
0
Japan Japanese families in U.S.
U.S.
7
0
Japan Japanese families in U.S.
U.S.
Tobacco Use and Cancer
Some Cancer-Causing Chemicals in Tobacco Smoke
Low-Strength Radiation
High
Dallas
Skin
Cancer
Incidence
Detroit
Low
Least
Pittsburgh
Annual Sunshine
(UV radiation)
Most
High
High-Strength Radiation
Leukemia
Incidence
Low
Least
X-ray Dose
(atomic radiation)
Most
Ultraviolet radiation-a complete carcinogen
Sources of UVR
Sunlight
Tanning salons
Industrial sources-welding arcs
Viruses-
Infect DNA, resulting in proto-oncogene changes and cell mutation.
Effects modified by:
Age
Immunocompetence
Viruses
Cancer-linked virus
Virus inserts and changes genes for cell growth
Examples of Human Cancer Viruses
Some Viruses Associated with Human Cancers
AIDS and Kaposi’s Sarcoma
Without disease
HIV infection
Depressed immune system
KSHV infection
Kaposi’s sarcoma
Bacteria and Stomach Cancer
Patient’s tissue sample
H. pylori
Heredity Can Affect Many Types of Cancer
Inherited Conditions That Increase Risk for Cancer
Mutations and Cancer
Genes Implicated in Cancer
What causes cancer???
Exposure to carcinogens-chemical, or viral, or physical or familial
Exposure to radiation-cellular DNA damage by physical release of energy.
Ionizing radiation
Damage to the cell by this source;
Is usually repaired and no mutation results.
May give rise to a malignancy when damage affects proto-oncogenes or tumor suppressor genes.
Depends on numerous factors.
Cancer Prevention
Carcinogenic radiation
Carcinogenic chemicals
Cancer viruses or bacteria
Avoid Tobacco
15x
Lung Cancer Risk Increases with
Cigarette Consumption
Lung
Cancer Risk
10x
5x
0 15 30
Non-smoker
Cigarettes Smoked per Day
Protect Yourself From Excessive Sunlight
Skin cancers most common with
UVR
Melanoma
Basal cell carcinoma
Squamous cell carcinoma
Avoid Cancer Viruses
High
HPV Infection Increases Risk for Cervical Cancer
Cervical
Cancer
Risk
Low
Noninfected women
Women infected with
HPV
Chemical Carcinogens
Chemical substances that alter DNA
Avoid Carcinogens at Work
Some Carcinogens in the Workplace
Examples of ionizing radiation
Most exposure is natural and unavoidable.
Diagnostic radiographs, radiation therapy, radioisotopes used in imaging.
Cosmic rays.
Radioactive ground minerals and gases-radon, radium, uranium.
Cancers linked to ionizing radiation.
Compromised Immune System
Immune surveillance against cancer
Surveillance occurs via recognition of tumorassociated antigens
Immune response may fail .
Age
Tumor burden
Shed substances
Outside factors
Microscopic Appearance of Cancer Cells
Staging of Cancer
TNM
T-extent or size of the tumor
N-absence or presence and extent of regional lymph node metastasis
M-absence or presence of distant metastases.