Tumor Suppressor Genes
advertisement

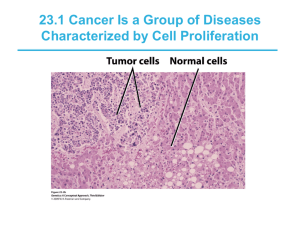
King Saud University College of Science Disclaimer Department of Biochemistry • The texts, tables and images contained in this course presentation are not my own, they can be found on: – References supplied – Atlases or – The web sites BCH 475 Biochemistry of Carcinogenesis Professor A. S. Alhomida Summer, 2008 Part 2 1 2 Oncogenesis 3 Oncogenesis Arises from • Spontaneous gene or chromosome mutations • Exposure to mutagens or radiation • Activity of genes introduced by tumor viruses • Some cancers are inherited (individuals may be predisposed) 4 Classes of Cancer Genes 5 Classes of Cancer Genes • Three classes of genes are mutated in cancer: (1) Proto-oncogenes whose products stimulate cell proliferation • Cab be mutated into oncogene that induce cell transformation (cancer cells) 6 Proto-oncogenes • Proto-oncgenes – Are genes that possess normal gene products and stimulate normal cell development • Oncogenes – Arise from mutant proto-oncogenes – Are more active than normal or active at inappropriate times and stimulate unregulated cell proliferation 7 Classes of Cancer Genes (2) Tumor suppressor genes whose products normally inhibit proliferation, negative regulatory protein 8 Classes of Cancer Genes (3) Mutator genes whose products ensure accurate replication and maintenance of the genome • Types of genes which may mutate to cause cancer (mutators) • DNA repair genes • Telomerase 9 10 Oncogenic Viruses (Viral Oncogenes) 11 Oncogenic Viruses • Oncogenic viruses or viral Carcinogenesis – Viruses which produce cancer • There is no single mechanism by which viruses cause tumors 12 Viral Oncogenes • Tumor viruses induce infected cells to proliferate and produce a tumor • There are two types, based on the viral genome: (1) RNA tumor viruses transform cells by introducing viral oncogenes • An oncogene is any gene that stimulates unregulated proliferation 13 Viral Oncogenes – RNA tumor viruses • Possess viral oncogenes • Derived from cellular proto-oncogenes capable of transforming cells to a cancerous state 14 Viral Oncogenes (2) DNA tumor viruses • Another class of tumor viruses; do not carry oncogenes, but induce cancer by activity of viral gene products on the cell (no transformation per se) 15 Cell Cycle and Cancer 16 Cell Cycle and Cancer • Cell differentiation occurs as cells proliferate to form tissues • Cell differentiation correlates with loss of ability to proliferate; highly specialized cells are terminally differentiated 17 Cell Cycle and Cancer • Terminally differentiated cells have a finite life span, and are replaced with new cells produced from stem cells • Stem cells are capable of selfrenewal; cells divide without undergoing terminal differentiation 18 Incidence of Cancer 19 Incidence of Cancer (1) Sporadic cancers – The more frequent type, do not appear to have an hereditary cause 20 Incidence of Cancer (2) Familial (hereditary) cancers – Run in families • Retinoblastoma – Is the most common eye tumor in children birth to 4 years – Early treatment (usually gamma radiation) is over 90% effective 21 Two-hit Mutation Model for Cancer 22 Two-hit Mutation Model • Cancers can be caused by viruses, but most result from mutations in cellular genes • Usually these mutations have accumulated over time, and research has identified the genes involved 23 Retroviruses and Oncogenes 24 Retroviruses and Oncogenes • Retrovirus – Single-stranded RNA virus that replicates via double-stranded DNA intermediate – RNA is converted to cDNA by reverse transcriptase – DNA integrates into host chromosome and is transcribed 25 Retroviruses Genes • Three types of genes occur in most retroviruses: – Gag (group antigen) • Codes the protein core – Pol (polymerase) • Codes reverse transcriptase and an enzyme for proviral integration – Env (envelope) • Codes envelope glycoproteins 26 Retroviruses and Oncogenes • Oncogenic retroviruses (v-onc) transform the cell and cause cancer (also called transducing viruses) • Different retroviruses carry different oncogenes responsible for different types of cancer – e.g. v-src in RSV 27 Retroviruses and Oncogenes • Most oncogenic retroviruses (but not RSV) are defective and do not possess a full set of virus life-cycle genes – Transform cells but do not produce progeny viruses 28 Retroviruses and Oncogenes • Defective retroviruses produce progeny with the help of a normal virus that co-infects cell and supplies missing gene products – Helper virus supplies missing gene products → viral expression 29 Transducing Retroviruses • Retroviruses that carry an oncogene (v-onc) are transducing retroviruses • Different types of cancer are caused by different v-onc genes (e.g., the sarcoma gene, v-src, of RSV) – RSV-infected cells rapidly transform, – Produce progeny RSV particles – Because RSV is unusual in having intact gag, pol, and env genes 30 Transducing Retroviruses – All other transducing retroviruses are defective, lacking one or more genes needed to replicate – If a helper virus supplies the missing gene product(s) progeny can be made 31 Structures of Four Defective Transducing Viruses 32 Structures of Four Defective Transducing Viruses 33 RNA Tumor Viruses • They are all retroviruses, and their oncogenes are altered forms of normal host genes – Examples include: • • • • Rous sarcoma virus Feline leukemia virus Mouse mammary tumor virus Human immunodeficiency virus (HIV-1, cause of AIDS) 34 35 RNA Tumor Viruses • Structurally, retroviruses have: – Two copies of the 7-10 kb ssRNA genome – A protein core (often icosahedral) – An envelope derived from host membrane and bearing viral glycoproteins used to enter a host cell 36 RNA Tumor Viruses • The retroviral life cycle was first characterized (1910) for a “filterable agent” from a chicken tumor, later named the Rous sarcoma virus (RSV) • RSV’s genome organization is known 37 RNA Tumor Viruses 38 Mechanism of RSV Action 39 Mechanism of RSV Action 40 Mechanism of RSV Action • Upon retroviral infection, the ssRNA genome is released from the virus particle, and reverse transcribed to dsDNA (proviral DNA) by reverse transcriptase carried in the virus particle 41 Mechanism of RSV Action – Proviral DNA integrates into host chromosome: • The 5’ (left) end of the viral genome has sequences R and U5, while the 3’ (right) end has sequences U3 and R • During proviral synthesis, genome ends are duplicated to produce long repeats (LTR) of U3-R-U5 • The LTRs contain transcription regulatory signals for viral genes 42 Mechanism of RSV Action • Proviral DNA is ligated to produce a circular dsDNA with two adjacent LTRs • Staggered nicks in proviral and host DNA are used for integration of the viral genome into the host chromosome • Single-stranded gaps are filled, producing short, direct repeats in host DNA flanking the provirus 43 Mechanism of RSV Action – Host RNA polymerase II transcribes the proviral DNA, and viral mRNAs are produced by alternative splicing – Three genes are characteristic of retroviruses: • The gag (group antigen) gene encodes a precursor protein that is cleaved to form the protein core (capsid) 44 Mechanism of RSV Action • The pol (polymerase) gene produces a precursor protein cleaved to make reverse transcriptase and an enzyme for proviral integration • The env (envelope) gene encodes the envelope glycoprotein, used to infect a host cell 45 Features of LTRs 46 Oncogenic Retroviruses Not Involved in the Cell Cycle 47 Oncogenic Retroviruses Not Involved in the Cell Cycle • Oncogenic retroviruses carry an oncogene that is not involved in the cell cycle – Different retroviruses carry different oncogenes – In RSV the oncogene is src 48 Oncogenic Retroviruses Not Involved in the Cell Cycle – Most retroviruses cannot replicate due to missing life-cycle genes (RSV is an exception) – Retroviruses without oncogenes (nononcogenic retroviruses) direct their own life cycle, and do not change the growth properties of infected cells 49 Nononcogenic Retroviruses 50 Life Cycle of Nononcogenic Retrovirus 51 Nononcogenic Retroviruses • They include HIV-1, a virus that causes AIDS, rather than cancer – The bullet-shaped capsid is surrounded by an envelope containing viral gp120 glycoproteins – The genome contains gag, pol and env genes, and several other genes used for gene regulation (e.g., tat regulates gag and pol expression) 52 Nononcogenic Retroviruses – Infection begins when the gp120 glycoprotein in the HIV-1 envelope binds: • Most commonly, the CD4 receptor of a helper T cell • A different receptor on a different type of cell (e.g., macrophage, glial cell in brain, regulatory cell of intestinal lining) 53 Mechanism of Nononcogenic Retroviruses 54 Mechanism of Nononcogenic Retroviruses – The virus particle enters the cell, the protein capsid is lost and the viral life cycle begins – Normal viral replication causes death of cells infected with HIV-1, depleting the helper T cells needed to mount an immune response – Unable to combat infection, AIDS patients frequently die of infections and cancers 55 Cellular Proto-oncogenes 56 Cellular Proto-oncogenes • Mid-1970s: J. Michael Bishop & Harold Varmus (Nobel Prize 1989) • Demonstrated normal animal cells contain non-cancer causing genes closely related to viral oncogenes 57 Cellular Proto-oncogenes • Early-1980s: R. A. Weinberg & M. Wigler demonstrated a variety of human tumor cells contain oncogenes, which transform normal cells growing in culture to cancer cells 58 Cellular Proto-oncogenes • Most human and animal oncogenes are mutated forms of normal cellular genes (proto-oncogene = normal state) 59 Cellular Proto-oncogenes • v-onc – Viral oncogene, carried by a virus • c-onc – Cellular oncogene, resides in host chromosome 60 Chicken c-src Proto-oncogene and v-src Oncogene 61 Genomic Changes that Cause Proto-oncogene Activation • Genomic changes (amplification, insertion & translocation) that cause proto-oncogene activation: – Amplification • c-myc, c-abl, c-myb, c-erbB, c-K-ras, mdm-2 • Presence of known oncogenes in amplified region – Amplification of same oncogenes in many cancers 62 Genomic Changes that Cause Proto-oncogene Activation • Insertion – Insertion of retrovirus LTR overexpresses c-myc • Insertion of ALV activates c-myc gene • Translocation – Reciprocal translocation by illegitimate recombination • Immunoglobulin or TCR gene and c-myc oncogene 63 Genomic Changes that Cause Proto-oncogene Activation • Increased c-myc expression after translocation • c-myc coding sequences are unaltered in all cases 64 Genomic Changes that Cause Proto-oncogene Activation 65 Genomic Changes that Cause Proto-oncogene Activation 66 Genomic Changes that Cause Proto-oncogene Activation 67 Genomic Changes that Cause Proto-oncogene Activation • Evidence of oncogenic potential of cmyc gene: – Transgenic mice carrying c-myc that: • Linked to B lymphocyte enhancer → lymphoma • Under mouse mammary tumor virus LTR → various cancers 68 Genomic Changes that Cause Proto-oncogene Activation • Translocation can generate hybrid oncogenes and human cancers – CML & Philadelphia chromosome • c-abl gene on chromosome 9 and bcr gene on chromosome 22 • Why is the hybrid bcr-abl protein oncogenic? – Activation of ras pathway for transformation 69 70 Mechanism of Retroviruses Oncogenesis 71 Mechanism of Retroviruses Oncogenesis • Retrovirus integrates into host chromosome near a cellular protooncogene by random recombination • Deletion fuses retrovirus transcription signal sequences with proto-oncogene sequences 72 Mechanism of Retroviruses Oncogenesis • In the process, parts of the viral DNA sequences typically are deleted (this is how the defective oncogene is created) • Viral “progeny” carry the cellular gene, but now under the influence of viral promoters 73 Mechanism of Retroviruses Oncogenesis • Most transducing viral oncogenes are defective and cannot replicate independently 74 Mechanism of Retroviruses Oncogenesis • If mRNA is packaged into a virus particle along with a normal virus genome (co-infection), reverse transcriptase produces a new defective oncogene by switching templates during cDNA synthesis 75 Mechanism of Retroviruses Oncogenesis • Template switching + lack of proofreading during DNA replication result in rapid evolution of oncogenic retroviruses 76 Formation of Transducing Retrovirus Oncogene 77 DNA Tumor Viruses 78 DNA Tumor Viruses • Do not carry oncogenes • Transform cells to the cancerous state through actions of genes in the viral genome 79 DNA Tumor Viruses • Examples include viruses in the following groups: – Papovaviruses (warts and human cervical cancer) – Hepatitis B – Herpes – Adenoviruses – Pox viruses 80 DNA Tumor Viruses • DNA viruses induce production of cellular DNA replication enzymes, which are used in viral replication • Rarely, viral DNA integrates into the host genome instead, and may produce protein(s) that stimulate the cell to proliferate 81 DNA Tumor Viruses • An example: – The papovavirus group includes many different papillomaviruses, some of which cause: • Human warts • Human cervical cancer (HPV-16, HPV-18), due to action of the E6 and E7 genes, which influence cell growth and division 82 Proto-oncogenes 83 Oncogenes • Oncogene is mutated form of normal genes called proto-oncogene – Control of cell proliferation and differentiation 84 Oncogenes • Oncogenic virus – Oncogenic DNA virus – Oncogenic RNA virus • Viruses are named because of reverse transcriptase • Retrovial oncogene, src 85 Proto-oncogen Activation • Normal cell genes from which oncogene originated, encoding proteins that function in: – Signal transduction pathway – Controlling normal cell proliferation 86 Proto-oncogen Activation 87 Functions of Oncogene Products • Uncotrolled proliferation of cancer cell • Defective differentiation • Failure to programmed cell death 88 ras Proto-oncogenes • Involved in signal transduction pathway as are many protooncogene products • ras family genes mutated in 40% of all cancers 89 ras Proto-oncogenes • Involved in signal transduction pathway from growth factor receptor to nucleus – G protein • Mutant form lacks GTPase activity and remains active 90 Proto-oncogene and Oncogene Protein Products • ~100 different oncogenes have been identified • To understand the cancer – Understand the function of protein products coded by the proto-oncogenes 91 Protein Products of Proto-oncogenes • Proto-oncogenes fall into classes with characteristic protein products, all of which stimulate cell growth • Examples: 92 Examples of Protein Products of Proto-oncogenes • An example of growth factors is the viral oncogene v-sis, which encodes platelet-derived growth factor (PDGF) – Deriving from mammalian blood platelets, PDGF causes fibroblasts to grow as part of wound-healing – Introduction of a cloned PDGF gene into cells that normally do not express it (e.g., fibroblasts) transformed the cells 93 Examples of Protein Products of Proto-oncogenes – Inappropriately expressed growth factors, therefore, can cause cancer • An example of protein kinases is the src gene product, which encodes pp60src, a nonreceptor protein kinase – Both cellular and viral versions of the pp60src protein phosphorylate tyrosine (rather than serine or threonine 94 Examples of Protein Products of Proto-oncogenes – Protein kinases are known to be involved in many aspects of cell signaling and growth regulation 95 Proto-oncogene and Oncogene Protein Products • All known proto-oncogenes are involved in positive control of cell growth and division 96 Proto-oncogene and Oncogene Protein Products • Two classes: – Growth factors • Regulatory genes involved in the control of cell multiplication – Protein kinases • Add phosphate groups to target proteins, important in signal transduction pathways 97 Mechanism of Conversion of Protooncogenes to Oncogenes 98 Mechanism of Conversion of Proto-oncogenes to Oncogenes • Conversion of proto-oncogenes to oncogenes relaxes cell control, allowing unregulated proliferation Examples: – Point mutations in the coding or controlling sequences can either change the gene product or alter its expression 99 Mechanism of Conversion of Proto-oncogenes to Oncogenes • The ras genes are an example: – A point mutation produces a mutant protein that can cause cancer in many different types of cells – G proteins lose regulation, and constitutive growth signals are transmitted to the cell 100 Mechanism of Conversion of Proto-oncogenes to Oncogenes – Deletions of coding or controlling sequences can change the amount of activity of growth stimulatory proteins, allowing proliferation. The myc gene is an example: • The myc gene product is a transcription factor that activates genes involved in cell division 101 Mechanism of Conversion of Proto-oncogenes to Oncogenes • Deletions can remove upstream sequences, allowing expression from an alternative promoter and changing the amount or activity of the protein product – Gene amplification, caused by random overreplication of regions of genomic DNA, has been found in tumor cells – Multiple copies of ras in mouse adrenocortical tumors are an example 102 Mechanism of Conversion of Proto-oncogenes to Oncogenes • Point mutations that result in constitutively active protein products • Localized gene amplification of a proto-oncogene leading to overexpression 103 Mechanism of Conversion of Proto-oncogenes to Oncogenes • Chromosomal translocation that brings a growth-regulatory gene under control of a different promoter that causes inappropriate expression • Note: These are generally gain-offunction mutations 104 Gain-of-function Mutations Convert Protooncogenes into Oncogenes 105 Gain-of-function Mutations • Oncogenes were first identified in cancer-causing retroviruses – The Rous sarcoma virus (RSV) contains a gene (src) that is required for cancerinduction but is not required for viral function • Normal cells contain a related gene that codes for a protein-tyrosine kinase 106 Gain-of-function Mutations • The normal gene (c-src) is the protooncogene, while the viral gene (v-src) is an oncogene that codes for a constitutively active mutant proteintyrosine kinase • Many DNA viruses also contain oncogenes but these have integral functions in viral replication 107 Slow-acting Carcinogenic Retroviruses can Activate Cellular Proto-oncogenes 108 Retroviruses Activate Cellular proto-oncogenes 109 Tumor Suppressor Genes 110 Tumor Suppressor Genes • Harris (1960s) showed that fusion of cancer cells and normal cells did not always result in a tumor, indicating the existence of tumor suppressor genes 111 Tumor Suppressor Genes • In certain cancers, both homologous chromosomes show deletion of specific regions, the sites of tumor suppressor genes that inhibit cell growth and division 112 Tumor Suppressor Genes • Human examples include: – Breast cancer – Colon cancer – Lung cancer • Action of tumor suppressors is the opposite of proto-oncogenes 113 Tumor Suppressor Genes • Both tumor suppressor genes must be lost for unregulated growth to occur (they are recessive), while only one mutation is needed to change a proto-oncogene to an oncogene (it is dominant) 114 Tumor Suppressor Genes • The gene’s normal function is to regulate cell division • Both alleles need to be mutated or removed in order to lose the gene activity • The first mutation may be inherited or somatic 115 Tumor Suppressor Genes • The second mutation will often be a gross event leading to loss of heterozygosity in the surrounding area • Block abnormal growth and malignant transformation 116 Tumor Suppressor Genes • Proto-oncogene; dominant in action • Tumor-suppressor gene; recessive in action – Examples: • Rb, p53, INK4, APC, DCC 117 Tumor Suppressor Genes • Functions of tumor suppressor gene products – Tumor development by eliminating negative regulatory proteins • Examples: – WT1, Rb and INK4, p53 gene product, APC and DCC 118 Five Proteins are Encoded by Tumor-Suppressor Genes 1. Intracellular proteins that regulate or inhibit progression through a specific stage of the cell cycle 2. Receptors for secreted hormones that inhibit cell proliferation 3. Checkpoint-control proteins that arrest the cell cycle 119 Five Proteins are Encoded by Tumor-Suppressor Genes 4. Proteins that promote apoptosis 5. Enzymes that participate in DNA repair Note: These are usually loss-offunction mutations 120 Loss-of-function Mutations in Tumor-suppressor Genes • The first tumor-suppressor gene was identified in patients with inherited retinoblastoma 121 Loss-of-function Mutations in Tumor-suppressor Genes 122 Loss-of-function Mutations in Tumor-suppressor Genes 123 Loss of Heterozygosity of TumorSuppressor Genes Occurs by Chromosome Mis-segregation or Mitotic Recombination 124 Loss of Heterozygosity of TumorSuppressor Genes Occurs by Chromosome Mis-segregation or Mitotic Recombination 125 Comparison of the Effects of Tumor Suppressor gene and Proto-oncogene Mutations 126 127 Protooncogenes and tumorsuppressor genes: the seven types of proteins that participate in controlling cell growth 128 p53 Tumor Suppressor Gene • Mutated (inactivated) in more than 50% of all cancers • p53 regulates (activates or represses) transcription of more than 50 different genes 129 Mutations in p53 Abolish G1 checkpoint Control • Some human carcinogens cause inactivating mutations in the p53 gene and • p53 activity is also inhibited by certain proteins encoded by DNA tumor viruses 130 Mutations in p53 Abolish G1 checkpoint Control 131 p53 Tumor Suppressor Gene • Mutations in the p53 gene occur in more than 50% of human cancers • Because p53 is a tetramer, a point mutation in a single allele can inhibit all p53 activity 132 p53 Tumor Suppressor Gene • MDM2, a protein that normally inhibits the ability of p53 to halt the cell cycle, is overexpressed in certain cancers • One human papillomavirus protein, E6, binds to and inhibits p53 133 p53 Tumor Suppressor Gene • The large T protein from the DNA monkey papovavirus binds to both p53 and Rb, inhibiting their function. • Carcinogens such as benzo(a)pyrene and aflotoxin induce inactivating mutations in p53 134 p53 Tumor Suppressor Gene • p53 regulated by Mdm2 (prevents the phosphorylations and acetylations that activate inactive p53) • Activated p53 levels rise rapidly if DNA is damaged or repair intermediates accumulate 135 p53 Tumor Suppressor Genes • Mutations in p53 are implicated in ~50% of human cancers, including cancers of the: – breast, brain, liver, lung, colorectal, bladder, and blood • Development of tumors requires mutations on two p53 alleles 136 p53 Tumor Suppressor Genes • Codes a 393 amino acid protein involved in transcription, cell cycle control, DNA repair, and apoptosis (programmed cell death) • p53 binds to several genes, including WAF1, and interacts with at least 17 cellular and viral proteins 137 p53 Tumor Suppressor Genes • Transgenic mice with deletions of both p53 alleles are viable, but 100% develop cancer by ten months of age • Effects of DNA damage and normal (non-mutant) p53 lead to cell growth arrest 138 p53 Function • Suppresses progression through the cell cycle in response to DNA damage • Initiates apoptosis if the damage to the cell is severe acts as a tumor suppressor • It is a transcription factor and once activate 139 p53 Function • It represses transcription of one set of genes (several of which are involved in stimulating cell growth) while stimulating expression of other genes involved in cell cycle control 140 p53 Function • Activated p53 acts as transcription factor to turn on genes that – Arrest the cell cycle so DNA can be repaired • Initiates synthesis of p21, which inhibits CDK4/cyuclinD1 complex, blocking entry into S phase • Genes expressed which retard rate of DNA replication • Other products block G2/M progression 141 p53 Function – Initiate apoptosis if DNA cannot be readily repaired • Turns on Bax gene, represses Bcl2 gene • Bax homodimers activate process of cell destruction • Cancer cells lacking p53 do not initiate pathway even if DNA/cellular damage is great 142 pRB Function • Tumor suppressor protein that controls the G1/S checkpoint • Found in nucleus and activity regulated by level of phosphorylation (by CDK4/cyclinD1 complex) 143 pRB Function • Nonphosphorylated version binds to TFs such as E2F, inactivating them • Free E2F and the other regulators turn on >30 genes required for transition to S phase 144 Role of pRB in Regulating Cell Division 145 Mechanism of Tumor Suppressor Genes 146 Mechanism of Tumor Suppressor Genes • Oncogenic virus enters the cell • DNA of virus enters cells chromosome – If retrovirus, first, the RNA is converted to DNA (provirus) – The provirus DNA enters the cell 147 Mechanism of Tumor Suppressor Genes • Virus has cancer causing gene = oncogene transformation: – Cell becomes cancer cell • In 1976 (Varmus and Bishop from UCSF received Nobel Prize 1989) • Oncogenes found in normal cells – (Same nucleotide sequence or genetic recipe) called protooncogene 148 Mechanism of Tumor Suppressor Genes • Most oncogenes are dominant genes • Whole lists of oncogenes now discovered for animal and a few for humans • We all have protooncogenes: – Human’s total genome is 100,000 genes probably < 100 are protooncogenes 149 Mechanism of Tumor Suppressor Genes – 40 discovered so far (50 Talaro) – They have normal functions that are important • Now we know that all cancers are the result of an oncogene 150 RB1 Tumor Suppressor Gene • Retinoblastoma 1 gene • Involved in breast, bone, lung, bladder and retinal cancers (among others) 151 RB1 Tumor Suppressor Gene • Inheriting one mutated (inactivated) copy of gene increases chances of retinoblastoma formation from 1/14,000-20,000 to 85% (plus increases other cancer rates) – Loss of second copy in a cell eliminates function – Normal cells unlikely to lose both good copies 152 DNA Repair Genes (Mutator Genes) 153 DNA Repair Genes (Mutator Genes) • Third category of cancer-causing genes – Excision, mismatch repair • Cancer effects are indirect • Defective DNA repair = increase rate of failure to repair mutations – Mutations accumulate in the genome 154 DNA Repair Genes (Mutator Genes) • Significance – Have an increased chance of mutation in a proto-oncogene and/or tumor suppressing gene 155 Mutator Genes 156 Mutator Genes • Mutator gene increases spontaneous mutation rate of other genes • Mutator gene products are involved in DNA replication and repair; mutations make the cell error prone • HNPCC-OMIM 120435, human nonpolyposis colon cancer 157 Mutator Genes • Mutation at any one of two genes (hMSH2, hMLH1, hPMS1, hPMS2) leads to predisposition • Tumor formation requires mutation at the second allele • All four genes have homologs in yeast • DNA blood tests are available for all 158 four genes Defects in DNA-repair Systems Perpetuate Mutations and are Associated with Certain Cancers 159 Virus-encoded Activators of Growth-factor Receptors Act as Oncoproteins 160 Activating Mutations or Overexpression of Growth-factor Receptors can Transform Cells 161 Constitutively Active SignalTransduction Proteins are Encoded by Many Oncogenes 162 Constitutively Active SignalTransduction Proteins are Encoded by Many Oncogenes 163 Chromosomal Abnormalities are Common in Human Tumors • In Burkitt’s lymphoma c-myc is translocated to chromosome 14 near an antibody-gene enhancer 164 Chromosomal Abnormalities are Common in Human Tumors • A translocation between chromosomes 9 and 22 causes the formation of the chimeric bcr-abl oncogene found in virtually all patients with chronic myelogenous leukemia 165 Chromosomal Abnormalities are Common in Human Tumors 166 Passage from G1 to S Phase is Controlled by Proto-oncogenes and Tumor-suppressor Genes 167 Passage from G1 to S Phase is Controlled by Proto-oncogenes and Tumor-suppressor Genes 168 Loss of TGF Signaling Contributes to Abnormal Cell Proliferation and malignancy 169 Finding Tumor Suppressor Genes • Recessive genes, like those for tumor suppression, are more difficult to detect than dominant genes • Positional cloning, the search for DNA variations between normal and tumor cells, was finally successful in isolating several tumor suppressor genes 170 Retinoblastoma 171 Retinoblastoma • Retinoblastoma has two forms: – Sporadic retinoblastoma (60%) develops in children with no family history of retinoblastoma, and occurs in one eye (unilateral tumor) 172 Retinoblastoma – Hereditary retinoblastoma (40%) patients typically develop multiple tumors involving both eyes (bilateral tumors) • Onset is usually earlier in the hereditary form • Siblings and offspring often develop the same type of tumor • Pedigrees of affected families are consistent with a single gene responsible for retinoblastoma 173 Knudson’s Two-hit Mutation Model for Retinoblastoma 174 Knudson’s Model for Retinoblastoma • Two mutations are required for the development of retinoblastoma • Sporadic retinoblastoma – Child starts with two wild type alleles (RB+/RB+) – Both alleles must mutate to produce the disease (RB/RB) 175 Knudson’s Model for Retinoblastoma – Probability of both mutations occurring in the same cell is low; only one tumor forms (e.g., one eye) 176 Knudson’s Model for Retinoblastoma • Hereditary retinoblastoma – Child starts with heterozygous alleles (RB/RB+) – Only one mutation is required to produce disease (RB/RB) – Mutations resulting in loss of heterozygosity (LOH) are more probable in rapidly dividing cells, and multiple tumors occur (e.g., both eyes) 177 178 Knudson’s Model for Retinoblastoma • Retinoblastoma alleles are recessive; only homozygotes (RB/RB) develop tumors • Retinoblastoma appears as dominant in pedigree analysis: – RB/RB+ individuals are predisposed and have a significant incidence of the disease 179 Knudson’s Model for Retinoblastoma – Homozygous dominant individuals (RB+/RB+) require two mutations in the same cell to develop the cancer • Retinoblastoma was mapped to the long arm of chromosome 13 (13q14.1-q14.2) 180 Knudson’s Model for Retinoblastoma • Mutations occur in a gene that encodes a growth inhibitory factors (tumor suppressor gene) • Retinoblastoma is rare among cancers; most cancers result from a series of mutations in many different genes 181 Retinoblastoma 182 Retinoblastoma 183 The Retinoblastoma Tumor Suppressor Gene • The human RB tumor suppressor gene has been mapped (13q14.1q14.2) and sequenced – Its 180 kb of DNA encodes a 4.7 kb mRNA that produces a 928-amino-acid nuclear phosphoprotein, pRB – pRB is expressed in every tissue type examined, regulating cell cycle and all major cellular processes 184 The Retinoblastoma Tumor Suppressor Gene – Tumor cells have point mutations or deletions in the gene, leading to loss of pRB function 185 The Retinoblastoma Tumor Suppressor Gene – Karyotype analysis detects about 5% of RB mutants, and the remainder are difficult to detect even with molecular techniques • Mitotic recombination • Chromosomal nondisjunction • Gene conversion 186 The Retinoblastoma Tumor Suppressor Gene • The cell cycle transition from G1 to S is regulated by pRB, committing the cell to the rest of the cycle – In a normal G1 cell, pRB binds two transcription factors, E2F and DP1 – As long as pRB stays bound to the factors, the cell remains in G1 or enters G0 187 The Retinoblastoma Tumor Suppressor Gene – At the signal to progress through the cell cycle, cyclin/cyclin-dependent kinase (Cdk) phosphorylates pRB so that it is unable to bind E2F – Free E2F now binds and activates transcription of genes required for entry into S phase – After the cell completes mitosis, pRB is dephosphorylated 188 The Retinoblastoma Tumor Suppressor Gene • In a cell with two mutant RB alleles: – If pRB is present, it is unable to bind E2F/DP1 – Target genes are activated, and the cell enters S phase 189 The Retinoblastoma Tumor Suppressor Gene • Several viruses (e.g., adenovirus, SV40) make proteins that complex with pRB, blocking its ability to bind E2F, and so allowing the S phase genes to be activated 190 The Retinoblastoma Tumor Suppressor Gene • pRB bind other cellular proteins, including those involved with all three RNA polymerases: – A component of the RNA polymerase II basal transcription machinery – Factors for rRNA synthesis by RNA polymerase I – Factors for tRNA synthesis by RNA polymerase III 191 The Retinoblastoma Tumor Suppressor Gene • Retinoblastoma indicates that pRB may also play a role in regulating development, perhaps by causing cells to become terminally differentiated 192 Retinoblastoma Tumor Suppressor Genes • Mapped to gene chromosome 13 and sequenced. • 180 kb; codes a 4.7 kb mRNA that produces a 928 amino acid nuclear phosphoprotein, pRB • pRB is expressed in every tissue that has been examined and regulates the cell cycle 193 Retinoblastoma Tumor Suppressor Genes • Retioblastoma tumor cells possess point mutations or deletions, which render pRB defective • In hereditary retinoblastoma, second RB mutation often is identical to the inherited one (a possible example of gene conversion) 194 Effects of DNA Damage and Normal p53 195 Breast Cancer Tumor Suppressor Genes • Breast cancer affects 1 in 10 women and represents 31% of cancers in women (~185,000 women diagnosed each year) 196 Breast Cancer Tumor Suppressor Genes • ~ 5% of breast cancers are hereditary; age of onset for hereditary breast cancer is earlier than other forms (mutations at two alleles) • Many genes involved; BRCA1 and BRCA2 are thought to be tumor suppressor genes 197 Breast Cancer Tumor Suppressor Genes • BRCA1 is important for homologous recombination, cellular repair of DNA damage, and transcription of mRNA • Mutations in BRCA1 also are involved in ovarian cancer • BRCA2 plays a role in timing of mitosis in the cell cycle 198 Multi-step Nature of Cancer • Cancer is a stepwise process, typically requiring accumulation of mutations in a number of genes • ~6-7 independent mutations typically occur over several decades: 199 Multi-step Nature of Cancer • Cancer is a stepwise process, typically requiring accumulation of mutations in a number of genes • ~ 6-7 independent mutations typically occur over several decades: – Conversion of proto-oncogenes to oncogenes – Inactivation of tumor suppressor genes 200 Bert Vogelstein’s model of colorectal cancer OMIM175100 201 How does HPV cause cancer? • Gene products of certain sub-type (eg 16 and 18) interfere with normal cellular proteins • Early viral proteins E6 and E7 bind p53 and RB proteins respectively 202 How does HPV cause cancer? 203