Part 5-lecture2
advertisement

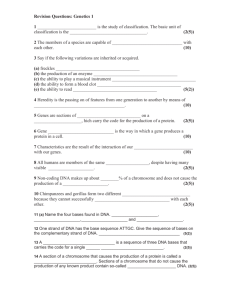
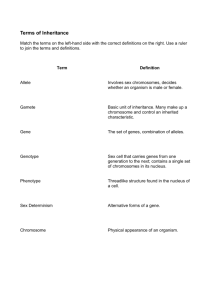
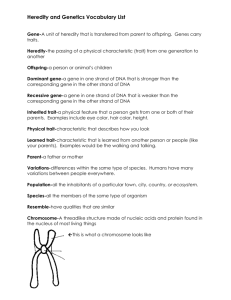
Chapter 18: Genetics of Cancer and Cell-Cycle Regulation What is Cancer? • Large number of complex diseases • Behave differently depending upon cell type from which originate – Age on onset, invasiveness, response to treatment • Common general properties – Abnormal cell growth/division (cell proliferation) • If only this is a benign tumor • When grow in culture without contact inhibition are referred to as transformed – Spread to other regions of body (metastasis) • Malignant tumors Cancer • Second leading cause of disease in Western Countries • 1 million new cases per year in U.S. – 500,000 per year die • War “declared” on cancer approximately 30 years ago • Slowly treatments are changing/improving based upon better genetic understanding of the varieties Cancer Rates in US Age and Cancer • Note log scale for incidence rate Abnormal Cell Growth Cancer is a Genetic Disease • Genome alterations – One nucleotide to large-scale chromosome rearrangements, amplifications and deletions – Mostly in somatic cells (unless associated with inherited risk—about 1% of total) – Alter cellular functions • DNA repair, cell division , apoptosis, cellular differentiation and cell-cell contact/communication Molecular Biology of Neoplasia Retroviral oncogenes: Abl, akt, erbB, ets, fos, kit, myb, myc, raf, ras, rel, src, yes Proto-oncogene: normal gene that can undergo a genetic change to become cancerous. Oncogene: a gene that causes a normal gene to become cancerous. Mutant overactive form of a protooncogene. Tumor suppressor gene: a recessive mutation in an inhibitory gene, thus inactivating the gene. Loss of function causes tumorigenesis. Functions of Cancer Causing Genes/Alleles • Many disrupt control of cell cycle • Oncogenes – Proto-oncogenes • Normal genes that if mutated may act to make a cell cancerous • Recessive, cancer causing forms active and stimulates cell division • C-oncogenes and v-oncogenes • Tumor suppressors – Genes whose products act to regulate cell cycle – Loss of gene product function contributes to cancer process – Recessive, commonly involved with inherited risk • About 200 proto-oncogenes and tumor suppressor genes Oncogenes are identified through their dominant transforming effects Changes observed when a normal tissue culture cell is transformed by a tumor virus or an expression vector carrying the oncogene 1. Alterations in the nucleus 2. Plasmamembrane related abnormalities 3. Adherence abnormalities 4. Growth and division abnormalities 5. Defective differentiation 6. Inability to undergo apoptosis following DNA damage Normal and Cancer Karyotypes • Chromosome painting (a) is a normal cell (b) is a “very messed up” cancer cell Clonal Origin of Tumors • Tumor arises from a single cell • Burkitt’s lymphoma – Translocation involving chromosome 8 (myc) and either chromosomes 2, 14, or 22 (near an immunoglobulin gene – All cells from a patient have breakpoints at exactly the same points as shown by DNA sequence analysis – Cancer cells in tumors of females all use same X chromosome (same one in Barr body) Multistep Process • Cancer requires mutation of multiple genes • Age relationship with cancer consistent with this – If one mutation caused cancer then rate would be constant independent of age • It increases dramatically with age… • Delay between carcinogen exposure and onset – 5-8 year delay between carcinogen exposure (Hiroshima and Nagasaki) and onset of leukemia – 15 year delay between tuberculosis X-ray treatment and onset of breast cancer Multistep Process…Continued • Cancers often develop in progressive steps – From mildly aberrant cells to malignant – See figure 18-3 – Process called tumorigenesis Tumorigenesis of Cervical Cancer Properties of Cancer Cells • Genetic instability – Mutator phenotype – Duplicating, losing and translocating chromosomes or portions of them common • Chronic myelogenous leukemia (CML) – Chromosome 9/chromosome 22 translocation – BCR gene fused to ABL (protein kinase) – Mutant signal transduction protein stimulates cells constantly to proliferate Genome Instability • Double minutes (DMs) – Miniature chromosomes giving many copies of rgion • Homogeneous staining regions (HSRs) – Tandem gene duplications Chromosomal Translocation in CML Xeroderma Pigmentosum • Failure to remove pyrimidine dimers from DNA – Excision repair defect • Patients often develop skin cancer and must stay out of sunlight HFNPCC • Hereditary nonpolyposis colorectal cancer • Higher than normal rates of colon (first noted) but also elevated rates of ovary, uterine and kidney cancers • 1/200 persons, autosomal dominant • Eight genes associated and four involve mismatch repair systems HNPCC Pedigree • Colon, Stomach endometiral, pancreatic, bladder • Orange also other cancers, multiple slashes unknown cause of death Role of cell division in tumor progression Tumors arise from cells with DNA damage or mutant DNA that divide uncontrollably. Cancer cells lose normal restraints for replication of damaged DNA and G1/S progression of cells with damaged DNA. Increased probability of tumor progression by further genetic change. Proto-oncogenes can be converted into oncogenes Proteins that control cell growth (proto-oncogenes and cell cycle checkpoints) 1. Growth factors and receptors: (EGF/EGFR, IGF/IGFR, PDGF/PDGFR) 2. Intracellular transducers: GTP binding proteins: Ras Protein kinases: Src, Raf 3. Intracellular receptors: ER, RAR 4. DNA repair proteins: BRCA1 5. Cell cycle control proteins: cyclins, cdkis, Rb, p53 Proto-oncogene may become converted to an oncogene by a mutation that results in increased intrinsic activity of the protein product 6. Transcription factors: myc, jun. fos, myb 7. Anti apoptotic proteins: Akt, Bcl-2 Defects in Cell Cycle Regulation • Cell cycle • G1, S, G2, M phases • Progression through cycle is regulated and specific blocks or checkpoints exist • Nondividing cell (quiescent) is in an extended G1 phase called G0 – Cancer cells never enter G0 Cell Cycle Cell Cycle Checkpoints • G1/S – Monitors cell size and for DNA damage • G2/M – Replication complete, DNA damage? • M – Spindle fibers connected, etc.? • G0 – Does body require more of my type of cell? Regulators of Cell Cycle • Cyclins and cyclin-dependent kinases (CDKs) • Cyclins synthesized and destroyed in a precise pattern – A cyclin bind to a specific CDKs, activating it • Other proteins phosphorylated/activated • CDK4/cyclinD activate transcription factors for genes such as DNA polymerase delta and DNA ligase • CDK1/cyclinB trigger events of early mitosis (chromosome condensation, nuclear membrane breakdown, etc.) Cell cycle regulatory genes can be oncogenes or tumor suppressors Cyclins as oncogenes 2. Oncogenes that encode growth factors or their receptors Translocation of Tel transcription factor onto PDGF causes dimerization (activation) in the absence of correct ligand. Found in leukemias • mutant receptor – always active even without binding ligand •mutant Gsα – always active – always signaling to adenylate cyclase Steroid hormone receptors as oncogenes: ER, AR, myl (RAR) Steroid hormone receptors can act as nuclear transcription factors and activate transcription of other oncogenes such as cyclins, myc, myb Cyclin Levels Activation of CDKs Tumor Suppressor Genes Mutations in tumor suppressor genes are usually recessive in their effects on the individual cell. 1. Cell Cycle Regulators: • Cdkis (cyclin-depndent kinase inhibitors) • Rb (Retinoblastoma protein) • P53 2. Signaling proteins: APC (adenomatous polyposis coli) 3. DNA damage repair proteins: BRCA1 (Breast cancer gene) 4. Enzymes: PTEN (phosphatase and tensin homolog deleted in chromosome ten) Cell cycle checkpoint proteins regulate G1/S transition A. CDK inhibitors activated by: • P53 (p21 = cip1) • Vitamin D (p21) • Adhesion (p27) • TGFb (p15, p27) B. Rb protein family: pRb, p107, p130 p15 gene Induction of p15 results in inhibition of Cdk4,6/cyclin D complexes and cell cycle arrest at G1. P15 and Smads are tumor suppressors Oncogenes/Proto-oncogenes • Cyclin D1 and Cyclin E are proto-oncogenes – Often amplified or over expressed due to other mutations (e.g. translocation) in many cancers • cyclinD1 allows for DNA replication (S phase) • Over expression seems to contribute to cell’s progression from G0 phase and begin division Oncogenes encoding signaling molecules: ras ERb-B is an oncogene in glioblastomas, renal cell, salivary gland, squamous cell, breast, gastric, ovarian, and esophageal carcinomas Ras is an oncogene in bladder, breast, lung, and head and neck carcinomas Ras is activated by a point mutation in the GTP binding domain Protooncogene First human activated protooncogene Homolog of Harvey-ras and Kirsten-ras from rat sarcoma ras Proto-oncogenes • Involved in signal transduction pathway – As are many proto-oncogene products • ras family genes mutated in 40% of all cancers • Involved in signal transduction pathway from growth factor receptor to nucleus – G protein – Mutant form lacks GTPase activity and remains active • See figure 18-11 Ras Pathway • Growth factor binds receptor • Receptor exchanges GTP for GDP on Ras – Ras activated • RasRafMekMap Kinasetranscription factors genes turned on Mutant Ras Protein • Single amino acid changes create N-ras and K-ras variants p53 Tumor Suppressor Gene • Mutated (inactivated) in more than 50% of all cancers • p53 regulates (activates or represses) transcription of more than 50 different genes • p53 regulated by Mdm2 (prevents the phosphorylations and acetylations that activate inactive p53) • Activated p53 levels rise rapidly if DNA is damaged or repair intermediates accumulate P53 Function • Activated p53 acts as transcription factor to turn on genes that – arrest the cell cycle so DNA can be repaired • Initiates synthesis of p21, which inhibits CDK4/cyuclinD1 complex, blocking entry into S phase • Genes expressed which retard rate of DNA replication • Other products block G2/M progression – Initiate apoptosis if DNA cannot be readily repaired • Turns on Bax gene, represses Bcl2 gene • Bax homodimers activate process of cell destruction • Cancer cells lacking p53 do not initiate pathway even if DNA/cellular damage is great RB1 Tumor Suppressor Gene • Retinoblastoma 1 gene • Involved in breast, bone, lung, bladder and retinal cancers (among others) • Inheriting one mutated (inactivated) copy of gene increases chances of retinoblastoma formation from 1/14,000-20,000 to 85% (plus increases other cancer rates) – Loss of second copy in a cell eliminates function – Normal cells unlikely to lose both good copies pRB Function • Tumor suppressor protein that controls the G1/S checkpoint • Found in nucleus and activity regulated by level of phosphorylation (by CDK4/cyclinD1 complex) – Nonphosphorylated version binds to TFs such as E2F, inactivating them – Free E2F and the other regulators turn on >30 genes required for transition to S phase Familial Retinoblastoma Inherited Predisposition for Cancer • About 1-2% of cancer has an inherited or familial component – 50 different forms known at present • Inherited in Mendelian fashion but most all genes/alleles are recessive – Second copy must be mutated in a somatic cell • Called loss of heterozygosity (and loss of function) • Loss of second copy in germ line lethal • RB1 and APC (lost in FAP, familial adenomatous polyposis) are examples of such genes Multistep Development of Colon Cancer • APC loss causes cells to partially escape cell cycle regulation, DCC seems to be involved in cell adhesion and differentiation Transforming Viruses • Viruses discovered to cause cancer in animals – Acute transforming viruses • Commonly but not always retroviruses – Rous sarcoma virus (RSV) discovered by Francis Peyton Rous discovered in 1910 as a causative agent of chicken sarcomas (solid tumors of muscle, bone or fat) • Many years later shown to be retrovirus • Nobel Prize in 1966 (link of viruses to cancer) Retroviruses • ssRNA chromosome • Chromosome copied to DNA by reverse transcriptase upon entry into cell • DNA integrated into host cell chromosome – Provirus • Provirus has strong promoter elements in U5 and U3 terminal sequences – U5 expresses gag, pol and env • Oncogenic when – Integrate near proto-oncogene and cause inappropriate or over expression – Bring v-onc as part of viral chromosome Retroviruses • Many transforming retroviruses are defective in the sense that one or more of gal/pol/env have been deleted to make room for the v-onc Viral Oncogenes • Most v-onc genes have normal cellular counterparts – If simply mutated to the oncogenic form and not in a virus are called c-onc Human Cancer-Associated Viruses • To date no acute transforming retroviruses have been discovered in humans – Viruses can contribute to but not be the sole cause of human cancer – However, up to 15% of all cancers have a viral association • Papillomaviruses HPV 16 and 18, hepatitis B virus, Epstein-Barr virus, Human T-cell leukemia virus are examples of cancer-associated viruses Human Viruses Associated With Cancer • Non-retroviral varieties • Many of these v-onc genes act to stimulate the cell cycle (viruses needs host replication apparatus to multiply V-onc Gene Product Action • Some v-onc gene products have their transforming effect by binding and thereby “taking out” certain tumor suppressor gene products – Cell division required to provide replication apparatus for virus – Bad, but does open some interesting treatment possibilities… Environmental Agents and Cancer • Natural and man-made carcinogens – Chemicals, radiation, chronic infections • 30% of cancer deaths associated with cigarettes – Seems to preferentially mutate proto-oncogene and tumor suppressor genes • Red meat consumption – How cooked? • Alcohol-based inflammation of the liver • Aflatoxin (mold on peanuts) • UV light or ionizing radiation – Radon gas (up to 50% of radiation exposure???) Oncogenes that code for cytoplasmic protein kinases involved in cell proliferation: src, raf Ras activates Raf kinase. Raf activates MAPKs. MAPKs phosphorylate and activate transcription factors Elk-1, SRF, AP-1 that regulate Cyclin expression Oncogenes that encode nuclear transcription factors: AP-1: fos, jun Translocation of c-myc in Burkitt’s lymphoma •Translocation of c-myc transcription factor gene to Ig loci • c-myc normally induced in response to growth factors •Translocation results in constitutive activation because of being under control of Ig promoters of the B-cells Oncogenes that code for cytoplasmic protein kinases involved in cell proliferation: abl Chronic myelogenous leukemia (CML) is a clonal hematopoetic stem cell disorder The cytogenetic hallmark of all phases of CML is the Philadelphia (Ph) chromosome. The Ph chromosome is a shortened chromosome 22 that results from a reciprocal translocation between chromosomes 9 and 22. Fusion of the c-abl oncogene from chromosome 9 with sequences from chromosome 22, the breakpoint cluster region (bcr) gives fused bcr-abl gene. Conversion of abl-protooncogene into an oncogene in myelogenous leukemia Depending on the site of the breakpoint in bcr, different fusion proteins are produced: p185 (185 kDa), p210 (210 kDa), or rarely p230. How does bcr-Abl fusion protein expression cause leukemia? c-abl, the cellular homolog of the transforming protein found in the Abelson murine leukemia virus (v-abl), encodes for a nonreceptor tyrosine kinase. The c-abl protein has tightly regulated kinase activity and shuttles between the nucleus and cytoplasm. Abl is a Src family tyrosine kinase that has SH2, SH3 domains and can activate MAPK signaling. bcr-abl fusion proteins are exclusively cytoplasmic and have enhanced tyrosine kinase activity that causes excess proliferation of myeloid cells. Genetic mechanisms underlying Retinoblastoma How to lose the remaining good copy of a tumor suppressor gene Rb mechanism of action in cell cycle regulation Phosphorylation of Rb by Cdk results in activation of E2F family transcription factors Cyclins No functional Rb = no inhibition of E2F activity = unchecked cell division • Li-Fraumeni syndrome (LFS) is a cancer predisposition syndrome associated with soft-tissue sarcoma, breast cancer, leukemia, osteosarcoma, melanoma, and cancer of the colon, pancreas, adrenal cortex, and brain. Individuals with LFS are at increased risk for developing multiple primary cancers. • More than 50% of individuals diagnosed clinically have an identifiable diseasecausing mutation in the P53 gene. Of these mutations, 95% can be detected by sequence analysis, • Genetic counseling. LFS is inherited in an autosomal dominant manner. Offspring of an affected individual have a 50% chance of inheriting the diseasecausing mutation. DNA damage induces p53 expression P53 mechanism of action in cell cycle regulation DNA damage increases p53 expression of normal cells. P53 acts as a transcription factor to induce p21 (cip1), a cdki. Blocks cell cycle progression. If the DNA damage cannot be repaired p53 will induce transcription of Bax, PUMA, proapoptotic Bcl-2 family members. Cell cycle regulation by tumor suppressors Bax, Noxa, PUMA Fas DR4,5 Replication of damaged DNA can lead to chromosomal abnormalities, gene amplification, and gene loss APC = adaptor, brings GSK-3 close to β-catenin so it can be Phosphorylated and degraded No APC = lots free β-catenin = increase in gene transcription = cell proliferation DNA damage repair by BRCA1 This pathway is dysfunctional in some breast cancers BRCA, the breast cancer gene, missing in only 5% of breast cancers, BRCA (-) genotype has 60% risk of breast cancer by age 70. ATM, ataxia-telangiectasia mutated Suppression of cell survival by PTEN Genetic Alterations in Colon Carcinoma 1. Loss of APC leads to early adenoma 2. Constitutive activation of ras leads to intermediate adenoma 3. Loss of smads and TGFbR lead to late adenoma 4. Loss of p53 leads to carcinoma 5. Other alterations can lead to metastasis Apoptosis • Programmed cell death, cell suicide • Pathway should be activated if “something goes wrong” – Especially involving DNA/chromosome damage • Involves proteases called caspases • Regulated by Bcl2 and BAX – BAX homodimer promotes apoptosis, Bcl2 homodimer blocks apoptosis – Some cancer cells overproduce Bcl2 and are resistant to some chemotherapies and radiation treatment • Proteins involved in cell cycle checkpoints regulate pathway Control of Apoptosis Oncogenes encoding products that affect apoptosis TRANSFORMATION Initial event PROMOTION Immortalization Altered DNA repair Inhibition of apoptosis Successive accumulation of mutations Cell cycle promotion Inhibition of apoptosis PROGRESSION Genomic instability Other mutations Irregular expression of apoptosis Drug resistance Two Major Pathways of Apoptosis: 1. Receptor-regulated 2. Mitochondrial From: “The biochemistry of apoptosis” Hengartner, 2000 Nature 407:770-776 Differentiation, development and programmed cell death.1999, The molecular basis of cell cycle and growth control. Ed. Stein, Baserga and Denhardt, 305-307, WileyLiss, Inc. Oncogneic activity of Bcl-2 and Bcl-xL Structure of Bcl-XL with a BH3 peptide bound. Adams and Cory, 1998. Science 281:1322-1326. APaf-1= apoptosis protease activating factor-1 CARD=caspase recruitment domain Apoptosome: contains cytochrome C, ATP, caspase9, APaf-1 Oncogenes encoding cell survival signals: akt Akt activity in blocking apoptosis