Medical Law/Application Process
Medical
Law/Application
Process
Classification of Law (2)
Criminal (“Penal”) Law
Relates to crime
Rules that define prohibited conduct because [that conduct] is believed to threaten, harm, or otherwise
damage the safety & welfare of the public.
Punishment: Imprisonment & Fines
Civil Law
Legal rights and responsibilities (duties) of private citizens
Punishment: Money awards
Legal Torts
“Legal or civil wrong committed by one person against the person or property of another person”
Two (2) Types
Intentional
Negligence
Intentional Tort of Misconduct
Plaintiff must establish that the defendant
intended to commit the specific wrong that has been alledged.
Must be conscious performance of act to accomplish specific result, or where a reasonable person would have known the results of a particular act.
Deliberate action
Conscious action
Plaintiff must show intent
Misconduct (types)
Assault
Acting intentionally & voluntarily causing the reasonable apprehension of an immediate harmful or offensive contact
Intent
Apprehension
Battery
Intentionally & voluntarily bringing about an unconsented harmful or offensive contact with a person
Involves actual contact
Misconduct (types)
False Imprisonment
Conscious restraint of freedom of another without proper authorization, priviledge, or consent
In healthcare must be limited to, and in proportion with the procedure being performed.
Based on “reasonableness”
Misconduct (types)
Defamation of Character
Slander – spoken
Libel – written
Must be written or spoken, and made to a person other than the plaintiff
Invasion of Privacy
Patient’s medical record (includes x-ray images)
Freedom of Information Act (pt can access records)
Covered by HIPAA Laws (PHI)
Standard of Care
“Skill and learning commonly possessed by members of a particular profession.”
In healthcare known as “Standard of
Reasonable Care”
Depends on specifics of situation
Open to interpretation by judge & jury
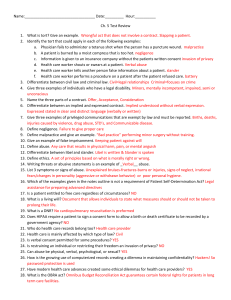
Tort of Negligence
“Doing something you should not have done” or
“Not doing something that you should have done.”
Negligent behavior or actions that cause harm to another person known as
“malpractice.”
Hippocratic Oath: “Do no harm”
Medical Negligence =
Malpractice
Def: “A breach from the standard practice that is the proximate cause of a patient’s injury.”
Elements of proof of negligence in a medical malpractice case include a deviation, or
departure from acceptable standard of practice
A negligent act committed by a professional person constitutes malpractice only if it involves negligence in the carrying out of his professional duties
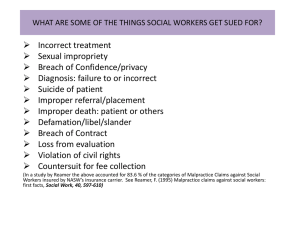
Malpractice classifications
Criminal Malpractice
Assault
Battery
Mercy Killing (“Angel of Death”)
Civil Malpractice
Practice falls below “Standard of Care”
Ethical Malpractice
Violations of professional ethics (e.g. ASRT Code
of Ethics)
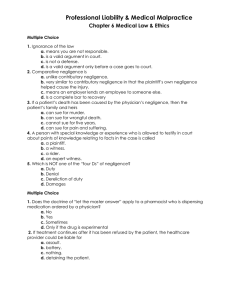
Malpractice: Plaintiff must prove
1.
2.
3.
4.
Duty of responsibility to patient owed
Duty of responsibility is breached (broken)
Damages (Injury or Death)
Proximal (Direct) Cause
Malpractice: Plaintiff must prove
1.
2.
3.
4.
Duty of responsibility to patient owed
Duty of responsibility is breached (broken)
Damages (Injury or Death)
Proximal (Direct) Cause
Medico-Legal Doctrines
Respondeat superior
“Let the master respond”
Employer is liable for negligent acts of employees which occur when the employee is acting as an instrument of the employer.
Employee-Employer relationship must exist
Does not relieve practitioner of negligent behavior
“Indemnification”
Employer can recover awarded damages from its employee
Medico-Legal Doctrines
Res ipsa loquitur
“The thing speaks for itself”
Often invoked to cause the defendant to prove his actions were not negligent (accused my prove that he is innocent)
The outcome is so obvious that the damage(s) can only have been caused by the defendant.
e.g. sponges & instruments left inside patients, surgical outcomes (esp. plastic surgery) that didn’t turn out right, wrong medications administered to the patient.
Medico-Legal Doctrines
Corporate Liability
Duty of reasonable care in selection and retention of employees and medical staff
Duty of reasonable care in maintenance and use of equipment
Availability of services
Informed Consent
Affirmation by patient to consent to have procedure performed
Patient must have:
Appropriate mental capacity
Accepted elements of consent
Been for lawful purpose
Who can sign?
Must be over age of majority
Spouse
Emancipated Minor
Informed Consent must contain:
Authorization Clause
Permits healthcare giver to perform procedure
Disclosure Clause
Explanation of procedure
Risks – to include possibility of death
Benefits of having procedure performed
Alternatives
Anesthesia Clause (if anesthesia to be given)
Informed Consent must contain:
No guarantee clause
Tissue Disposal Clause
Patient Understanding Clause
Had all questions answered
Everything explained to patient
Signature Clause
Patient signature or mark
Witness
The lack of a signed Informed
Consent form constitutes medical malpractice!
(Deviation from “Standard of
Practice”)
Child Abuse
“Abuse” vs “Neglect”
Abuse: Positive action, very distinct, aggravated
Neglect: Failing to do something you should
Punishment
Abuse: Child removed from family
Neglect: DFS/DCWS work with family, counselling
Not reporting suspected child abuse
Civil Liability
California Supreme Court (1976) – Landeros v.
Flood
Sued ER physician (Flood) & hospital for malpractice because they had a duty to recognize battered child syndrome.
Required by law to report suspected child abuse
Immunity Provision
Immunity does not apply for malicious reporting
Laws you should know about:
Radiologic Technology Act (1974)
Calif Code of Regulations (CCR) Title XVII
Health Insurance Portability & Accountability
Act (HIPAA)
Passed 1996; became fully effective 2003
Privacy of patient information (PHI)
10 CFR 20 – NRC (1994)
“Standards for Protection Against Radiation”
Laws you should know about:
Mammographic Quality Standards Act (1992, renewed 2003) – “MQSA”
Patient-Consumer Radiation Health & Safety Act
(1981)
National educational & credentialing standards for RT training (Sec. HHS)
Compliance was voluntary
Did not specify “penalties” for non-compliance
Law was unenforceable
Didn’t do what it was intended to do
Laws you should know about:
Consistency, Accuracy, Responsibility & Excellence in Medical Imaging (CARE) Bill
Originally discussed as an enforcement clause in the
1981 Act.
Compliance mandatory - tied to MediCare/MediCAID reimbursement to force compliance
1997 – ASRT votes to advocate federally mandated standard for education & credentialing
1999 - First introduced as a Congressional bill
2011 - Still pending Congressional passage (H.R. 1207)
Laws you should know about:
Calif SB 1237
Procedures to protect patients from radiation overexposure (ref CT Scans) – signed into law October
2010.
Requires:
◦
◦
CT Scan Dose reporting
CT Facility accreditation
◦
◦
Medical event reporting to DPH
Effective July1,2012