homeostatic imbalance
advertisement

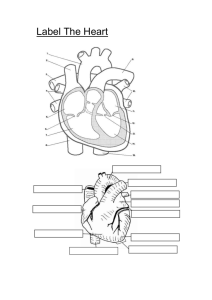
The cardiovascular system • The cardiovascular system provides the transport system that keeps blood continuously circulating. The heart is no more than the transport system pump; the hollow blood vessels are the delivery routes. • Using blood as the transport medium, the heart continually propels oxygen, nutrients, wastes, and many other substances into the blood vessels that service body cells. Heart Anatomy Size, Location, and Orientation About the size of a fist, the hollow, cone-shaped heart has a mass of between 250 and 350 grams—less than a pound. enclosed within the mediastinum (me″de-ah-sti′num), the medial cavity of the thorax, the heart extends obliquely for 12 to 14 cm (about 5 inches) from the second rib to the fifth intercostal space . As it rests on the superior surface of the diaphragm, the heart lies anterior to the vertebral column and posterior to the sternum. If you press your fingers between the fifth and sixth ribs just below the left nipple, you can easily feel your heart beating where the apex contacts the chest wall. Hence, this site is referred to as the point of maximal intensity (PMI). The lungs flank the heart laterally and partially obscure it. Approximately two-thirds of its mass lies to the left of the midsternal line. Its broad, flat base, or posterior surface, is about 9 cm (3.5 in) wide and directed toward the right shoulder. Its apex points inferiorly toward the left hip. Coverings of the Heart The heart is enclosed in a double-walled sac called the pericardium. The loosely fitting superficial part of this sac is the fibrous pericardium. This tough, dense connective tissue layer (1) protects the heart, (2) anchors it to surrounding structures, and (3) prevents overfilling of the heart with blood. Deep to the fibrous pericardium is the serous pericardium, a thin, slippery, two-layer serous membrane. Its parietal layer lines the internal surface of the fibrous pericardium. At the superior margin of the heart, the parietal layer attaches to the large arteries exiting the heart, and then turns inferiorly and continues over the external heart surface as the visceral layer, also called the epicardium (“upon the heart”), which is an integral part of the heart wall. Between the parietal and visceral layers is the slitlike pericardial cavity, which contains a film of serous fluid. The serous membranes, lubricated by the fluid, glide smoothly past one another during heart activity, allowing the mobile heart to work in a relatively friction-free environment HOMEOSTATIC IMBALANCE Pericarditis, inflammation of the pericardium, roughens the serous membrane surfaces. Pericarditis is characterized by pain deep to the sternum. Over time, it may lead to adhesions in which the visceral and parietal pericardia stick together and impede heart activity. In severe cases, excess fluid compresses the heart, limiting its ability to pump blood. This condition in which the heart is compressed by fluid is called cardiac tamponade (tam″pŏ-nād′). Physicians treat it by inserting a syringe into the pericardial cavity and draining off the excess fluid. Layers of the Heart Wall The heart wall is composed of three layers : 1-The superficial epicardium is the visceral layer of the serous pericardium. It is often infiltrated with fat, especially in older people. 2-The middle layer, the myocardium (“muscle heart”), is composed mainly of cardiac muscle and forms the bulk of the heart. It is the layer that contracts. 3-The third layer, the endocardium (“inside the heart”), is a glistening white sheet of endothelium (squamous epithelium) resting on a thin connective tissue layer. Located on the inner myocardial surface, it lines the heart chambers and covers the fibrous skeleton of the valves. The endocardium is continuous with the endothelial linings of the blood vessels leaving and entering the heart. Chambers and Associated Great Vessels The heart has four chambers ,two superior atria (a′tre-ah) and two inferior ventricles (ven′trĭ-klz). The internal partition that divides the heart longitudinally is called the interatrial septum where it separates the atria, and the interventricular septum where it separates the ventricles. The right ventricle forms most of the anterior surface of the heart. The left ventricle dominates the inferoposterior aspect of the heart and forms the heart apex. The coronary sulcus or atrioventricular groove, encircles the junction of the atria and ventricles like a crown (corona = crown). Atria: The Receiving Chambers Except for small, wrinkled, protruding appendages called auricles (or′ĭ-klz; auricle = little ear), which increase the atrial volume somewhat, the right and left atria are remarkably free of distinguishing surface features. The interatrial septum bears a shallow depression, the fossa ovalis (o-vă′lis), that marks the spot where an opening, the foramen ovale, existed in the fetal heart . Atria are receiving chambers for blood returning to the heart from the circulation .Because they need contract only minimally to push blood “downstairs” into the ventricles, the atria are relatively small, thinwalled chambers. As a rule, they contribute little to the propulsive pumping activity of the heart. -Blood enters the right atrium via three veins : (1) The superior vena cava returns blood from body regions superior to the diaphragm; (2) (2) the inferior vena cava returns blood from body areas below the diaphragm; and (3) (3) the coronary sinus collects blood draining from the myocardium. - Four pulmonary veins enter the left atrium, which makes up most of the heart’s base. Ventricles: The Discharging Chambers Together the ventricles make up most of the volume of the heart. The conelike papillary muscles, which play a role in valve function, project into the ventricular cavity. The ventricles are the discharging chambers or actual pumps of the heart .When the ventricles contract, blood is propelled out of the heart into the circulation. -The right ventricle pumps blood into the pulmonary trunk, which routes the blood to the lungs where gas exchange occurs. -The left ventricle ejects blood into the aorta (a-or′tah), the largest artery in the body. Pathway of Blood Through the Heart The heart is actually two side-by-side pumps, each serving a separate blood circuit. • The blood vessels that carry blood to and from the lungs form the pulmonary circuit (pulmonos = lung), which serves gas exchange. • The blood vessels that carry the functional blood supply to and from all body tissues constitute the systemic circuit. The right side of the heart is the pulmonary circuit pump. Blood returning from the body is relatively oxygen-poor and carbon dioxide–rich. It enters the right atrium and passes into the right ventricle, which pumps it to the lungs via the pulmonary trunk . -In the lungs, the blood unloads carbon dioxide and picks up oxygen. The freshly oxygenated blood is carried by the pulmonary veins back to the left side of the heart. -Typically, we think of veins as vessels that carry blood that is relatively oxygen-poor to the heart and arteries as transporters of oxygen-rich blood from the heart to the rest of the body. -Exactly the opposite condition exists in the pulmonary circuit. The left side of the heart is the systemic circuit pump. Freshly oxygenated blood leaving the lungs is returned to the left atrium and passes into the left ventricle, which pumps it into the aorta. From there the blood is transported via smaller systemic arteries to the body tissues, where gases and nutrients are exchanged across the capillary walls. Then the blood, once again loaded with carbon dioxide and depleted of oxygen, returns through the systemic veins to the right side of the heart, where it enters the right atrium through the superior and inferior venae cavae. Although equal volumes of blood are pumped to the pulmonary and systemic circuits at any moment, the two ventricles have very unequal workloads. The pulmonary circuit, served by the right ventricle, is a short, low-pressure circulation, whereas the systemic circuit, associated with the left ventricle, takes a long pathway through the entire body and encounters about five times as much friction, or resistance to blood flow. This functional difference is revealed in the anatomy of the two ventricles .The walls of the left ventricle are three times as thick as those of the right ventricle, and its cavity is nearly circular. Consequently, the left ventricle can generate much more pressure than the right and is a far more powerful pump. Coronary Circulation The coronary circulation, the functional blood supply of the heart, is the shortest circulation in the body. The arterial supply of the coronary circulation is provided by the right and left coronary arteries, both arising from the base of the aorta and encircling the heart in the coronary sulcus. HOMEOSTATIC IMBALANCE Blockage of the coronary arterial circulation can be serious and sometimes fatal. Angina pectoris is thoracic pain caused by a fleeting deficiency in blood delivery to the myocardium. The myocardial cells are weakened by the temporary lack of oxygen but do not die. Myocardial infarction (MI), is far more serious is prolonged coronary blockage. Because adult cardiac muscle is essentially amitotic, most areas of cell death are repaired with noncontractile scar tissue. Whether or not a person survives a myocardial infarction depends on the extent and location of the damage. Damage to the left ventricle, which is the systemic pump, is most serious. • Heart Valves Blood flows through the heart in one direction: from atria to ventricles and out the great arteries leaving the superior aspect of the heart. This one-way traffic is enforced by four valves that open and close in response to differences in blood pressure on their two sides. Atrioventricular Valves The two atrioventricular (AV) valves, one located at each atrialventricular junction, prevent backflow into the atria when the ventricles are contracting. • The right AV valve, the tricuspid valve has three flexible cusps • The left AV valve, with two flaps, is called the mitral valve (mi′tral). It is sometimes called the bicuspid valve. • Attached to each AV valve flap are tiny white collagen cords called chordae tendineae “heart strings” which anchor the cusps to the papillary muscles protruding from the ventricular walls. • When the heart is completely relaxed, the AV valve flaps hang limply into the ventricular chambers below and blood flows into the atria and then through the open AV valves into the ventricles. When the ventricles contract, compressing the blood in their chambers, the intraventricular pressure rises, forcing the blood superiorly against the valve flaps. As a result, the flap edges meet, closing the valve .The chordae tendineae and the papillary muscles serve to anchor the valve flaps in their closed position. If the cusps were not anchored in this manner, they would be blown upward into the atria, in the same way an umbrella is blown inside out by a gusty wind. • Semilunar Valves The aortic and pulmonary (semilunar, SL) valves guard the bases of the aorta and pulmonary trunk, respectively and prevent backflow into the associated ventricles. • Each SL valve is fashioned from three pocketlike cusps, each shaped roughly like a crescent moon . • Like the AV valves, the SL valves open and close in response to differences in pressure. In the SL case, when the ventricles are contracting and intraventricular pressure rises above the pressure in the aorta and pulmonary trunk, the SL valves are forced open . • When the ventricles relax, and the blood (no longer propelled forward by the pressure of ventricular contraction) flows backward toward the heart, it fills the cusps and closes the valves. HOMEOSTATIC IMBALANCE Heart valves—like any mechanical pump—can function with “leaky” valves as long as the impairment is not too great. An incompetent valve forces the heart to repump the same blood over and over because the valve does not close properly and blood backflows. In valvular stenosis (“narrowing”), the valve flaps become stiff and constrict the opening. This stiffness compels the heart to contract more forcibly than normal. In both instances, the heart’s workload increases and, ultimately, the heart may be severely weakened. Under such conditions, the faulty valve (most often the mitral valve) is replaced . Cardiac muscle structure Heart Physiology -The ability of cardiac muscle to depolarize and contract is intrinsic; that is, it is a property of heart muscle and does not depend on the nervous system. Even if all nerve connections to the heart are severed, the heart continues to beat rhythmically (as demonstrated by transplanted hearts). -Nevertheless,the healthy heart is amply supplied with autonomic nerve fibers that can alter the basic rhythm of heart activity set by intrinsic factors. Setting the Basic Rhythm: The Intrinsic Conduction System The independent activity consists of noncontractile cardiac cells specialized to initiate and distribute impulses throughout the heart in an orderly, sequential manner. Thus, the heart beats as a coordinated unit. Sequence of Excitation 1-Sinoatrial node. The crescent-shaped sinoatrial (SA) node is located in the right atrial wall, just inferior to the entrance of the superior vena cava. A minute cell mass with a mammoth job, the SA node typically generates impulses about 75 times every minute. (However, its inherent rate in the absence of extrinsic neural and hormonal factors is closer to 100 times per minute.) Because no other region of the conduction system or the myocardium has a faster depolarization rate, the SA is the heart’s pacemaker, and its characteristic rhythm, called sinus rhythm, determines heart rate. 2-Atrioventricular node. From the SA node, the depolarization wave spreads to the atrioventricular (AV) node, located in the inferior portion of the interatrial septum immediately above the tricuspid valve. At the AV node, the impulse is delayed allowing the atria to respond and complete their contraction before the ventricles contract. Once through the AV node, the signaling impulse passes rapidly through the rest of the system. 3-Atrioventricular bundle. From the AV node, the impulse sweeps to the atrioventricular (AV) bundle (also called the bundle of His) in the superior part of the interventricular septum. 4- Right and left bundle branches. The AV bundle persists only briefly before splitting into two pathways—the right and left bundle branches, which course along the interventricular septum toward the heart apex. 5- Purkinje fibers complete the pathway through the interventricular septum, penetrate into the heart apex, and then turn superiorly into the ventricular walls. HOMEOSTATIC IMBALANCE Defects in the intrinsic conduction system can cause irregular heart rhythms, or arrhythmias (ah-rith′meahz): fibrillation, a condition caused by ischemia . It is a rapid and irregular contractions in which control of heart rhythm is taken away from the SA node by rapid activity in other heart regions. The heart in fibrillation has been compared with a squirming bag of worms. Fibrillating ventricles are useless as pumps; and unless the heart is defibrillated quickly, circulation stops and brain death occurs. Defibrillation is accomplished by electrically shocking the heart.The hope is that the SA node will begin to function normally and sinus rhythm will be reestablished. • Because the only route for impulse transmission from atria to ventricles is through the AV node, any damage to the AV node, referred to as a heart block. -In total heart block no impulses get through and the ventricles beat at their intrinsic rate, which is too slow(20-40/min) to maintain adequate circulation. -In partial heart block, only some of the atrial impulses reach the ventricles. In both cases, pacemakers are used to recouple the atria to the ventricles as necessary. Modifying the Basic Rhythm: Extrinsic Innervation of the Heart • The sympathetic nervous system (the “accelerator”) increases both the rate and the force of heartbeat. • The Parasympathetic activation (the “brakes”) slows the heart. It sends inhibitory impulses to the heart via branches of the vagus nerves. The cardiac centers are located in the medulla oblongata (cardioacceleratory center and cardioinhibitory center ) • They sends impulses to the SA and AV nodes. Electrocardiography The electrical currents generated in and transmitted through the heart spread throughout the body and can be detected with an electrocardiograph. A graphic record of heart activity is called an electrocardiogram .An ECG is a composite of all the action potentials generated by nodal and contractile cells at a given time and not, as sometimes assumed, a tracing of a single action potential. A typical ECG has three waves : 1-The first, the small P wave, lasts about 0.08 s and results from movement of the depolarization wave from the SA node through the atria. 2-The large QRS complex results from ventricular depolarization. It has a complicated shape because the paths of the depolarization waves through the ventricular walls change continuously, producing corresponding changes in current direction. 3- The T wave is caused by ventricular repolarization. Because atrial repolarization takes place during the period of ventricular excitation, the wave representing atrial repolarization is normally obscured by the large QRS complex being recorded at the same time. Heart Sounds During each heartbeat, two sounds can be distinguished when the thorax is auscultated (listened to) with a stethoscope. These heart sounds, often described as lub-dup, are associated with closing of heart valves. The basic rhythm of the heart sounds is lub-dup, pause, lub-dup, pause, and so on. • The first sound, which occurs as the AV valves close, signifies the point when ventricular pressure rises above atrial pressure .The first sound tends to be louder, longer, and more resonant than • the second sound, which is a short and sharp sound heard as the SL valves close at the beginning of ventricular relaxation (diastole). HOMEOSTATIC IMBALANCE Blood flows silently as long as the flow is smooth and uninterrupted. If it strikes obstructions, however, its flow becomes turbulent and generates heart murmurs that can be heard with a stethoscope. • Heart murmurs are fairly common in young children (and some elderly people) with perfectly healthy hearts, probably because their heart walls are relatively thin and vibrate with rushing blood. • Most often, however, murmurs indicate valve problems. If a valve is incompetent, a murmur is heard as the blood backflows or regurgitates through the valve. • A stenotic valve, in which the valvular opening is narrowed, restricts blood flow through the valve. Mechanical Events: The Cardiac Cycle The heart alternately contracts, forcing blood out of its chambers, and then relaxes, allowing its chambers to refill with blood. The terms systole (sis′to-le) and diastole (di-as′to-le) refer respectively to these contraction and relaxation periods. The cardiac cycle includes atrial systole and diastole followed by ventricular systole and diastole`(one complete heart beat). These mechanical events always follow the electrical events seen in the ECG. The average heart beats approximately 75 times per minute , so the length of the cardiac cycle is normally about 0.8 seconds. Cardiac output (CO) is the amount of blood pumped out by each ventricle in 1 minute. It is the product of heart rate (HR) and stroke volume (SV). Stroke volume is defined as the volume of blood pumped out by one ventricle with each beat. In general, stroke volume is correlated with the force of ventricular contraction. Using normal resting values for heart rate (75 beats/min) and stroke volume (70 ml/beat), the average adult cardiac output is about 5 L.(heart rate x stroke volume) Thus, the entire blood supply passes through each side of the heart once each minute. Notice that cardiac output varies directly with SV and HR. Thus CO increases when the stroke volume increases or the heart beats faster or both, and decreases when either or both of these factors decrease. Regulation of Heart Rate 1- When blood volume drops sharply or when the heart is seriously weakened, SV declines and CO is maintained by increasing HR and contractility. 2 -Temporary stressors can also influence HR— and consequently CO—by acting through homeostatic mechanisms induced neurally, chemically, and physically. a-Autonomic Nervous System Regulation The most important extrinsic controls affecting heart rate. -When the sympathetic nervous system is activated by emotional or physical stressors, such as fright, anxiety, or exercise ,sympathetic nerve fibers release norepinephrine. As a result, the pacemaker fires more rapidly and the heart responds by beating faster. -The parasympathetic division opposes sympathetic effects and effectively reduces heart rate when a stressful situation has passed. Cutting the vagal nerves results in an almost immediate increase in heart rate of about 25 beats/min, reflecting the inherent rate (100 beats/min) of the pacemaking SA node. b-Chemical Regulation 1. Hormones. -Epinephrine, liberated by the adrenal medulla during sympathetic nervous system activation, enhances heart rate and contractility. -Thyroxine is a thyroid gland hormone that increases metabolic rate and body heat production and heart rate. 2. Ions. Plasma electrolyte imbalances pose real dangers to the heart. - Low calcium(hypocalcemia) depress the heart - Excessive K+ (hyperkalemia) may lead to heart block and cardiac arrest c-Other Factors -age,, and also influence HR. Resting heart rate is fastest in the fetus (140–160 beats/min) and gradually declines throughout life. - gender,, average heart rate is faster in females (72–80 beats/min) than in males (64–72 beats/min). - Exercise raises HR by acting through the sympathetic nervous system . However, resting HR in the physically fit tends to be as slow as 40 beats/min. - body temperature increases HR by enhancing the metabolic rate of cardiac cells. This explains the rapid, pounding heartbeat you feel when you have a high fever and also accounts, in part, for the effect of exercise on HR (remember, working muscles generate heat). Cold directly decreases heart rate. HOMEOSTATIC IMBALANCE Although HR varies with changes in activity, marked and persistent rate changes usually signal cardiovascular disease. • Tachycardia (take-kar′de-ah; “heart hurry”) is an abnormally fast heart rate (more than 100 beats/min) that may result from elevated body temperature, stress, certain drugs, or heart disease. Because tachycardia occasionally promotes fibrillation, persistent tachycardia is considered pathological. • Bradycardia (brade-kar′de-ah; brady = slow) is a heart rate slower than 60 beats/min. It may result from low body temperature, certain drugs, or parasympathetic nervous activation. It is a known, and desirable, consequence of endurance training. Homeostatic Imbalance of Cardiac Output -The heart’s pumping action ordinarily maintains a balance between cardiac output and venous return. Were this not so, blood congestion would occur in the veins returning blood to the heart. - When the pumping efficiency (CO) of the heart is so low that blood circulation is inadequate to meet tissue needs, the heart is said to be in congestive heart failure (CHF). It occurs in: 1. Coronary atherosclerosis 2. Persistent high blood pressure 3. Multiple myocardial infarcts Because the heart is a double pump, each side can initially fail independently of the other. - If the left side fails, The right side continues to propel blood to the lungs, but the left side does not adequately eject the returning blood into the systemic circulation. causing pulmonary edema. If the congestion is untreated, the person suffocates - If the right side of the heart fails, peripheral congestion occurs. Blood stagnates in body organs, and pooled in the extremities (feet, ankles, and fingers). Failure of one side of the heart puts a greater strain on the other side, and ultimately the whole heart fails. OVERVIEW OF BLOOD VESSEL STRUCTURE AND FUNCTION The blood vessels of the body form a closed delivery system that begins and ends at the heart. The three major types of blood vessels are : 1- the arteries, capillaries, and veins. As the heart contracts, it forces blood into the large arteries leaving the ventricles. The blood then moves into successively smaller arteries, finally reaching their smallest branches, the arterioles (arte′re-ōlz; “little arteries”), which feed into 2-the capillary beds of body organs and tissues. Blood drains from the capillaries into 3-the venules (ven′ūlz), the smallest veins, and then on into larger and larger veins that merge to form the large veins that ultimately empty into the heart. - Altogether, the blood vessels in the adult human stretch for about 100,000 km (60,000 miles) . Structure of Blood Vessel Walls • • • • • The walls of all blood vessels, except the very smallest, have three distinct layers, or tunics : The walls of arteries and veins are composed of the tunica intima (endothelium underlain by loose connective tissue), the tunica media (smooth muscle cells and elastic fibers), and the tunica externa (largely collagen fibers). Capillaries are composed of only of simple squamous epithelium on a basement membrane. Depending on the body’s needs at any given moment, either vasoconstriction (reduction in lumen diameter as the smooth muscle contracts) or vasodilation (increase in lumen diameter as the smooth muscle relaxes) can be effected. The arterial wall is thicker , more circular , with less diameter than the corresponding vein. Large vein also has valves and large arteries are able to expand and recoil. venous return Venous pressure is normally too low to promote adequate venous return. Hence, three factors are critically important to venous return: 1-the respiratory “pump.” As we inhale, abdominal pressure increases, squeezing the local veins and forcing blood toward the heart. At the same time, the pressure in the chest decreases, allowing thoracic veins to expand and speeding blood entry into the right atrium. 2- the muscular “pump.” Skeletal muscle activity, or the so-called muscular pump, is the more important pumping mechanism. As the skeletal muscles surrounding the deep veins contract and relax, they “milk” blood toward the heart, and once blood passes each successive valve, it cannot flow back. 3- the valves in the large veins. HOMEOSTATIC IMBALANCE • Varicose veins are veins that have become tortuous and dilated because of incompetent (leaky) valves. More than 15% of adults suffer from varicose veins, usually in the lower limbs. Several factors contribute, including heredity ,prolonged standing, obesity, or pregnancy. Consequently, blood pools in the lower limbs, and the venous walls stretch and become floppy. • A serious complication is thrombophlebitis, inflammation of a vein that results when a clot forms in a vessel with poor circulation . • The clot may detach and pulmonary embolism may occur. The muscular pump. When contracting skeletal muscles press against a vein, the valves proximal to the area of contraction are forced open and blood is propelled toward the heart. The valves distal to the area of contraction are closed by the back flowing blood. ANASTOMOSES • An anastomosis is a connection, or joining, of vessels, that is, artery to artery or vein to vein. The general purpose of these connections is to provide alternate pathways for the flow of blood if one vessel becomes obstructed. An arterial anastomosis helps ensure that blood will get to the capillaries of an organ to deliver oxygen and nutrients and to remove waste products. • There are arterial anastomoses, for example, between some of the coronary arteries that supply blood to the myocardium. • A venous anastomosis helps ensure that blood will be able to return to the heart in order to be pumped again. Venous anastomoses are most numerous among the veins of the legs, where the possibility of obstruction increases as a person gets older. CAPILLARIES Capillaries carry blood from arterioles to venules. Their walls are only one cell in thickness; capillaries are actually the extension of the endothelium, the simple squamous lining, of arteries and veins. -Some tissues do not have capillaries; these are the epidermis, cartilage, and the lens and cornea of the eye. - Most tissues, however, have extensive capillary networks. The quantity or volume of capillary networks in an organ reflects the metabolic activity of the organ. The functioning of the kidneys, for example, depends upon a good blood supply. The vessels in kidneys are dense, most of which are capillaries. In contrast, a tendon such as the Achilles tendon at the heel or the patellar tendon at the knee would have far fewer vessels, because fibrous connective tissue is far less metabolically active. Blood flow into capillary networks -Is regulated by smooth muscle cells called precapillary sphincters, found at the beginning of each network. Precapillary sphincters constrict or dilate depending on the needs of the tissues. Because there is not enough blood in the body to fill all of the capillaries, precapillary sphincters are usually slightly constricted. -In an active tissue that requires more oxygen, such as exercising muscle, the precapillary sphincters dilate to increase blood flow. These automatic responses ensure that blood, the volume of which is constant, will circulate where it is needed most. -Some organs have another type of capillary called sinusoids, which are larger and more permeable than are other capillaries. Sinusoids are found in the red bone marrow and spleen, where blood cells enter or leave the blood, and in organs such as the liver and pituitary gland, which produce and secrete proteins into the blood. EXCHANGES IN CAPILLARIES Capillaries are the sites of exchanges of materials . Some of these substances move from the blood to tissue fluid, and others move from tissue fluid to the blood. They move by diffusion, that is, from their area of greater concentration to their area of lesser concentration. Oxygen, therefore, diffuses from the blood in systemic capillaries to the tissue fluid, and carbon dioxide diffuses from tissue fluid to the blood to be brought to the lungs and exhaled. Blood pressure here(the pushing power) is about 30 to 35 mmHg, and the pressure of the surrounding tissue fluid is much lower, about 2 mmHg. Because the capillary blood pressure is higher, the process of filtration occurs, which forces plasma contents (except cells and albumin) out of the capillaries and into tissue fluid. Arrows shows the direction of movement. Filtration takes place at the arterial end of the capillary. Osmosis takes place at the venous end. Blood pressure decreases as blood reaches the venous end of capillaries, to become 15mmHg . Albumin contributes to the osmotic pressure of blood; this is an “attracting” pressure, or “pulling” rather than a “pushing” pressure and constant all through the capillary which is about 25mmHg. At the arterial end of capillaries, the pulling power of albumin is less than pushing power of blood pressure so plasma goes out the capillaries.Blood pressure at the venous end is less than osmotic pressure so fluid comes back to circulation. Pathways of Circulation Pulmonary circulation: Right ventricle pulmonary artery pulmonary capillaries (exchange of gases) pulmonary veins left atrium . Systemic circulation: Left ventricle aorta capillaries in body tissues superior and inferior caval veins right atrium. Hepatic portal circulation: Blood from the digestive organs and spleen flows through the portal vein to the liver where it divides into capillaries then it joins into hepatic vein before returning to the heart. The purpose is that the liver stores some nutrients or regulates their blood levels and detoxifies potential poisons before blood enters the rest of peripheral circulation. FETAL CIRCULATION The fetus depends upon the mother for oxygen and nutrients and for the removal of carbon dioxide and wastes. • Because the fetal lungs are deflated and do not provide for gas exchange, blood is shunted away from the lungs. The foramen ovale is an opening in the interatrial septum that permits some blood to flow from the right atrium to the left atrium. The blood that does enter the right ventricle is pumped into the pulmonary artery. • The ductus arteriosus is a short vessel that diverts most of the blood in the pulmonary artery to the aorta, to the body. Both the foramen ovale and the ductus arteriosus permit blood to bypass the fetal lungs . • Just after birth, the baby breathes and expands its lungs, which pulls more blood into the pulmonary circulation. • More blood then returns to the left atrium,and a flap on the left side of the foramen ovale is closed. The ductus arteriosus constricts, probably in response to the higher oxygen content of the blood. BLOOD PRESSURE Blood pressure is the force the blood exerts against the walls of the blood vessels . -The dynamics of blood flow in blood vessels is similar to any fluid driven by a pump and the nearer the fluid is to the pump, the greater the pressure exerted on the fluid. The blood flows through the blood vessels along a pressure gradient always moving from higherto lower-pressure areas. -Systemic blood pressure is highest in the aorta and declines throughout the pathway to finally reach 0 mm Hg in the right atrium. -The steepest drop in blood pressure occurs in the arterioles, which offer the greatest resistance to blood flow. Blood pressure in various blood vessels of the systemic circulation. Quest ion: In which class of blood vessels does the greatest drop in blood pressure occur? Answer: Arterioles, because this is the site of greatest resistance. Arterioles control the distribution of blood to the tissues by changing their resistance. Arterial blood pressure Reflects two factors: (1) how much the elastic arteries close to the heart can be stretched, and (2) the volume of blood forced into them. If the amounts of blood entering and leaving the elastic arteries in a given period were equal, arterial pressure would be constant. Instead, blood pressure rises and falls in a regular fashion in the elastic arteries near the heart.As the left ventricle contracts and expels blood into the aorta, it stretches the elastic aorta and large arteries. This pressure peak, called the systolic pressure, averages 120 mm Hg in healthy adults. • Blood moves forward into the arterial bed because the pressure in the aorta is higher than the pressure in the more distal vessels. • During diastole, the aortic valve closes, preventing blood from flowing back into the heart, and the walls of the aorta (and other elastic arteries) recoil, maintaining sufficient pressure to keep the blood flowing forward into the smaller vessels. During this time, aortic pressure drops to its lowest level (approximately 70 to 80 mm Hg in healthy adults), called the diastolic pressure. • The difference between the systolic and diastolic pressures is called the pulse pressure. It is felt as a throbbing pulsation in an artery (pulse) during systole, as the elastic arteries are expanded by the blood being forced into them by ventricular contraction. • Increased stroke volume and faster blood ejection from the heart (a result of increased contractility) cause temporary increases in the pulse pressure. Factors that increase BP 1-increased stroke volume. 2-increased heart rate. 3-increased blood viscosity . 4-increased peripheral resistance • Peripheral resistance: is the friction force created between the blood and the walls of the blood vessels which hinders blood flow. • Viscosity: The greater the viscosity the greater the resistance to flowing. The presence of blood cells and plasma proteins increases the viscosity of the blood hence the greater the force is needed to move it in the vascular system. • Therefore, the BP rises as the blood viscosity increases and drops as viscosity decreases. • Hypertension is a resting systemic pressure above the normal range. Clinicians now consider: • from125 to 139/85 to 89 mmHg to be pre-hypertension. • A systolic reading of 140 to 159 mmHg or a diastolic reading of 90 to 99 mmHg may be called stage 1 hypertension, and a systolic reading above 160 mmHg or a diastolic reading above 100 mmHg may be called stage 2 hypertension. • The term “primary or essential hypertension” means that no specific cause can be determined; most cases are in this category. For some people, however, the cause of their hypertension is known ,it is called secondary hypertension. • Although hypertension often produces no symptoms, the long-term consequences may be very serious on the heart and may be fatal(silent killer). • Although the walls of arteries are strong, hypertension weakens them and arteries may rupture or develop aneurysms, which may in turn lead to a cerebro-vascular accident (CVA) or kidney damage. • Hypertension let the left ventricle works harder and, like any other muscle, enlarges as more work is demanded; this is called left ventricular hypertrophy. • This abnormal growth of the myocardium, however, is not accompanied by a corresponding growth in coronary capillaries, and the blood supply of the left ventricle may not be adequate for all situations. • Exercise, for example, puts further demands on the heart, and the person may experience angina due to a lack of oxygen or a myocardial infarction if there is a severe oxygen deficiency. • Although several different kinds of medications (diuretics, vasodilators) are used to treat hypertension, people with moderate hypertension may limit their dependence on medications by following certain guidelines: • Don’t smoke, because nicotine stimulates vasoconstriction, which raises BP. Smoking also damages arteries, contributing to arteriosclerosis. • Lose weight if overweight. A weight loss of as little as 10 pounds can lower BP. A diet high in fruits and vegetables may, for some people, contribute to lower BP. Saturated fat, and cholesterol increase the possibilities of hypertension. • Cut salt intake in half. Although salt consumption may not be the cause of hypertension, reducing salt intake may help lower blood pressure by decreasing blood volume. • Exercise on a regular basis. A moderate amount of aerobic exercise (such as a half hour walk every day) is beneficial for the entire cardiovascular system and may also contribute to weight loss. • Avoid Stress • Secondary hypertension, which accounts for 10% of cases, is due to identifiable disorders, such as obstruction of the renal arteries, kidney disease, arteriosclerosis, and endocrine disorders such as hyperthyroidism and Cushing’s disease. Treatment for secondary hypertension is directed toward correcting the causative problem. • The rennin and angiotensin mechanism 1. Decreased blood pressure stimulates the kidneys to secrete renin. 2. Renin splits the plasma protein angiotensinogen (synthesized by the liver) to angiotensin I. 3. Angiotensin I is converted to angiotensin II by an enzyme (called converting enzyme) secreted by lung tissue and vascular endothelium. 4. Angiotensin II: -causes vasoconstriction -stimulates the adrenal cortex to secrete aldosterone • Hypotension is a systolic pressure below 100 mm Hg. Low blood pressure is often associated with old age free of cardiovascular illness. • Elderly people are prone to orthostatic hypotension— temporary low blood pressure and dizziness when they rise suddenly. Because the aging sympathetic nervous system blood pools briefly in the lower limbs, reducing blood delivery to the brain. Making postural changes slowly usually prevents this problem. • Chronic hypotension may indicate poor nutrition because poorly nourished people are often anemic and have inadequate levels of blood proteins so blood viscosity is low. Chronic hypotension also warns of Addison’s disease (inadequate adrenal cortex function), hypothyroidism, or severe tissue wasting. • Acute hypotension is one of the most important signs of circulatory shock and a threat to patients undergoing surgery and those in intensive care units. 1. 2. 3. 4. Developmental Aspects of Blood Vessels The fetal vasculature is functioning in blood delivery by the fourth week. Fetal circulation differs from circulation after birth. The pulmonary and hepatic shunts and special umbilical vessels are normally occluded shortly after birth. Blood pressure is low in infants and rises to adult values. vascular problems include varicose veins, hypertension, and atherosclerosis. Hypertension is the most important cause of sudden cardiovascular death in middle-aged men. Atherosclerosis is the most important cause of cardiovascular disease in the aged. AGING AND THE VASCULAR SYSTEM • It is believed that the aging of blood vessels, especially arteries, begins in childhood, although the effects are not apparent for decades. • The cholesterol deposits of atherosclerosis are to be expected with advancing age, with the most serious consequences in the coronary arteries. • The veins also deteriorate with age; their thin walls weaken and stretch, making their valves incompetent. This is most likely to occur in the veins of the legs; their walls are subject to great pressure as blood is returned to the heart against the force of gravity. Varicose veins and phlebitis are more likely to occur among elderly people. HOMEOSTATIC IMBALANCE • Each year about 30,000 infants are born in the U.S. with one or more of 30 different congenital heart defects, making them the most common of all birth defects. • Most congenital heart problems are traceable to environmental influences, such as maternal infection or drug intake during month 2 when the major events of heart formation occur. • The most prevalent abnormalities produce two basic kinds of disorders in the newborn. They either : (1) lead to mixing of oxygen-poor systemic blood with oxygenated pulmonary blood (so that inadequately oxygenated blood reaches the body tissues) as septal defects and patent ductus arteriosis. (2) involve narrowed valves or vessels that greatly increase the workload on the heart as coarctation of the aorta . Modern surgical techniques can correct most of these heart defects.